The current approach to the treatment of neurogenic tumors varies depending on the location of the tumor, its size and the potential risks of the chosen method. Treatment of tumors of the sacral region is a complex surgical task due to the fact that in most cases combined anteroposterior approaches are required. With this approach, there is a high risk of damage to blood vessels, nerve structures or the wall of the rectum, which are always intimately adjacent to the tumor capsule.
Neurogenic tumors are extremely rarely localized in the pelvic area. Thus, T. Rasmussen et al. [1] found only 35 (7%) cases of neurogenic sacral tumor among 557 patients with spinal tumors. Database analysis confirms that for every 40,000 patients with spinal tumors, there is only one with a neurogenic sacral tumor. Most patients with neurogenic tumors of the sacral location have neurofibromatosis [2].
As a rule, the manifestation of the disease occurs in the case of progression of the tumor process. This may be accompanied only by local or radicular pain, less often by dysfunction of the pelvic organs. The appearance of symptoms always indicates the beginning of progressive tumor growth, and in cases where a large tumor is detected, its malignancy should be suspected [3-5]. Neurogenic tumors rarely infiltrate bone tissue. Even in the case of malignant transformation, local growth is often expansive, however, this often leads to the destruction of bone tissue. Considering the possibility of malignant transformation of a neurogenic tumor, even small tumors of a neurogenic nature should be radically removed [6].
One of the treatment options for a neurogenic tumor of the sacrum, in the absence of significant symptoms, is stereotactic radiation therapy [7–10].
The approach to a neurogenic tumor of the sacrum is selected depending on the location of the tumor, its size and adjacent structures.
Thus, according to the findings of P. Klimo et al. [11], all neurogenic tumors of the sacrum can be divided into three types (Fig. 1).
Rice. 1. Classification of neurogenic tumors of the sacrum by type of growth. Type I - intracanal tumor growth; Type II - anteroposterior type of growth with expansion into the pelvic area and growth of the sacral tire; Type III - anterior type of growth, mainly towards the pelvis.
The authors suggest a specific approach for each type of tumor growth: for type I tumors, in their opinion, a posterior approach can be used; for type II tumors - a combined anteroposterior approach or only a posterior approach; for type III tumors, it is advisable to use a combined posteroanterior approach, which involves isolating the source of tumor growth - the nerve root of the sacral localization and intersection in the area of its healthy part, followed by foraminal dissection of its cuff to facilitate isolation tumors via anterior approach. Then the tumor is removed using an anterior retro- or transperitoneal approach.
Our article presents a case of removal of a type II tumor. Radical resection was achieved by amputation of the sacrum below the S1 body only from the posterior approach.
Clinical case
Patient P
., 23 years old, applied to the Neurosurgery Center named after. N.N. Burdenko in 2015 with complaints of severe local pain in the sacral region, in the perineum and impaired sensitivity in the anogenital zone. MRI/MSCT (spiral computed tomography) revealed a sacral tumor with a cystic component and bone destruction at the S1-S5 level (Fig. 2).
Rice.
2. MRI of the sacrum, T1-weighted image in the sagittal projection (arrow marks the tumor). Given the complex configuration of the tumor and destruction of bone tissue, the diagnosis was questioned. Therefore, the first stage was a diagnostic puncture CT biopsy of the tumor under the control of a navigation system. During pathomorphological examination of the biopsy specimen, a diagnosis was made: neuroma.
Considering the dynamic MRI data of the sacral region - an increase in tumor size, as well as the absence of gross neurological symptoms, in order to preserve the function of the pelvic organs, it was decided to perform radiation therapy instead of radical resection. Stereotactic hypofractionated radiation therapy was performed using the Cyber-Knife device (bremsstrahlung photon radiation from electrons 6 MeV). The tumor volume is 90 cm3. The average single focal dose is 5.2 Gy, the average focal dose is 26 Gy.
The observation period was 24 months. During this time, there were no significant changes in the neurological status; on the contrary, 3 months after radiation therapy, the pain syndrome regressed. However, in 2017, the patient again noted the appearance of local pain. The appearance of rectal bleeding, which was not associated with hemorrhoidal lesions of the veins, was also alarming. Sigmoidoscopy revealed no erosions, cracks, ulcerations or tumor penetration of the intestinal wall. At the same time, given the amount of non-steroidal anti-inflammatory drugs used, this bleeding could be an expected complication. According to control MRI/SCT studies of the lumbosacral region with contrast enhancement, continued tumor growth was determined at the S1-S5 level (Fig. 3).
Rice. 3. Continued growth of the sacral tumor after stereotactic radiation therapy. a — SCT of the lumbosacral region in the sagittal projection; b — 3D image constructed from computed tomography, median section in sagittal projection; c — SCT of the sacrum in the axial projection.
The patient was offered surgical treatment. Taking into account previous radiation therapy and the nature of tumor growth, radical tumor removal with simultaneous lumbopelvic trans-S2 stabilization and pelvic floor plastic surgery was planned. Stabilization was considered due to the possibility of postoperative stress fracture of the remnant sacrum and instability.
Operation stages
Position the patient on her stomach. The incision is linear, along the spinous processes and slightly lateral to the intergluteal fold (Fig. 4).
Rice. 4. Position of the patient on the operating table and marking of the future incision. a - schematic representation of the patient’s position on the table, the position changes before stabilization. The frame is lowered to create maximum lordosis; b - schematic representation of the projection of a linear section. The dotted line marks the area of skeletonization of the pelvic bones; c — intraoperative photo: a marker shows the dotted line of the incision.
The sacrum is skeletonized, it is noted that the sacral covering is destroyed in the S2-S3 zone (Fig. 5).
Rice. 5. Intraoperative photo. Skeletonized sacrum. A reference frame was installed on the spinous process before the laminectomy stage.
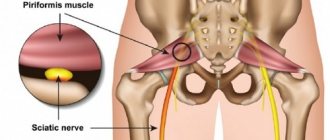
A laminectomy of S1 was performed, the roots below S2, which were part of the tumor parenchyma, were ligated, a cut was made to the healthy bone of the sacrum below the S1 vertebra, the sacrotuberous and coccygeal-tuberous ligaments, piriformis were crossed, then the presacral fascia was disconnected from the rectal wall, the nerves of the sacral plexus were crossed at peripheral segment (Fig. 6).
Rice. 6. Intraoperative photo. a — laminectomy was performed (arrow indicates tumor tissue); b — the sacral ligaments are crossed, the sacrum is elevated to disconnect the rectal wall from the presacral fascia.
The tumor along with the sacrum was removed en bloc. Transpedicular stabilization of L5—S1 and lumbopelvic stabilization through the lateral masses of the sacrum at the S2 level were performed (Fig. 7).
Rice. 7. Intraoperative photos. a — bed of the removed tumor, free S2 roots are visible (shown by white arrows); b — type of installed lumbopelvic stabilizing system; c — pelvic floor plastic surgery was performed with polypropylene material, the area of the ligated roots was additionally covered with plastic material; d — block of the tumor removed from the sacrum in the anteroposterior and lateral projections; d — intraoperative 3D reconstruction of radiographs. Type of stabilizing structure.
The last stage was soft tissue plastic surgery by suturing free muscle flaps of the gluteal muscles, the skin was sutured with an intradermal suture (Fig. 8).
Rice. 8. Schematic representation of the selection of free flaps of the gluteus maximus muscles (a, b) and the appearance of the wound after healing (c).
In the postoperative period, the patient was activated on the 1st day after surgery. The wound discharge was drained for 5 days.
On the control MRI there are no signs of a tumor, signs of a serous cavity, perineal hernia or other complications (Fig. 9).
Rice. 9. MRI of the lumbosacral spine in 3 projections 2 months after surgery. a — sagittal projection; b - frontal projection; c — axial projection.
Urological rehabilitation was carried out for 3 months after the operation: electrical stimulation of the bladder, periodic catheterization, physical therapy, and taking cholinomimetics. After 3 months, there was a decrease in the amount of residual urine to 20-50 ml, no episodes of urinary retention or incontinence, and normal bowel movements. The only manifestation of discomfort was a violation of sensitivity in the anal area in the form of superficial hypoesthesia.
Types of disease
Neuroma is divided into two types - benign and malignant. Benign is a slowly growing node that does not cause disruptions or disturbances in the functioning of the body. Location: head, spine, neck.
Malignant neuroma is the result of the transition of a benign tumor to a malignant sarcoma of the nerve. It is difficult to define and establish clear boundaries of the disease. The node grows quickly, and metastases may develop in other organs. The tumor can reach large sizes; the larger, the more difficult it is to treat. Location: forearms, feet, hands. Take into account! The malignant form is typical for people aged 20 to 40 years, and the benign stage is typical for people aged 50 to 60 years. The clinical symptoms of both forms are similar, which complicates the situation; the doctor needs to clearly understand what stage the disease belongs to.
The following types of neuroma are also distinguished:
- tumor of the thoracic and cervical regions. The disease affects the spine, when the tumor grows through the intervertebral spaces, a schwannoma of the neck begins to develop;
- Morton's neuroma. The tumor affects the foot, touching the nerve endings. In the affected area, both one and both limbs often grow between the fingers;
- a brain tumor. Slow development, the tumor is limited to neighboring tissues;
- acoustic schwannoma. Localization - right or left ear, slow development.
The disease can affect the trigeminal nerve and can develop in the lower leg area, between the right and left pleural cavities.
Discussion and conclusions
Various tumors occur in the sacral area, most often primary bone tumors: chordoma, giant cell tumor. Neurogenic tumors make up only a small proportion of neoplasms found in the sacral region. Moreover, the behavior of these tumors, as a rule, is characterized by an aggressive growth pattern and frequent malignant transformation of tumor tissue [12–14]. Malignancy more often occurs in cases of prolonged growth of xanthomatous neurofibroma. A tumor biopsy sometimes provides little information, since during puncture the surgeon aims at the most massive part of the tumor, and the material taken does not always contain the degenerated part.
In the described case, the choice of the type of resection was dictated by the fact that the tumor completely destroyed the sacrum in the S2-S5 zone, in addition, the risk of malignancy was especially significant after radiation preceding the continued growth of the tumor.
Literature data [9, 10] provide cases of the formation of secondary tumors or malignancy of benign tumors after conventional radiation therapy. Therefore, most authors consider radiation therapy to be a risky treatment.
However, current practice shows that radiosurgery or hypofractionated high-dose radiation therapy is an alternative to surgical methods for treating patients with neurogenic tumors in the spine [7, 8]. However, most publications present single observations or analysis of treatment in small series of patients. Therefore, it is extremely difficult to predict the outcome of treatment. In our observation, according to MRI data, after irradiation there was an increase in tumor volume, with pain, as well as a risk of tumor malignancy. All this became the basis for the decision to undergo surgical treatment.
Various aspects of surgical treatment are quite well described in the literature. J. Feldenzer et al. [15] operated on 9 patients. Two of them underwent combined tumor removal from an anteroposterior approach, the rest were operated on only from a posterior approach. At the same time, 2 patients from the posterior approach group had malignant tumors of the peripheral nerves and died during 3 years of observation; the rest had no signs of tumor recurrence. J. Domínguez et al. [16] describe in their publication 6 patients with giant sacral schwannomas. Two underwent an anteroposterior approach to remove the tumor; the rest underwent a posterior approach. Tumor recurrence was observed in 3 patients with an intradural component of the tumor, and in 1 patient the recurrence occurred 17 years after surgery. In a series of observations by C. Abernathey et al. [17] 10 patients were operated on only from the posterior approach, 3 patients - from the anterior approach. In 4 patients, removal of the intrathecal component of the tumor was required. Total removal was noted by the authors in 4 cases. Nine patients who underwent partial tumor resection were asymptomatic during the entire follow-up period, but 4 (44%) patients required reoperation. All of these 4 patients had no signs of continued tumor growth or malignancy during 7–84 months of follow-up. During their treatment, an additional anterior approach was used to remove the tumor in 3 cases, and a combined anteroposterior approach was used in 1 case. One patient required additional pelvic stabilization, but the authors did not indicate the reasons for this. Complications included dysfunction of the pelvic organs in 1 patient, sensory disturbances in the anogenital area in 4 patients, motor disorders and problems with movement in 1 patient. Wound complications were described in 3 patients.
In modern specialized literature, there are no examples of sacral amputation or total sacrectomy in the treatment of patients with potentially benign or potentially malignant sacral tumors, since sacrectomy is considered the method of choice for the treatment of patients with locally aggressive or completely malignant, mainly bone, sacral tumors.
In the case we described, partial resection of the tumor did not make sense and would have led to tumor recurrence. In addition, the S3-S5 roots passed through the tumor parenchyma, so the decision to en bloc resection of the sacral tumor was justified.
An interesting fact is that in the postoperative period the patient experienced only transient dysfunction of the pelvic organs. This was due to the preservation of the anatomical integrity of the S2 roots on both sides. According to the literature, the preservation of the S2 roots is the key to preserving the function of the bladder sphincter, while the preservation of the normal act of defecation depends on many factors, in particular on the preservation of normal pelvic floor function and the preservation of the sensitivity of filling and emptying of the rectal ampulla.
J. Wilfrid [18] uses data from O. Foerster et al., who described back in 1927 the multiplicity of options for the innervation of the pelvic organs, which makes possible the reinnervation of the pelvic organs and determines positive dynamics as a result of rehabilitation (see table).
Variants of innervation of the pelvic organs according to O. Foerster et al. (1927)
Another important problem that often complicates the postoperative course in the area of sacral resection is instability in the sacroiliac joint. Typically, instability develops as a result of resection of more than 50% of the sacroiliac joint or due to osteoporosis or prolonged excessive load and requires additional stabilization and restoration of continuity of the pelvic ring [19].
Following all precautions and taking into account world experience, we completed the operation with lumbopelvic stabilization.
Causes of the disease and main symptoms
If a doctor has diagnosed a neuroma of the auditory nerve, spine, or brain, this does not mean that the disease was affected by another disease. This puts specialists in a difficult position, since it is difficult to establish the exact cause of the disease; it develops in healthy people.
The cause of the development of nerve tumors can be influenced by genetic diseases, among which are:
- schwannomatosis;
- neurofibromatosis (type 1,2);
- Gorlin-Goltz syndrome.
If a person has a genetic predisposition and close relatives had malignant tumors, then this can also be a reason. It is necessary to highlight frequent injuries and exposure to ionizing radiation.
Among the common symptoms of neuroma are:
- palpable formation (located above the skin);
- pain (severe pain when pressing).
Nerve swelling has visible and invisible signs. If a nerve located deep in the tissue is affected, there will be no signs. Otherwise, a dense formation appears above the skin.
Nerve swelling may not bother you for several months or years, but this does not mean that the disease does not progress. There are symptoms depending on the location of the disease.
Acoustic neuroma
The main symptoms of acoustic neuroma include:
- frequent ringing in the ears;
- hearing impairment;
- dizziness (especially when turning your head);
- lack of balance (one side will seem heavier);
These symptoms can lead to the development of deafness. The disease is accompanied by nausea, vomiting, and pain.
Trigeminal nerve injury
Symptoms include:
- burning;
- severe pain;
- numbness in areas of the face (for example, in the eyebrows, chin, lips);
- atrophy of the masticatory muscles;
The patient may lose taste and increase salivation. Late stages of development are characterized by intracranial pressure.
Spinal neuroma
The following symptoms are typical for spinal neuroma:
- pain in the back;
- pain in arms, legs;
- numbness of legs, arms;
- pain in the lumbar region;
The patient complains of intestinal problems, difficulty urinating, for example, there may be incontinence, the disease can lead to paralysis of the legs.
Pulmonary neuroma
Symptoms:
- increased cough;
- pain during inhalation/exhalation;
- the appearance of frequent shortness of breath.
Cervical neuroma
Among the main symptoms are:
- pain while swallowing;
- the tongue will begin to go numb;
- swelling will appear on the neck;
Also characteristic is pain in the neck area, radiating to the shoulders.
Symptoms
Neuroma has a whole list of symptoms characteristic of this tumor that need to be paid attention to.
The symptoms of the tumor are as follows:
- radicular pain syndrome. Everything will depend on which root was injured: if the anterior roots are damaged, partial paralysis may develop, if the posterior roots are affected, sensitivity may be impaired or severe pain may occur.
- noticeable disruption of the pelvic organs
- severe pain in the stomach area that does not stop after a standard dose of pain medication
- erectile dysfunction that occurs repeatedly and is not associated with fatigue or other factors
- bradycardia
- disturbance or absence of normal functions of defecation and urination
Treatment of neuroma
Treatment of neuroma depends on the stage and form of the disease - benign or malignant.
Surgical intervention
Neuroma of the brain, auditory nerve, or spine in complex forms is treated with surgical intervention. If this benign formation is small in size and does not cause discomfort, then the neuroma may not be removed. If this is a malignant form, then surgery is a mandatory procedure.
Radiosurgery
Removal of a neuroma using radiosurgery involves exposure to the source of the disease using radioactive radiation. This is a painless procedure lasting no more than an hour.
Chemotherapy and radiation therapy
Used after surgical removal of a neuroma, it allows you to get rid of the remnants of the disease. The treatment regimen for each client is selected individually.
A comment
The article, presented by a team of authors, raises one of the most complex topics in modern spinal neurosurgery and neurosurgery in general - the diagnosis and treatment of neurogenic tumors of the sacral region. Diagnosis of this group of diseases is a difficult task even for an experienced specialist due to the blurred clinical picture in the early stages of the disease. The authors emphasize the technical complexity and high morbidity of surgical treatment of tumors in the sacral region due to the close proximity of many vital anatomical structures - large vessels, nerves and pelvic organs. The article presents a case of successful surgical treatment of this rare pathology, expresses the opinion of the authors and provides current literature data. The lack of scientific development of this topic leaves many unresolved issues that require additional scientific research, and this work is a contribution to the development of this important problem.
A.O. Guscha (Moscow)
Prognosis for treatment of malignant disease
Treatment of neuroma should be carried out regardless of stage and form. A benign form can develop into a malignant one, which will lead to the death of the patient. With a benign form, the five-year survival rate is 100%, with a malignant stage – from 37 to 65%. The tumor grows slowly; the location of the disease and the possibility of surgery are important. After removal, a neuroma can lead to loss of hearing, facial expressions, and some motor functions may fail. Surgery for neuroma in most cases does not have negative consequences, the patient is prescribed postoperative care and recovery.
conclusions
Radical resection of giant neurogenic tumors of the sacral region may possibly reduce the potential for local tumor recurrence and thereby prevent local malignancy and improve patient survival. Despite the high risk of neurological, wound, intraoperative complications, as well as possible lumbopelvic destabilization, en bloc tumor resection remains a justified treatment method. Restoring the lost quality of life as a result of surgical trauma is one of the most important tasks of future research to find opportunities for rehabilitation of pelvic functions in patients who have undergone various types of sacrectomy.
The authors declare no conflict of interest.
*e-mail: [email protected]
Diagnostic methods
The picture of the disease has many similarities with a wide range of pathologies leading to damage to the nerve trunk. The causes of such lesions are inflammatory processes, pressure, confusion of nerve pathways, and metabolic disorders. An experienced neurologist can differentiate the anomaly, who initially determines the extent of the damage occurring. Next, instrumental studies are prescribed to identify the cause of the disease. The main ways are:
- Computer tomogram of the head brain. Most often, this diagnosis is made using a contrast agent. Enhancing staining allows tumors larger than one centimeter to be seen on photographs.
- Magnetic resonance scanning. Examination of the intracranial area makes it possible to assess the condition of not only the neoplasm, but also the surrounding tissues associated with it. If areas of the back are affected, targeted tomography of the roots is performed. In MRI images, the level of compression of the abnormal zone is clearly visible.
- Audiometry. It allows not only to determine the degree of hearing loss, but also to exclude other sources of its development.
- Tomographic screening of the larynx. It is used as a clarifying technique to determine the size and location of an object.
- Ultrasound examination of soft tissues of the extremities. Well visualizes thickening of the membrane of the neural column.
- Electroneuromyography. Helps assess nerve functionality. Often used after instrumental intervention to monitor recovery.
- Histology. It is carried out after instrumental removal of the tumor in order to study its structure and benignity.