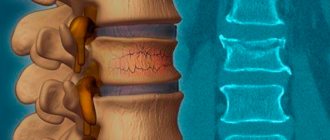
Transpedicular fixation (TPF) is a fundamentally new method of spinal fixation developed in the 60-70s. Transpedicular fixation is an operation whose essence is to stabilize the vertebra by inserting screws through the pedicles (pedicles) into the vertebral body. The technique allows for tight, secure fixation of the screw in the vertebral body and is one of the most common types of treatment for traumatic injuries and chronic diseases of the spine. Indications for surgical treatment include unstable vertebral fractures, scoliotic deformities of the spine, osteochondrosis and some other diseases.
Key features of screw installation: strength at the bone-metal interface , avoidance of damage to nerve , vascular structures , and facet joints . The screws are installed using the convergent monocortical technique with the selection of the maximum allowable sizes. In order to determine the entry point into the root of the arch, anatomical landmarks are used: the transverse and articular processes. The hole for the screw is prepared using an awl or probe. X-ray control is carried out. Monoaxial or polyaxial types of screws are used.
Properly performed fixation ensures a high incidence of spinal fusion (onset of bone fusion), reduces the time of hospital treatment and disability, and ensures a qualitatively higher level of rehabilitation, combined with the possibility of early activation of the patient.
The advantages of TPF are the low invasiveness of the intervention and the possibility of reliable stabilization of the spinal motion segment.
And, although the concept of transpedicular fixation of the spine is not new, this technique has developed particularly rapidly over the past two decades. The technique of installing metal structures, indications, contraindications, complications and long-term results have been deeply and comprehensively studied and described in detail in the literature.
Today, the transpedicular fixation technique is widely used by vertebrologists for surgical treatment of the entire spectrum of diseases and injuries of the spine. The use of internal fixation is well justified in the correction of deformities, especially scoliosis. The advantages of transpedicular fixation over previous methods in the treatment of spinal fractures have been sufficiently substantiated (closure of only a short segment, reposition and fixation with one structure, stability of fixation, which allows early mobilization of the patient without external immobilization). And if 10 years ago there were discussions about the relationship between the risk and effectiveness of transpedicular fixation for degenerative diseases of the spine, including osteochondrosis, today indications have been formulated and it has been clearly shown that the cause of complications is most often incorrect surgical technique.
The “gold standard” for surgical treatment of osteochondrosis with instability of the lumbar spine was rigid fixation of the operated segment in combination with interbody corporodesis with a cage. Positive results from spinal fusion range from 90 to 95% across different investigators, with an average of about 79% based on a review of the literature.
The increase in the frequency of use of metal structures is closely related to the popularity among surgeons of 360-degree spinal fusion (a combination of interbody and transpedicular fusion. This operation is considered as the most optimal way to achieve stability of the operated segment. With interbody fusion, a higher frequency of bone fusions is observed than with posterior fusion. The disadvantage of posterior stabilization is residual micromobility in the anterior parts of the spinal motion segment, which can provoke lumbar pain syndrome.The use of cages allows you to avoid this.
Modern interbody implants must meet the following requirements:
- ensure stability of the vertebral bodies
- maintain intervertebral disc height to prevent compression of nerve structures
- contain bone material to achieve bone fusion (for example, bone chips or synthetic material with a bone-stimulating effect)
- restoration and preservation of the frontal and sagittal balance of the spine
- withstand the axial load of the spine, especially during the period of graft reconstruction
Transpedicular fixation of the lumbar spine
Transpedicular spinal fixation (hereinafter referred to as TSF) is one of the most common operations in modern neurosurgery. It is used for various diseases and injuries: degenerative-dystrophic diseases of the spine (spinal stenosis, spondylolisthesis - degenerative and spondylolysis, instability); spinal injuries, inflammatory diseases - spondylitis and spondylodiscitis; primary and secondary tumors of the spine.
Transpedicular fixation of the spine can be multi-level (fix several spinal motion segments of the spine) or fix only one segment.
It can be dynamic , when there is slight mobility in the facet joints after installation of the system, which slows down the progression of spondyloarthrosis and, as a result, pain and rigidity , when any micromobility is excluded.
According to the installation method - TPF for “open” operations, when wide access to the spinal structures is provided and the system is installed using external anatomical landmarks and additional x-ray control, PERCUTANARY TPF - systems, when several small incisions are made in the projection of screw insertion, the integrity of the multifidus muscles is preserved , the risk of suppuration and blood loss associated with access is significantly reduced. This operation is under X-ray guidance and is classified as minimally invasive spine surgery (MIS).
360 degree locking
Fixation at 270 degrees - using only 2 screws on one side (where the facet joint was removed and an interbody cage (so-called TLIF) was installed)
MRI before surgery
X-ray after surgery
X-ray of postoperative percutaneous TPF in a patient with multiple vertebral fractures
When to use
Indications for transpedicular fixation of the spine include the following pathologies and mechanical damage:
- violation of integrity, fracture-dislocations and serious contusions of the vertebrae in the lumbosacral and thoracic region;
- deformation of the spinal column structures;
- severe disc displacement leading to spinal instability;
Direct indications for surgery in the above cases are pain, as well as a significant risk of dysfunction of the entire musculoskeletal system and immobilization of the patient. If we talk about contraindications, the use of TPP is prohibited in the following cases:
- pregnancy;
- high BMI (obesity);
- individual intolerance to titanium;
- infectious lesions of the area of the back that will undergo surgery;
- advanced forms of osteoporosis.
For fractures and pathological processes in the cervical spine, transpedicular fixation is not used due to the small vertebral arches, which do not allow the screws to be properly secured.
Rehabilitation after transpedicular fixation (TPF)
It is clear that recovery after TPF surgery on the spine will depend on the disease or injury for which treatment is being performed, the type of intervention and its traumatic nature. All other things being equal, less traumatic and minimally invasive operations help to rehabilitate the patient faster. Spinal surgeries, especially in cases of uncomplicated uncomplicated trauma (type A fracture, for example), are designed to help get the patient back on his feet and able to work as soon as possible, make him independent from outside help, and avoid complications associated with prolonged bed rest - bedsores, thrombotic complications, pneumonia etc. Until the early 90s of the last century, the most common type of treatment and rehabilitation of patients with a spinal fracture was the functional Gorinevskaya-Drevig method, which required long-term bed rest with gradual reclination of the compressed vertebra. Currently, thanks to the introduction of TPF, this process has been significantly simplified and reduced in time.
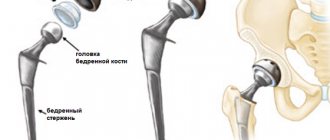
Features and essence of the method
The transpedicular spinal fixation system is based on the introduction of titanium screws connecting broken vertebrae. This will allow restoration of motor function and healing of damaged segments. Previously, stainless alloys were used for such operations, but now titanium alloys are increasingly used. This will make it possible in the future to use magnetic resonance imaging devices to monitor the patient’s condition and assess the success of treatment.
Transpedicular fixators must meet the following requirements:
- Biological inertness of the material. The body should not reject the implant, which will ensure lifelong use. In addition, the material is selected taking into account the effects of the body's environment.
- Increased mechanical strength. Despite all the advantages of titanium, this material is quite fragile and therefore cannot withstand shock loads. Special alloys make it possible to achieve the necessary ductility and stability.
- MRI compatible. Diagnostics using an MRI machine will allow you to assess the condition of the implant, and is also often used for a general scan of the body. That is why, when installing a retainer, it is necessary to achieve not only an exceptional fit, but also create good visibility during examination.
- Convenient installation. Modern devices allow the implant to be inserted through small incisions in the skin, reducing the traumatic nature of this procedure. In addition, there are many types of screw fastening in three planes, which makes it possible to gradually restore damaged vertebrae.
- Additional features. These include the so-called cemented systems. They allow you to introduce a special solution to securely fix the screws. Such procedures are used for joint diseases (osteoporosis), when there is a high risk of the fixator becoming dislodged.
These clamps are designed to secure vertebrae in the thoracic and lumbar regions. For other situations, similar methods are used, but using other types of clamps.
Photo of transpedicular fixation of the spine
X-ray after surgery
Thus, the terms of rehabilitation depend on the disease for which surgery was performed, and the operation of transpedicular fixation helps to accelerate the rehabilitation process.
Author of the article: neurosurgeon Anton Viktorovich Vorobiev Frame around the text
Why choose us:
- we will offer the most optimal treatment method;
- we have extensive experience in treating major neurosurgical diseases;
- We have polite and attentive staff;
- Get qualified advice on your problem.
Drug treatment
After the intervention, everyone without exception is prescribed a course of antibiotic therapy, which will prevent the appearance of an infectious-purulent focus in the vertebral and paravertebral structures. Along with antibiotics, the patient is recommended to take anti-inflammatory and analgesic medications that relieve swelling, inflammation and pain at the site of the manipulation. To prevent thrombosis, drugs with anticoagulant properties are prescribed. Additionally, they may prescribe a vitamin-mineral complex and medications to strengthen osteochondral structures, for example, medications based on calcium, glucosamine and chondroitin.
Possible complications
The main disadvantage of FPT is that surgical intervention requires the surgeon to have appropriate skills and experience, and can also lead to serious unpleasant consequences, which include:
- damage to nerve fibers, elements of the circulatory system and the spinal cord due to improper fixation of screws;
- inflammatory and septic processes at the junction of screws with bone tissue;
- breakage of screws or their loss from bone tissue.
The most dangerous complication is fractures and screw damage, which usually occur 4-5 months after surgery, when the bones have not yet had time to fully heal. As a result, destabilization of the structure occurs, which threatens repeated deformation of the spine, the development of pain, and requires repeated surgery.
Contraindications
Spinal fusion cannot be performed if:
- severe diseases of the cardiovascular system;
- recent stroke or heart attack;
- acute infectious diseases;
- exacerbation of chronic diseases;
- formation of fistulas of unknown origin;
- blood clotting disorders;
- varicose veins.
Traditionally, surgical treatment is indicated only for patients aged 12 to 60 years. In other cases, the possibility of surgical intervention is considered by a group of specialists.
Disability after spinal surgery with metal structures
There is no need to immediately panic if the temperature rises in the early phase after the intervention, you feel a foreign object in the operated area, swelling and pain. All these early reactions are not always interpreted as complications, but for the most part are the body’s natural physiological response to surgical trauma. In the hospital, and after discharge, in the rehabilitation center, they will create an effective recovery program for you. Therapeutic measures will help strengthen nutrition, activate regenerative and reparative processes in the problem area, strengthen the muscular frame of the back, which will gradually lead you to the desired recovery.
Now let's talk about officially obtaining disability status. The mere fact of the presence of a metal structure in the spine does not indicate that the patient is entitled to a disability. A group can be assigned only under compelling circumstances, if serious postoperative complications have arisen that limit a person’s ability to work.
If the recovery is delayed or the consequences of surgery with a metal structure have developed, which were not resolved during the rehabilitation period, the patient is referred to MSE. Based on medical documentation (ultrasound, REG, MRI, etc.), medical and social examination bodies will assess the person’s health status and make a conclusion regarding the need to assign disability.
The attending physician must necessarily refer a person to undergo MSEC if the following problems exist:
- frequent and prolonged physical and neurological exacerbations that limit the patient in the social, domestic and professional spheres of life;
- the logical completion of the recovery process is greatly delayed;
- the patient developed cephalgic syndrome;
- critical movement disorders (paresis, paralysis), etc. appeared.
It is worth noting that during rehabilitation, each patient receives a sick leave certificate for temporary incapacity for work for an average of 4 months, and only after this time can one begin to deal with issues of group registration. We are talking about assigning lifelong disability (group 1) only if it is not possible to restore the lost functions, in other words, medicine is no longer powerless to do anything. Usually, people with unfavorable conditions are more often given group 3, less often the second; after recommission, it can be removed or transferred to a group that is more severe by the standards of the physical condition of the body.
Preparation
Transpedicular fixation (TFP) of the spine begins with the preparation stage. Before the procedure, patients undergo all necessary tests. After which the surgeon examines the spinal column. This step is necessary to select the correct screw size.
Taking into account the type of damage, the diameter and length of the titanium screws themselves are selected. If it is necessary to fix several areas, then a special frame is assembled. It is made of wire and serves as a template. Titanium screws are made from this frame.
During the intervention, several segments are subject to fixation. For these purposes, 4 to 6 screws are used. After preparation, the operation itself is carried out.
Indications for surgery
Transpedicular fixation (abbreviated as TPF) is a modern method of treating complex spinal injuries. The operation allows you to fix the vertebrae in the desired position, and thereby eliminate their displacement or other serious consequences. This type of manipulation is used both in the cervical, thoracic, and lumbar regions. Prescribed only if there are indications and there are no alternative treatments.
The main indications for this are:
- Spondylolisthesis (loss of one or several bone elements at once).
- Severe injuries or fractures of the spine.
- Narrowing of the lumen of the spinal canal.
- Classic and compression traumatic fractures, dislocations.
- Excessive mobility of the spinal column, instability.
- Degenerative or dystrophic processes in the spine that pose a threat to human life and health.
- Scoliosis stage 3-4, irreversible pathological changes in the spine.
- Pseudoarthrosis.
- Destruction of intervertebral discs.
- Pinched nerve endings.
The technique is relatively young, although it was developed back in the 50-60s. It is constantly being improved, which minimizes the likelihood of postoperative complications after the installation of fixators. It is carried out only after other treatment methods have not given the desired result.
What does the system itself consist of?
The entire system consists of special screws and stabilizers. All material is durable, multi-layered and consists of a single metal structure. The screws themselves have caps that prevent them from screwing together. The entire system is held together by springs and various mechanisms. There are several types of screws. The choice depends on the specific situation.
A prerequisite is stabilization of the entire screw system. This stage is carried out at the end of the operation. Allows you to reduce the likelihood of system displacement.
When to use
Indications for transpedicular fixation of the spine include the following pathologies and mechanical damage:
- violation of integrity, fracture-dislocations and serious contusions of the vertebrae in the lumbosacral and thoracic region;
- deformation of the spinal column structures;
- severe disc displacement leading to spinal instability;
Direct indications for surgery in the above cases are pain, as well as a significant risk of dysfunction of the entire musculoskeletal system and immobilization of the patient. If we talk about contraindications, the use of TPP is prohibited in the following cases:
- pregnancy;
- high BMI (obesity);
- individual intolerance to titanium;
- infectious lesions of the area of the back that will undergo surgery;
- advanced forms of osteoporosis.
For fractures and pathological processes in the cervical spine, transpedicular fixation is not used due to the small vertebral arches, which do not allow the screws to be properly secured.