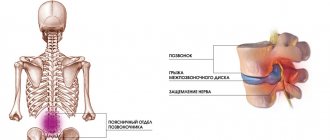
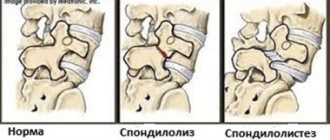
Spondylolisthesis (spon + dee + lo + lis + thee + sis) is a spinal pathology in which one of the vertebrae slips forward or backward in relation to the adjacent vertebra. Slipping of the upper vertebra forward relative to the underlying one is called anterolisthesis, and slipping backward is called retrolisthesis.
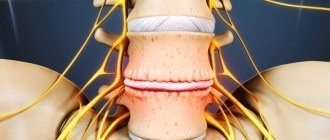
Spondylolisthesis (vertebral displacement) can lead to spinal deformity, as well as narrowing of the spinal canal (central spinal stenosis) or compression of the exiting nerve roots (foraminal stenosis).
Spondylolisthesis most often occurs in the lower back (lumbar spine), but can also occur in the thoracic and cervical regions. Treatment for vertebral displacement will depend on the degree of disruption of the biomechanics of the spine and the effect on nearby nerve structures and can be either conservative or surgical.
Causes of spondylolisthesis (vertebral displacement)
Spondylolisthesis has several main causes. Doctors have developed a classification system based on the different causes of spondylolisthesis.
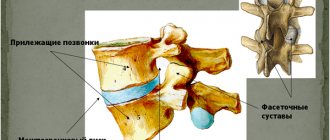
Type I: It is also called dysplastic or congenital spondylolisthesis. Thus, type I spondylolisthesis is a defect of the articular processes of the vertebra. This defect usually occurs at the junction of the lumbar spine and the sacrum: area L5-S1. The defect causes the L5 vertebra to slip forward relative to the sacrum.
Type II: Also called isthmic, this is the most common type of spondylolisthesis. In type II spondylolisthesis, there is a problem with the pars interarticularis, a specific area of the vertebra. . Isthmic spondylolisthesis is further divided into subtypes:
- Type II A: Gymnasts, weightlifters and football players are especially susceptible to this type of spondylolisthesis. This type of vertebral displacement is caused by multiple microdestructions in the pars interarticularis area, which arise due to hyperextension and excessive loads. The vertebral arches in type II A are completely broken.
- Type II B: This type is also caused by microfractures. The difference, however, is that the arms do not break completely. Instead, bone tissue grows and the arches become longer as they regenerate. Longer arches may force the vertebra to move forward.
- Type II C: Like Type II A, this type has a complete fracture and is caused by acute trauma. For example, an impact from a car accident can destroy the temples.
A fracture of the arch can lead to the appearance of a moving part of the bone; the disconnected inferior articular process may move. This bone fragment, also called a Gill fragment, can impinge on a nerve root and often requires surgical removal of the bone fragment.
Problems with the pars interarticularis can also be called spondylolysis. The word is similar to spondylolisthesis, and the two are somewhat related. Microdestructions in the pars interarticularis - often occur in gymnasts, football players and weightlifters - are a form of spondylolysis. Fractures of the arches are called spondylolysis; If a vertebra slips forward because it is not held in place properly, it is called spondylolisthesis.
Type III: Aging can also cause spondylolisthesis. As a person ages, degeneration of the spinal structures occurs. Usually, the intervertebral discs degrade first. The older a person is, the less water and proteoglycans there are in the discs - and this leads to a decrease in the shock-absorbing functions of the discs. The discs become thinner and the load on the facet joints increases. The joints become hypermobile and the vertebra can end up sliding forward because the facet joints cannot effectively hold the vertebra in place. Typical degenerative spondylolisthesis usually develops in the L4-L5 region and is more common in women over 50 years of age.
Type IV: Similar to Type II C, Type IV involves a fracture. However, it is a fracture of any other part of the vertebra other than the pars interarticularis. For example, the facet joints may collapse, separating the front part of the vertebra from the back part.
Type V: Tumors in the spine can also cause spondylolisthesis because they weaken the bones and can cause fractures that separate the vertebrae, leading to instability and potential slippage.
Type VI: develops after surgical treatment of the spine. It is also known as iatrogenic spondylolisthesis, and is usually associated with postoperative instability of the spinal motion segments.
Symptoms of spondylolisthesis
Symptoms of spondylolisthesis with minor mechanical disturbance of the location of the vertebra may be limited to discomfort after physical activity.
As the vertebra moves, conditions arise for a compression effect on the spinal cord (with anterolisthesis) and on the nerve roots (retrolisthesis). Mechanical impact on nerve structures can lead to symptoms of compression of the spinal cord or roots.
With severe compression of the spinal cord, serious complications such as cauda equina syndrome may occur, which requires emergency surgical intervention.
Most often, the following symptoms appear with spondylolisthesis:
- Pain in the lower back (neck) increases when turning or bending
- Pain in arms or legs
- Pain that runs down the back of the leg, pain in the buttocks
- Weakness in legs, arms
- Tingling or numbness in the extremities
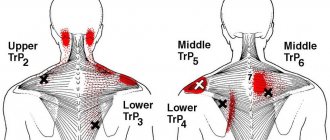
- Muscle discomfort
- Muscle spasms
- Difficulty walking
- Bladder and bowel dysfunction (cauda equina syndrome)
Prevention
Doctors at the ADANAYA clinic recommend:
- Moderate but regular physical activity, physical activity and compliance with other healthy lifestyle rules.
- When working at a desk or computer desk, watch your back position. You need to sit straight, and the height of the chair should be adjusted (seat at knee level). You can place a small bench or other support under your feet.
- If the work is standing or you have to stand in a long line, it is important to change your position often (every 10 minutes). Walking in place and rolling from heel to toe also helps.
- When lifting and moving heavy objects, it is important to distribute the weight correctly. It is best to divide the load into parts so that you can carry it not in one hand, but in two. If you need to lift something heavy, then it is not your back that should bend, but your knees, so that there is no strain on the lower back. It is better to carry cargo over long distances in a backpack, which will be located on the back, and not in a bag over the shoulder or in one hand (this is safer for the spine).
- You also need to sleep properly. The bed should be semi-soft, and instead of a cushion under the head there should be a rectangular pillow.
- Playing sports will also not hurt, but instead of running it is better to choose race walking, since it is less traumatic for the spine.
- It is recommended to avoid drafts and hypothermia, as this may cause additional tension in the muscles adjacent to the spine, which creates additional conditions for illness.
Diagnosis of vertebral displacement
As a rule, it is impossible to obtain visual signs of spondylolisthesis (vertebral displacement) based on the examination of the patient.
Patients usually complain of back pain and occasional pain in the legs or arms. Misalignment of the vertebrae (spondylolisthesis) can often cause muscle spasms or stiffness in the harness tendons.
The diagnosis of vertebral displacement is easily made using simple radiographs. A lateral x-ray can clearly show the presence of slippage of one vertebra in relation to another.
Spondylolisthesis is measured as the percentage of displacement of a vertebra compared to the adjacent vertebra.
- Grade I is a displacement of up to 25%.
- Grade II ranges from 26% to 50%.
- Grade III ranges from 51% to 75%.
- Grade IV ranges from 76% to 100%.
- Grade V or spondyloptosis occurs when a vertebra has completely fallen out of the underlying vertebra.
If the patient complains of pain, numbness, tingling or weakness in the legs, the doctor may order additional tests. These symptoms may be caused by stenosis or narrowing of the foramina and compression of the nerve roots. A CT scan or MRI may help identify nerve compression associated with vertebral misalignment. Sometimes a PET scan can help determine whether the bone at the defect site is active. This may help in choosing treatment tactics.
Features of preparation
Initially, an MRI is performed, the results of which determine the degree of displacement, the percentage of deformation and narrowing of the intervertebral discs. It is also necessary to perform an X-ray of the cervical or lumbar region in two standard projections with functional tests in the lateral projection. Based on this, it is chosen which spine surgery will be performed for spondylolisthesis.
As part of the preoperative examination, the following is prescribed:
- UAC and OAM;
- Doppler ultrasound of the vessels of the lower extremities;
- CT;
- electromyography.
Treatment of vertebral displacement
- Initial treatment for spondylolisthesis (displacement of the vertebrae) is conservative and based on symptoms.
- A short period of rest or avoidance of activities such as heavy lifting, bending, and athletics may help reduce symptoms.
- Physical therapy can help increase range of motion in the lumbar or cervical spine, relieve muscle spasms, and strengthen core muscles.
A physical therapy program is one of the most effective treatments for spondylolisthesis for two main reasons: (1) It can help strengthen the muscles that support the spine, and (2) it can teach the patient how to maintain spinal function and prevent further progression of vertebral misalignment.
Physical therapy includes both passive and active treatment methods.
- Passive treatments help relax the body. They are called passive because the patient does not actively participate. A physical therapy program may begin with passive treatment to allow the body to heal, especially if the patient has pars interarticularis fractures.
- But the main goal of physical therapy is active treatment. These are therapeutic exercises that strengthen the body and help prevent the recurrence of possible pain associated with a misaligned vertebra.
Passive treatment
The doctor may prescribe passive procedures such as:
- Deep tissue massage: This method aims to relieve spasm and chronic muscle tension that occurs due to the body's adaptation to biomechanical disorders associated with vertebral misalignment.
- Hot and cold therapy: alternating hot and cold therapy. By using heat, blood flow can be achieved to a specific area and the increased blood flow brings more oxygen and nutrients to that area. Blood is also needed to remove the byproducts created by muscle spasms and also aids in healing.
- Cold therapy, also called cryotherapy, slows blood circulation and helps reduce inflammation, muscle spasms and pain. Ice packs can be used for cryotherapy, but currently a special physiotherapeutic hardware technique called cryotherapy is used to cool tissues.
- TENS (transcutaneous electrical nerve stimulation): TENS helps reduce muscle spasms and it can also increase the production of endorphins, natural pain relievers.
- Ultrasound: By increasing blood circulation, ultrasound helps reduce muscle spasms, swelling, stiffness and pain. The sound waves penetrate deep into muscle tissue, creating heat that enhances circulation and healing.
Patient reviews
Vladimir Pokladov Minsk
I injured my back while training at the gym. I couldn’t calmly tie my shoelaces. I came to the clinic through work acquaintances when it was just opening. I was amazed that they immediately told me how to heal economically. They recommended some procedures to choose from. What immediately caught my eye was what they thought about people. There are significant improvements at the moment.
Oksana Aleksandrovna Minsk
I discovered the wonderful SpineMed center, where all the staff treats clients with great attention! I would like to thank massage therapists Vitaly Trotsyuk and Maxim Troyan for their work, professionalism, and their golden hands! Massage therapists work responsibly and efficiently! Thanks to the administration and management of the center for the good selection of personnel. I wish all the employees of the center good health and all the best! Good luck and prosperity to the center!
Active treatments
In the active portion of physical therapy, the physical therapy therapist will teach the patient various exercises to improve flexibility, strength, stability of the spinal column and restore range of motion. The physical exercise program (physical therapy) is individualized, taking into account health and medical history. Exercises for one person may not be suitable for another person with spondylolisthesis. Thus, the exercise therapy doctor selects an individual exercise program for each patient and the task of the set of exercises is to create a muscle corset that will compensate for biomechanical disorders associated with vertebral displacement.
If necessary, the patient receives information from a physical therapy doctor on how to correct his posture and incorporate ergonomic principles into daily activities. This is all part of the physical self-care or self-medication aspect: through physical therapy, the patient learns good habits and principles to better care for the body.
Rehabilitation after surgery
If the condition is satisfactory before surgery and there are no complications associated with surgery, the patient does not need specialized rehabilitation centers and can recover at home, visiting the pool, receiving massage and therapeutic exercises.
Author of the article: neurosurgeon Anton Viktorovich Vorobiev Frame around the text
Why choose us:
- we will offer the most optimal treatment method;
- we have extensive experience in treating major neurosurgical diseases;
- We have polite and attentive staff;
- Get qualified advice on your problem.
Surgical treatment of vertebral displacement (spondylolisthesis)
Surgical treatment may be recommended if there is severe displacement of the vertebra or there is no effect of conservative treatment.
The type of surgery depends on the type of spondylolisthesis. Patients with isthmic spondylolisthesis may undergo surgical reconstruction of the defective part of the vertebra. If an MRI scan or PET scan shows that the bone is active at the site of the defect, then it will be restored when the arches are reconstructed. This surgery involves removing any scar tissue from the defect and placing a bone graft in the area, followed by screw fixation.
If there are signs of compression of nerve structures, surgery may include decompression to create more space for the nerve roots to exit the spine. Decompression is often combined with vertebral fusion, which can be performed either with or without screws. In some cases, the vertebrae are returned to their normal position before fusion is performed, and in other cases, only fusion can correct the misalignment of the vertebra. Outcomes and recovery after surgery depend on a comprehensive rehabilitation program.
Massage session:
All movements are performed from the bottom up, along the course of the lymph. The area above and below the diseased area must be captured. Therefore, the massage begins from the thoracic region, the buttocks and thighs are massaged. If the pain is localized on one side, the healthy lumbar region is treated first. Each lumbar massage session lasts from 15 to 30 minutes, depending on the pathology and individual condition of the patient. At first, the impact should be less intense; the pressure and activity of the massage can be increased from 2-3 sessions.
Complications and prognosis of spondylolisthesis
Complications of a misaligned vertebrae (spondylolisthesis) include chronic pain in the lower back or legs, and numbness, tingling, or weakness in the legs. Severe nerve compression can cause problems with bowel or bladder control, but this complication is very rare.
The prognosis for patients with spondylolisthesis is good. Most patients respond well to conservative treatment.
If severe symptoms are present, surgery may help relieve symptoms by decompressing nerve structures.
results
| ✓ Relief of pain symptoms |
| ✓ Restoration of the functions of the musculoskeletal system |
| ✓ Formation of healthy and beautiful posture |
The reputation of the clinic is strengthening and growing every year!
The ADANAYA Clinic, specializing in the treatment of diseases of the spine and joints, has a team of specialized specialists in the treatment of vertebral displacement. For more than 7 years, we have been successfully restoring the health of our patients, restoring them the freedom and joy of movement without pain. Treatment at the clinic gives positive results in 98% of cases, which is confirmed by reviews of our specialists.
We do not leave you alone with the disease. We heal with our hands and heart.