Plasters for a hernia of the lumbar spine are a very convenient and effective method of treatment. The most important symptom of a lumbar disc herniation is pain. It becomes stronger when bending, turning, or sudden movements. A patch for a spinal hernia is a convenient and effective way to relieve pain and inflammation.
An anesthetic patch for a hernia is a simple method of relieving the symptoms of the disease.
The main cause of spinal hernia is osteochondrosis, heavy lifting, high physical activity, and lack of physical activity. When pain occurs, the fibrous ring in the vertebrae ruptures and the nucleus pulposus protrudes. In this case, pressure occurs on the nerve roots of the spinal cord and because of this, pain occurs.
In the article we will tell you in detail which plasters will be most effective for intervertebral disc herniation: TOP 9 effective plasters.
Benefits of patches
Therapeutic patches are a folk remedy for the treatment of sacrolumbar, as well as thoracic and cervical hernia. Particularly popular is Nanoplast Forte, which copes well with inflammatory processes in the tissues and muscles of the back (according to the manufacturer).
Using the patches is very simple and convenient. The advantages of these small pieces of matter for intervertebral disc herniation:
- lasts for a long time;
- combined with other conservative treatment methods;
- they are very easy to use, anyone can do it;
- reducing the treatment time for lumbar hernia;
- the rehabilitation process after surgery is accelerated;
- reduction of temporary disability due to back pain;
- is an excellent replacement for compresses and bandages.
Very often on TV and the media there are advertisements for specialized patches for back pain.
Nanoplast has conflicting reviews from patients and specialists
Remember, this piece of material only relieves pain for a while . He is in no way able to cure the disease itself or avoid the appearance of a hernia.
But this does not apply to patches with chondroprotectors and natural herbs, which can improve the condition of the cartilage tissue of the intervertebral discs.
When the first signs of a lumbar hernia appear, you should consult a therapist or neurologist.
A herniated disc is a very dangerous disease, so treatment should begin as quickly as possible to prevent complications.
How is a sequestered hernia formed?
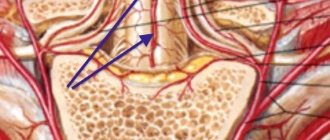
Between the vertebrae are the nucleus pulposus, made of jelly-like cartilage tissue, designed to reduce friction and soften shock loads.
They are surrounded by a dense fibrous ring of collagen fibers. With osteochondrosis, metabolic processes in the fibers of the fibrous ring are disrupted, as a result of which they weaken and can rupture under the influence of high loads. At the site of the rupture, the nucleus pulposus protrudes beyond the spinal column - a hernia is formed. A sequestered disc herniation occurs when a protruding fragment of the nucleus pulposus breaks off and floats freely. This separated part is called "sequester". Most often it ends up in the spinal canal, where the spinal cord is located. Sequester is not capable of self-dissolution; deprived of nutrition, it loses moisture and undergoes the following changes:
- acquires hard, pointed edges;
- affected by microorganisms;
- causes inflammation of surrounding tissues.
A moving sequestered intervertebral hernia can injure the spinal cord and the roots extending from it, cause swelling that compresses the meninges, or cause purulent inflammation. Its movement can lead to the most severe consequences.
Based on local anesthetics
Lidocaine, which is included in their composition, has an excellent anesthetic effect. This active substance effectively penetrates the skin in the affected area. After half an hour, the pain goes away completely and the effect lasts 8-9 hours.
The drugs act no worse than the therapeutic blockade based on novocaine, which is why they are so popular. There are no side effects. With prolonged use, they reach maximum concentrations in the blood. Names - “Versatis”, “Emla”, “Parapran”.
Pepper and mustard patches
Pepper patch
Their composition is based on pepper or mustard, they are widely used to suppress back pain. One side is covered with a sticky composition based on mustard or pepper mixture. The main active ingredient of the pepper patch is capsaicin oil; it is part of the red pepper extract and has a powerful warming effect.
Positive sides:
- improvement of blood circulation in soft tissues;
- the effect lasts up to 4 hours;
- warming and positive irritating effect;
- metabolism in tissues improves;
- The hernia treatment process progresses more quickly.
If you use pepper patch for a long time, you may experience allergies or burns. Due to the resulting inflammation, it will not be possible to use ointments, gels and other drugs. Therefore, it is recommended to apply the patches through a bandage or cloth if discomfort occurs.
You can also moisten the area where it will be glued with Johnson's baby oil or regular baby cream. Choose pepper patches that have a mesh structure. The mesh structure protects the skin from burns, so you can wear it longer.
Be sure to read: 10 methods of rehabilitation after removal of a lumbar hernia (spine surgery): stages, exercises, complications, consequences
We read an excellent article in which you can learn in detail about the pepper patch: All about the pepper patch for cervical osteochondrosis (price, reviews, photos, where to apply)
Treatment of lumbar hernia without surgery
A hernia of the lumbar spine does not always manifest itself as pain, numbness in the legs or difficulty walking. It is often found by chance after an MRI. What to do? If you have been diagnosed with an intervertebral hernia, but it does not affect your quality of life, then you have no reason to worry. However, it is better not to wait for attacks of pain, “shooting” in the back and limbs, but to consult with a neurologist so that he can assess the clinical picture, predict the course of the disease and, if necessary, promptly select conservative treatment tactics.
Treatment of lumbar spinal hernia without surgery involves non-surgical treatment methods, which are often combined with each other:
- Manual therapy.
- Therapeutic physical education (physical therapy).
- Massage.
- Drug therapy, including blockade of the lumbar spine, when drugs and painkillers are injected directly into the area of the affected vertebra or joint.
- Ultrasound therapy for hernias.
- Shock wave therapy for spinal hernias.
- High-field magnetic stimulation and other physiotherapy procedures.
The doctors of the Rehabilitation Center at the Pirogov Clinic (chiropractors, neurologists, algologists), even during the quarantine period, are ready to provide emergency assistance to patients with acute and intense pain syndromes.
Worldwide practice shows that only 30% of intervertebral hernias require surgical intervention, and all the rest, subject to timely and adequate conservative therapy, can be cured without surgery.
View reviews about the treatment of intervertebral hernias in our clinic
Heat reflective patch
Heat reflective patches are the safest. They do not contain any medicinal substances and have no contraindications. Their action is based on the fact that they reflect the heat of the human body and have a gentle effect on the sore spot. Attach it to clothing.
The heat reflective patch is essentially a fabric bandage
Anti-inflammatory patches
They contain the active ingredient - diclofenac. This substance acts like the tablets of the same name, but absorption occurs through the skin. Painkillers eliminate pain and inflammation in the hernia area, especially when lumbago occurs in the lower back.
They relieve pain to a lesser extent than anesthetic-based patches, but also show good effectiveness. They are recommended for inflammation. They have almost no contraindications, do not cause burns, allergic reactions, or irritation.
Voltaren patch, according to patient reviews, does not adhere well to the skin
As a preventive measure, it is recommended to take drugs that protect the gastric mucosa, for example, Omeprazole. You can use them for a maximum of daily use for no more than three weeks, otherwise problems with the gastrointestinal tract may occur. The most common drugs are Voltaren, Diclofenac-ratiopharm, Ketotop.
Removal
The product can stay on the skin for several days thanks to the strong adhesives included in its composition. Naturally, removing the sticker can be quite painful and cause discomfort.
First of all, it is worth remembering that the sticker cannot be torn off abruptly, otherwise it can cause significant damage to the skin.
Particular attention should be paid to people with sensitive skin who decide to be treated in this way, as well as pregnant women, as their sensitivity may increase due to hormonal changes.
You can remove the patch painlessly using water or simple sunflower oil. The best option is to keep the sealed area under the shower or lie in the bathtub. After this, the sticker can be removed without unnecessary difficulties.
Using pepper patch as an additional treatment is a very good way to relieve yourself of severe pain.
However, do not forget that any new means of restoring health must be approved by your doctor, since each individual case of the disease requires a special approach to treatment.
If you want to get more information like this from Alexandra Bonina, check out the materials on the links below.
Additional useful information:
- My free books, videos and master classes
- My exercise programs and video courses
- My printed books (available in major online stores)
- Free online marathon “How to save your face from old age”
See more useful materials on my social networks:
YouTube | VKontakte | Yandex.Zen | Instagram | Telegram | Facebook
Denial of responsibility
The information in the articles is for general information purposes only and should not be used for self-diagnosis of health problems or for therapeutic purposes. This article is not a substitute for medical advice from a doctor (neurologist, therapist). Please consult your doctor first to know the exact cause of your health problem.
I will be very grateful if you click on one of the buttons and share this material with your friends 
Chinese patches
They contain various medicinal herbs and homeopathic substances. This is alternative medicine. They are named so because they are based on traditional Chinese medicine. Unfortunately, they do not have a patent in our country and their effectiveness has not been officially confirmed. Doctors rarely prescribe them. But, oddly enough, people prefer them because of their natural ingredients , which have a positive effect on the human body.
There are many diseases that Chinese patches can treat: radiculitis, osteochondrosis and many others. They must be used in conjunction with other painkillers, as they have a very mild effect.
Plasters based on chondroprotectors
Preparations based on chondroprotectors have proven themselves to be excellent - these are substances that effectively restore cartilage tissue. The fact is that with a hernia, the cartilage tissue between the vertebrae is very quickly destroyed and therefore the disease progresses.
It is very important to take medications based on chondroprotectors. Nanoplasters also contain various bioadditives. There is only one patch available for sale called Nano Patch GS.
The price for a course of treatment with Nano Patch GS patches is more than 7,000 rubles.
Pros:
- the active substances they contain - chondroitin and glucosamine sulfate - stimulate cell growth in cartilage tissue, protect them from destruction;
- vitamin B1 and thiamine restore the body's defenses;
- the amount of other medications taken is reduced.
Minuses:
- requires long-term use;
- very expensive;
- do not reduce back pain.
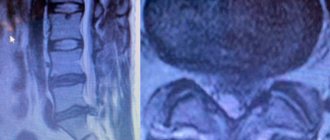
Basic principles of diagnosis and treatment
The only informative method for identifying a sequester hernia is MRI, and new generation tomographs with high resolution and a magnetic field strength of at least 1.5 Tesla should be used. If bone sequesters are present, they can also be seen on x-ray. Myelography using a radiopaque contrast agent can be used to detect inflammation inside the canal.
Treatment of sequestered hernia is only surgical. Except in cases where emergency surgery is necessary, patients are scheduled for elective surgery, in preparation for which they must undergo a course of treatment with anti-inflammatory drugs to relieve pain and swelling. To prevent displacement of the sequestrum, patients are prescribed to wear a corset.
Surgical removal of a sequestered hernia can be combined with the elimination of destroyed parts of the intervertebral disc and subsequent surgery to reconstruct it using an endoprosthesis. Treatment without surgery for a hernia that has sequestered is simply impossible. By refusing surgical intervention, the patient will be constantly exposed to the threat of developing severe complications. After the operation, long-term rehabilitation is carried out, including modern methods of physiotherapy, manual therapy, acupuncture, and exercise therapy. All these measures ensure restoration of the functionality of the spine and accelerate recovery.
Review: top 9 patches for spinal hernia
- Nano Patch GS . It is made on the basis of chondroprotectors. Promotes the restoration of cartilage tissue. It does not eliminate pain, but in combination with other drugs it gives an excellent effect.
- Voltaren. Clinically proven effectiveness. The active substance is diclofenac (NSAID). Excellently copes with inflammatory processes in tissues. It helps well with pain arising from chronic diseases. When used, allergies may occur; it should not be used by children, pregnant or lactating women.
Voltaren - Versatis. The active ingredient is lidocaine. It is an anesthetic, so the pain goes away very quickly. Cons – does not remove inflammation and does not have a healing effect.
Versatis - Ketonal Thermo. It has a warming effect, relaxes muscles and joints, and significantly suppresses pain. Duration of action is 9-10 hours. Cannot be used during pregnancy or diabetes.
Ketonal Thermo - Nanoplast Forte. This is an orthopedic plaster. Contains fine powder of magnetic particles. Its action is based on the simultaneous operation of magnetic and infrared fields. Has a restorative effect. The effect is long lasting – 10-12 hours. It is advisable to use before bedtime.
Nanoplast Forte - Pepper patch . This is a warming patch that relieves pain. But it can only be used outside the acute stage. May cause skin burns. This is the cheapest hernia patch, the cost of which starts from 10 rubles.
Be sure to read: TOP 14 types of headaches in pictures, names and treatment
Contraindications
Back pain patches should be used with extreme caution.
The main contraindications when using pepper, anesthetic and anti-inflammatory patches:
- It is forbidden to attach to open wounds and skin diseases;
- cannot be attached to areas of the skin where there are moles and various damage to the skin;
- with poor blood circulation;
- cannot be used by children, pregnant and lactating women;
- for stomach problems (gastritis, ulcers);
- not recommended for diabetics;
- if you are allergic to any component included in the composition;
- with individual intolerance.
Regarding Chinese patches, we can say that there are many counterfeit products, so you need to order from trusted stores.
You can run into fakes on the medical market, especially for Chinese plasters.
When choosing a patch, you should consult your doctor or listen to the advice of friends. Be sure to read the instructions supplied with the drug. Many people choose patches to cope with back pain because they are more effective than tablets and gels. It is worth remembering that patches based on chemicals have clinically proven effectiveness, but those based on natural medicinal herbs or dietary supplements do not.
Using only one patch for back pain will in no way get rid of a herniated disc.
To eliminate a hernia in the lumbar region, you must undergo comprehensive non-surgical treatment, which includes:
- Exercise therapy – useful exercises for the spine;
- physiotherapeutic procedures;
- taking medications;
- massage and manual therapy;
- treatment at home with folk remedies.
Symptoms and danger of sequestration in the thoracic and cervical spine
This localization of intervertebral sequestered hernia is the most dangerous, since the spinal cord is located in the spinal canal of the cervical and thoracic areas of the ridge. The higher the localization, the more limbs are paralyzed in the worst case scenario. Therefore, the most severe consequences are lesions of the intervertebral discs of the neck, which can cause paralysis of the entire body. Symptoms of the appearance of sequestration are a sharp girdling pain in the chest or neck, radiating to the upper extremities and accompanied by numbness and muscle weakness. Jumps in blood pressure, hyperemia and an increase in local temperature may be observed.
If the spinal cord is affected, then signs of paralysis of all areas located below the affected area develop, and one half of the body may be affected. Progressive weakness, immobility of the limbs, loss of sensitivity of the skin appears, and urination disorders may appear.
Even if after the formation of a sequester hernia in the neck and chest there are no signs of paralysis, they can appear at any time, since the sequester can move, injuring the meninges or causing swelling that puts pressure on the spinal cord.
Real patient reviews
We conducted a survey of those people who used patches from different manufacturers to eliminate back pain:
Margarita, 25 years old, Chinese patches help me a lot, they have been helping me for more than three years and have never let me down. Currently, I have come across counterfeits, so I buy from reliable stores that work directly with China.
Oleg, 34 years old I tested on myself all types of patches that are commercially available. I decided to try it based on chondroprotectors. Fortunately for me, this effective remedy coped with the inflammation, and there was no more pain. By the way, he also cured my rheumatoid arthritis well.
Olga, 29 years old My back began to hurt severely during pregnancy. A friend recommended a patch based on an anesthetic. The pain quickly went away. And when I gave birth to my baby, I started using Voltaren. I really liked him too. Now I don’t know what back pain is.
Complete relief from a hernia does not occur immediately. Doctors must first diagnose the disease, for example using magnetic resonance imaging. Next, treatment will be prescribed and if the result is positive, you will be able to avoid surgical treatment. According to statistics, only 75% of all patients return to a normal lifestyle.
In any case, you should consult your doctor before starting treatment with patches on your own.
LUMBAR PAIN
Lumbar pain (LP), like headaches, is one of the most common complaints with which patients turn to both a local (family) general practitioner and a neurologist. According to WHO experts, almost 90% of people have experienced lower back pain at least once in their lives.
Among the most common causes of LBP are diseases of the spine, primarily degenerative-dystrophic (osteochondrosis, spondylosis deformans) and overstrain of the lumbar muscles. However, we should not forget that various diseases of the pelvic and abdominal organs, including tumors, can cause the same symptom complex as a herniated disc that compresses the spinal root.
The 20th century made serious adjustments to the understanding of the etiology and pathogenesis of BE. Initially, the main cause of their occurrence was considered to be inflammation of the nerve roots and trunks, which was reflected in such terms as lumbosacral radiculitis, radiculoneuritis, funiculitis, etc. Back in the 40-50s, “radiculitis” was often treated with massive doses of antibiotics. But subsequently, the infectious-inflammatory theory of the pathogenesis of BE began to be replaced by a vertebrogenic one, which was greatly facilitated by successful operations for disc herniation. They began to look for the cause of all BE in degenerative-dystrophic changes in the spine, in compression of a nerve root disc by a herniated disc. This period also corresponds to certain terminology: discogenic radicular compression syndrome, vertebrogenic radiculopathy, vertebrogenic reflex syndrome. In the 80-90s, the theory of the predominantly muscular origin of BE began to prevail among neurologists. Many researchers believe that in almost 90% of cases the cause of BE is myofascial syndromes, and vertebrogenic disorders account for no more than 10%. This is reflected in the corresponding terminology: dorsalgia, lumbodynia, myofascial syndrome.
- Etiology and pathogenesis of lumbar pain
The most common causes of BE are: pathological changes in the spine (primarily degenerative-dystrophic); pathological changes in muscles (most often myofascial syndrome); pathological changes in the pelvic and abdominal organs; diseases of the nervous system. The following are considered risk factors for the development of BE: heavy physical activity; physical stress; uncomfortable working posture; injury; cooling, drafts; alcohol abuse; depression and stress; consequences of “harmful” professions (exposure to high temperatures in hot shops and radiant energy, sudden temperature fluctuations, vibration, etc.).
The pathogenesis of PB can be reduced to the following simplified scheme. Painful impulses, regardless of the source (spine, overstrained muscle, “sick” internal organ) enter the spinal cord, from where it goes to special organs of muscle sensitivity - muscle spindles, overexcitation of which causes muscle spasm, leading to a change in body posture and increases it, increasing pain . This creates a vicious circle of maintaining pain. Muscle spasms can be aggravated by depression and chronic stress, which lower the threshold for pain perception, as well as alcohol, which softens the control of maintaining posture.
Among the vertebrogenic causes of BE there are: root ischemia (discogenic radicular syndrome, discogenic radiculopathy), resulting from compression of the root by a disc herniation; reflex muscle syndromes, the cause of which may be various degenerative changes in the spine.
Various functional disorders of the lumbar spine may have a certain significance in the development of LBP, when, due to incorrect posture, blocks of the intervertebral joints occur and their mobility is impaired. In the joints located above and below the block, compensatory hypermobility develops, leading to muscle spasm.
- Lumbar pain in various diseases of the spine
In addition to degenerative-dystrophic changes, relatively rare spinal pathology may also be important in the development of BE.
Spondylolisthesis - literally translated (from the Greek spondylos - vertebra and olisthesis - slipping) - a sliding vertebra that is displaced from the underlying one (most often the 4th or 5th, rarely the 3rd lumbar vertebra). Spondylolisthesis is observed in 2-4% of the population and in 7-10% of cases causes lumbosacral pain. The disease does not always manifest itself clinically and can be detected accidentally during an X-ray examination of the spine. It all depends on the nature of the displacement, i.e., on whether it is partial or complete. Depending on the angle of displacement of the sliding vertebra, stable and unstable spondylolisthesis are distinguished. Its stable form is characterized by the fact that when the spine bends and turns, the relationship between the protruding and underlying vertebrae is not disturbed. With unstable spondylolisthesis (more severe), these relationships are periodically disrupted.
Low back pain in childhood and adolescence is most often caused by abnormalities in the development of the spine. Spinal bifida (spina bifida) occurs in 20% of adults. Neurological symptoms occur in the cystic form of this pathology, when the dura mater protrudes and the epidural tissue grows. Upon examination, attention is drawn to hyperpigmentation, birthmarks, multiple scars, funnels and hyperkeratosis of the skin of the lumbar region. Sometimes urinary incontinence, trophic disorders, and weakness in the legs are noted. In this case, it is necessary to exclude rigid filament terminalis syndrome, which is characterized by thickening and shortening of the fila terminalis, which leads to overstretching of the spinal cord.
BE can cause lumbarization - the transition of the S-1 vertebra in relation to the lumbar spine and sacralization - the attachment of the L-5 vertebra to the sacrum. These anomalies are formed due to individual characteristics of the development of the transverse processes of the vertebrae.
Ankylosing spondylitis. In 1882, this disease was first described by the outstanding Russian neurologist V.M. Bekhterev under the name “stiffness of the spine with curvature.” It is currently referred to as “ankylosing spondylitis.” Almost all patients complain of lower back pain. According to various authors, the disease occurs in 0.08-2.6% of the population, and on average its prevalence is one case per 100. The vast majority of patients (up to 90%) are men aged 20-40 years. Rarely, the disease occurs in children and adults over 50 years of age.
Ankylosing spondylitis is manifested by inflammatory lesions primarily of low-moving joints (intervertebral, costovertebral, lumbosacral joints) and spinal ligaments. Gradually, ossification develops in them, the spine loses elasticity and functional mobility, becomes like a bamboo stick, fragile and easily injured. In the stage of pronounced clinical manifestations of the disease, the mobility of the chest during breathing and the vital capacity of the lungs are significantly reduced.
Tuberculous spondylitis. Chronic inflammation of the spine caused by tuberculosis. As a rule, one of the vertebrae is initially affected, in which a tuberculous granuloma develops, gradually destroying bone tissue. The strength of the outer layers of the vertebra prevents its deformation and the process is asymptomatic for a long time. This is the so-called prespondylytic phase, which in adults can last for many years. Clinically, tuberculous spondylitis begins to manifest itself when the process spreads to tissues adjacent to the vertebra or the affected vertebra is deformed. Often (up to 30% of cases), bruises contribute to the manifestation of the disease, and in children, in addition, various infections.
In children, the disease is more violent and the process often spreads to the vertebrae above and below. Gradually, the pain intensifies, local pain occurs when pressing over the lesion, gait becomes difficult, the mobility of the spine is sharply limited and its configuration changes, which leads to the formation of a hump.
When one or more vertebrae are affected by the tuberculosis process, purulent-necrotic masses can form an abscess that sometimes breaks out, forming a fistula.
Diagnosis of tuberculous spondylitis is initially based on X-ray data of the spine and other organs. The first radiological sign is a narrowing of the intervertebral disc. Then local osteoporosis, bone cavity, marginal destruction, wedge-shaped deformity and, finally, edema abscesses appear in the vertebral body. Breakthrough of caseous masses under the posterior longitudinal ligament into the epidural space is usually accompanied by compression of one or more roots, sometimes the spinal cord with the development of lower paraparesis.
Luetic spondylitis. It is a complication of secondary or tertiary syphilis. Differential radiological signs include severe osteosclerosis, defects of adjacent plates of the affected vertebrae, osteophytes (without ankylosis). The luetic nature of the process should be assumed in the case of recurrent meningitis, meningoencephalitis, repeated strokes (especially at a young age), and spontaneous subarachnoid hemorrhages. To confirm the diagnosis, blood and cerebrospinal fluid tests are performed - the Wassermann reaction and immobilization of treponema pallidum (TIPT).
Brucellous spondylitis. The etiology of the disease is associated with undulating fever with widespread rises in temperature (patients tolerate them relatively easily), profuse sweating, arthralgia and myalgia, lymphadenitis with a predominant enlargement of the cervical and, less commonly, inguinal lymph nodes. The diagnosis is confirmed by serological reactions of Wright and Heddelson.
Typhoid spondylitis. It occurs against the background of a long period of imaginary recovery. The diagnosis is confirmed by the Widal serological reaction.
Dysenteric spondylitis. The diagnosis is confirmed by the results of culture of intestinal contents in the acute period of dysentery.
Rheumatic spondylitis. Sometimes it complicates the course of rheumatism, which is typical for young people and is accompanied by relapses, changes in the heart, polyarthritis with damage to large joints. If bacterial endocarditis is added, then in this case there is fever, leukocytosis, a shift in the blood count to the left, and a sharp increase in ESR. To confirm the diagnosis, rheumatic tests, repeated blood cultures, ECG, and echocardiography are performed.
Nonspecific spondylitis. They can complicate any infection, but most often the intestinal and urinary tract.
Spinal osteomyelitis. Inflammatory damage to the bone marrow with subsequent spread of the process to all elements of bone tissue. Accounts for about 2% of all cases of bone osteomyelitis. The lumbar vertebrae are affected more often than the cervical and thoracic ones. There are nonspecific and specific osteomyelitis. The first is caused by pyogenic pathogens (mainly staphylo- and streptococci); the second - may be tuberculosis, syphilitic and other etiologies. With nonspecific osteomyelitis of the spine, the focus of purulent infection can be located in any part of the body in the form of boils, carbuncles, infected skin wounds, eczema, etc. and is transmitted hematogenously. However, the spine is often affected from nearby purulent foci, for example, with open infected fractures and gunshot wounds. Spinal osteomyelitis can occur acutely, subacutely and chronically. With an acute onset, fever, pronounced blood changes, and sharp, shooting pain in the lower back occur quickly. In the subacute and chronic course of the disease, which occurs more often, the pain is less pronounced. Characteristic changes on radiographs are revealed only after 1.5-2 months. after the onset of the disease.
Epidurit. There is a purulent focus: in 80% of cases, pyoderma, septic changes in the blood - leukocytosis, increased ESR, shift of the formula to the left; rapid increase in pain, fever, symptoms of intoxication. At the beginning of the disease, the pain is local, then signs of compression of one or more roots appear: symptoms of tension, sensory and motor disorders; meningeal symptoms. In the advanced stage of the disease, after an average of two days, gradually increasing pelvic and conduction disorders join these symptoms.
Additional studies include magnetic resonance imaging, cultures of blood, urine and discharge from purulent lesions. Lumbar puncture is contraindicated due to the risk of infection in the subarachnoid space.
Intramedullary abscess. In the initial stage, it is clinically similar to epiduritis. The main differential feature is the type of distribution of conduction disorders: ascending with epiduritis and descending with intramedullary abscess.
Multiple myeloma. It manifests itself as local pain in the thoracic or lumbar spine, which occurs gradually against the background of progressive weight loss, sweating, undulating fever and proteinuria. X-rays reveal diffuse osteoporosis, osteosclerosis, and later secondary spinal deformity. When pathological fractures occur, the pain increases sharply, symptoms of tension, radicular disorders, and lower paraparesis appear. In 70% of cases, ESR increases and normochromic anemia is detected.
| In the 80-90s, the theory of the predominantly muscular origin of BE began to prevail among neurologists. Many researchers believe that in almost 90% of cases the cause of BE is myofascial syndromes, and vertebrogenic disorders account for no more than 10%. This is reflected in the corresponding terminology: dorsalgia, lumbodynia, myofascial syndrome |
Electrophoresis of blood proteins reveals paraproteinemia, hypogammaglobulinemia, and Bence Jones protein in the urine. Hypocalcemia is detected in the blood. The diagnosis is confirmed by examining the puncture of the sternum. In this case, myeloma cell proliferation is determined in 90% of cases. In addition, an X-ray of the skull, chest, and pelvic bones should be performed—favorite sites for myeloma.
Spinal tumors. They can be benign or malignant, originating primarily from the spine or metastatic. Benign tumors of the spine (osteochondroma, chondroma, hemangioma) are sometimes clinically asymptomatic. With hemangioma, a spinal fracture can occur even with minor external influences (pathological fracture). Malignant tumors are predominantly metastatic from the prostate and mammary glands, uterus, lungs, adrenal glands and other organs. Pain in this case occurs much more often than with benign tumors, usually persistent, painful, intensifies with the slightest movement and deprives patients of rest and sleep. Characterized by a progressive deterioration of the condition, an increase in general exhaustion, and pronounced changes in the blood. In diagnosis, radiography, computed tomography, and magnetic resonance imaging are of great importance.
Osteoporosis. The main cause of the disease is a decrease in the function of the endocrine glands due to an independent disease or against the background of general aging of the body. Patients who long-term use of hormones, aminazine, anti-tuberculosis drugs, tetracycline may develop exogenous osteoporosis. Radicular disorders occur due to deformation of the intervertebral foramina, and spinal disorders (myelopathy) due to compression of the radiculomedullary artery or vertebral fracture, even after minor injuries.
Myofascial syndrome. According to many researchers, this is the main reason for the development of BE. It can occur due to overexertion (during heavy physical activity), overextension and bruises of muscles, unphysiological posture during work, reaction to emotional stress, shortening of one leg and even flat feet. Predisposing factors include: hypovitaminosis B1, B6, B12, folic and ascorbic acids, deficiency of microelements (potassium, calcium, magnesium, iron), hypoglycemia, gouty diathesis, chronic infections, sleep disturbance. In the literature, this phenomenon is often referred to by other terms: myalgia, myofibrositis, myofasciitis, trigger points (areas, zones).
In addition to myofascial pain syndrome, the cause of LBP can be other muscle diseases.
Myositis. They represent a large group of diseases of various etiologies: rheumatic, tuberculosis, syphilitic, viral, etc. Parasitic diseases - trichinosis, echinococcosis can also lead to muscle damage. In this case, persistent and prolonged pain is noted.
Widespread muscle changes are found in collagenoses, primarily in dermatomyositis, which can begin suddenly, especially after exacerbation of foci of chronic infection, colds or hypothermia. Muscle soreness, including the lower back, is typical. Simultaneously with the pain or after its cessation, weakness and “weight loss” of the muscles occur, limiting the patient’s motor activity. Skin changes: redness with a purple tint, pinpoint or spotty rash, swelling. During bed rest, foci of necrosis may occur with subsequent development of scars. Severe peeling often occurs, causing the skin to resemble fish scales. Muscle pain and skin changes are usually symmetrical. Half of patients with dermatomyositis have calcification in individual muscles. With multiple calcifications, the skin becomes lumpy and dense to the touch. In the ossifying form of the disease, the ossification of the muscles and subcutaneous tissue can be so strong that it fetters the patients, they become as if dressed in a shell.
Scleroderma. There is widespread thickening of the skin and subcutaneous tissue. The pain is less pronounced than with dermatomyositis.
Diseases of internal organs. PA often occurs with diseases of internal organs: gastric and duodenal ulcers, pancreatitis, cholecystitis, urolithiasis, etc. The pain can be pronounced and imitate the picture of lumbago or discogenic lumbosacral radiculitis. However, there are also clear differences, thanks to which it is possible to differentiate referred pain from that arising from diseases of the lumbosacral part of the peripheral nervous system. These are primarily clinical signs of the underlying disease. For example, with a peptic ulcer of the stomach and duodenum, patients, as a rule, complain of nausea, vomiting, heartburn, belching, which does not happen with radiculitis, and attacks of renal colic are accompanied by frequent urination with pain, nausea, vomiting, and bloating. Difficulties in differential diagnosis are caused by cases when the signs of disease of the internal organs are weakly expressed or the patient has reflected pain combined with pain caused by pathology of the lumbosacral part of the peripheral nervous system.
Very often, BE is caused by diseases of the pelvic organs: the uterus, appendages, prostate gland, vas deferens, rectum, which is primarily due to the proximity of these organs to the lumbosacral nerve formations. Therefore, along with reflected pain, pain from direct impact may also appear. In the past, the term “adnexitis-sciatica” was even used. Lower back pain can occur when the uterus is in an incorrect position during pregnancy, and in women who interrupt sexual intercourse to prevent pregnancy. Gynecological diseases are characterized by a predominant increase in pain during sexual intercourse.
Increased pain during bowel movements is typical for diseases of the rectum: hemorrhoids, tumors, fissures, polyps. In these cases, diarrhea alternating with constipation and significant weight loss are noted. A constant sign of the disease is the presence of mucus and blood in the stool. In some cases, hypochromic anemia is detected. When straining, hemorrhoids may fall out. For differential diagnostic purposes, sigmoidoscopy is indicated to exclude colon tumors.
Dissecting aortic aneurysm. The pain radiates to the abdomen, legs and is accompanied by a collapsing state. A tumor-like formation is palpated in the abdomen, over the projection of which a systolic murmur is heard. Additionally, ultrasound and computed tomography examinations of the abdominal organs are performed.
Diseases of the nervous system. In some cases, BE occurs in the initial stages of the disease, is temporary and is combined with various neurological disorders, and in others it is long-term or permanent. Transient lumbar pain can be observed in acute inflammatory diseases of the nervous system: meningitis, myelitis, polyradiculoneuritis, which have a predominantly acute onset and are severe. At the same time, mild or moderate pain in the lower back seems to recede into the background. In addition, they decrease or disappear quite quickly. PB can also occur several years after acute inflammatory diseases of the nervous system.
Spinal cord tumors. Depending on the primary localization, they are divided into intra- and extramedullary, which are more common and are predominantly benign: limited, do not infiltrate the brain tissue. BE in extramedullary tumors is an early sign of the disease. They arise due to a decrease in the free cavity of the spinal canal due to tumor growth, tension in the nerve roots and meninges.
Lumbar pain can be observed with multiple sclerosis, spinal gliosis, and tabes of the spinal cord. They do not play a leading role in the clinical picture.
Finally, one should remember about the possibility of the occurrence of pain in neuroses, which, unlike pain in organic diseases of the nervous system, are not constant and clearly localized. They move from one part of the body to another, and their severity depends on the general emotional state. Usually there are no symptoms of tension in the spinal roots and prolapse from the reflex sphere.
- Clinical symptoms of lumbar pain
Most often, BE occurs at the age of 25-44 years. There are acute pains, lasting, as a rule, 2-3 weeks, and sometimes up to two months, and chronic pains - over two months.
Compression radicular syndromes (discogenic radiculopathy) are characterized by a sudden onset, often after heavy lifting, sudden movements, or hypothermia. Symptoms depend on the location of the lesion. The syndrome is based on compression of the root by a disc herniation, which occurs as a result of degenerative processes facilitated by static and dynamic loads, hormonal disorders, and injuries (including microtraumatization of the spine). Most often, the pathological process involves the area of the root from the dura mater to the intervertebral foramen. In addition to disc herniation, bone growths, scars of epidural tissue, and hypertrophied ligamentum flavum may be involved in root trauma.
The upper lumbar roots (L-1, L-2, L-3) are rarely affected: they account for no more than 3% of all lumbar radicular syndromes. L-4 is most often affected (6%), causing a characteristic clinical picture: mild pain along the inner-lower and anterior surfaces of the thigh, the medial surface of the leg, paresthesia in this area, slight weakness of the quadriceps muscle. Knee reflexes are preserved and sometimes even increased. The L-5 root is most often affected (46%). The pain is localized in the lower back, gluteal region, along the outer surface of the thigh, the anterior outer surface of the lower leg down to the foot and the first three fingers. It is often accompanied by a decrease in the sensitivity of the skin of the anterior outer surface of the leg and the strength in the extensor of the first finger. The patient finds it difficult to stand on his heel. With long-term radiculopathy, hypotrophy of the tibialis anterior muscle develops.
The S-1 root is just as often affected (45%). Lower back pain radiates along the outer back of the thigh, outer surface of the leg and foot. Examination often reveals hypalgesia of the posterior outer surface of the leg, decreased strength of the triceps muscle and toe flexors. It is difficult for such patients to stand on their toes. There is a decrease or loss of the Achilles reflex.
Vertebrogenic lumbar reflex syndrome. It can be acute or chronic. Acute LBP (lumbago, “lumbago”) develops over several minutes or hours, often suddenly due to awkward movements. Piercing, shooting (like an electric shock) pain is localized throughout the lower back, sometimes radiating to the iliac region and buttocks, sharply intensifies with movement, coughing, sneezing, and decreases when lying down, especially if the patient finds a comfortable position. Movements in the lumbar spine are limited, the lumbar muscles are tense, Lasegue's symptom is caused, often bilaterally. Acute lumbodynia usually lasts 5-6 days, sometimes less. The first attack ends faster than subsequent ones. Repeated attacks of lumbago tend to develop into chronic LBP.
Myofascial pain. It is usually long-lasting, ranging from mild discomfort to severe and excruciating pain. It can occur at rest and during movement, is associated with trigger points and is non-segmental in nature, and the zone of greatest intensity is rarely localized at the most trigger (hyperirritable) point in a dense cord of skeletal muscle, painful on palpation. Trigger points are activated by overload, physical fatigue, injury or cold. Pressure on them causes or intensifies painful phenomena in the area of referred pain.
It is worth highlighting a number of clinical symptoms that are not typical for BE caused by degenerative-dystrophic changes in the spine or myofascial syndrome. They should alert you, as they may be a sign of the presence of pathological processes in the pelvic and abdominal organs or diseases of the spine that go beyond osteochondrosis. These symptoms include: the appearance of BE in childhood and adolescence; back injury shortly before the onset of LBP; PB, accompanied by fever and signs of intoxication; PA not associated with spinal movements; unusual irradiation of pain: in the perineum, abdomen, rectum, vagina, both legs, girdle pain; connection of PB with eating, defecation, sexual intercourse, urination; concomitant urinary retention or incontinence; gynecological pathology (amenorrhea, dysmenorrhea, vaginal discharge), which appeared against the background of PB, strengthening of PB in the horizontal position and decrease in the vertical position (Razdolsky’s symptom, characteristic of a tumor process in the spine); steadily increasing pain over one to two weeks; development of paresis of the lower extremities against the background of BE, the appearance of pathological reflexes.
- Examination methods
— External examination and palpation of the lumbar region, identification of scoliosis, muscle tension, pain and trigger points. — Determination of range of motion in the lumbar spine, areas of muscle wasting. — Study of neurological status: determination of tension symptoms (Laseg, Wasserman, Neri); states of sensitivity, reflex sphere, muscle tone, vasomotor and autonomic disorders (swelling, changes in skin color). — X-ray, computer or magnetic resonance imaging of the lumbar spine; Ultrasound examination of the pelvic organs. — Gynecological examination. — If necessary, additional studies are carried out: cerebrospinal fluid, blood and urine, sigmoidoscopy, colonoscopy, gastroscopy, etc.
- Treatment
I. Acute BE (or exacerbation) of vertebral or myofascial origin.
A. Undifferentiated treatment. Gentle motor mode; in case of severe pain in the first days, bed rest, and then walking on crutches to unload the spine; hard bed: the best option is a wooden board with a thin mattress on top of it. For local warming, a woolen shawl, an electric heating pad, and a bag of heated sand or salt are recommended. Local exposure in the area of greatest pain: irritating ointments (phenalgon, tiger ointment, capsin, nicoflex, etc.), mustard plasters, pepper plaster, ultraviolet irradiation in an erythemal dose, leeches or irrigation with ethyl chloride.
Anesthetic electrical procedures (the means of choice are: transcutaneous electroanalgesia, sinusoidal modulated currents, diadynamic currents, electrophoresis with novocaine, etc.); acupuncture.
Novocaine blockades and pressure massage of trigger zones are used. Use analgesics, antihistamines, non-steroidal anti-inflammatory drugs, tranquilizers and/or antidepressants; drugs that reduce muscle tension (muscle relaxants): baclofen (5 to 20 mg three times a day) or sirdalud (1 to 4 mg three times a day). In case of arterial hypertension, sirdalud should be taken with great caution due to its hypotensive effect. If root swelling is suspected, diuretics are prescribed.
B. For discogenic radiculopathy, traction therapy (dry or underwater traction) is used in a neurological hospital.
B. For myofascial syndrome, after local treatment (novocaine blockade, irrigation with ethyl chloride), a hot compress is applied to the muscle for several minutes.
II. Chronic lumbar pain of vertebrogenic or myogenic origin.
In case of disc herniation, it is recommended to wear a rigid corset of the “weightlifter’s belt” type; limiting physical activity; exclusion of sudden movements, bends; physical therapy to create a muscle corset and restore muscle mobility; massage; novocaine blockades; acupuncture; physiotherapy: ultrasound, laser therapy, heat therapy. They use antidepressants, vitamin therapy: intramuscular B vitamins (B1, B6, B12), multivitamins with mineral supplements. For paroxysmal pain, Finlepsin (Tegretol) is prescribed. Psychotherapy is indicated.
In this article we do not touch upon issues of manual therapy and surgical treatment, which require special consideration.