Causes of the disease
Among the factors causing lipoarthritis of the knee joints are:
- Intense physical activity associated with professional activities. In this case, there is a constant force impact on the knee joints as a result of jumping, running, and sudden squats. Against the background of physical processes, the disease develops in athletes, ballet dancers, professional runners, and acrobats.
- Constant loads of moderate nature. The knees experience this type of impact during repetitive work, such as working in garden beds.
- Changes in hormonal balance. Degeneration of adipose tissue can develop in women during the premenopausal and menopausal periods. In this case, the pathogenesis is associated with the influence of hormonal changes on the ability of tissues to regenerate independently.
- Knee joint injuries. Significant traumatic impact can damage the pterygoid ligaments and cause meniscal rupture, which leads to hemorrhages into the adipose tissue and inflammation.
Normally, adipose tissue in the area of the knee joint ensures stability of the joint, reduces friction between the osteochondral elements, and evenly distributes the load on the legs. With constant physical activity, microdamage to adipose tissue is inevitable. Repeated hemorrhages and compression between the surfaces of the femur and tibia lead to an inflammatory process, hypoxia of the soft tissues of the knee, and impaired local circulation.
Although the inflammation is of aseptic origin, it is invariably accompanied by the accumulation of fibrin and hemosiderin. Macrophages begin an attack on the body's own fat cells in the area of the pathological focus. The result of these processes is the replacement of elastic adipose tissue with denser and coarser connective tissue - degeneration of the knee ridges develops.
Treatment
The basic principles of treatment for Hoffa disease are as follows:
- decreased proliferation activity in the area of the pterygoid folds;
- elimination of blockage by fatty bodies of the knee joint;
- elimination of inflammation;
- restoration of muscle function;
- restoration of leg support;
- restoration of motor stereotype.
In the early stages of lipoarthritis, the introduction of long-acting hormonal drugs into the area of the pterygoid folds of the knee joint can reduce proliferation and inflammation. If conservative treatment is insufficient, arthroscopic surgery “resection of the Hoffa fatty body” is performed - this is a method of radical treatment of the disease.
If you have any questions or make an appointment with a specialist, please call: (4852) 37-00-85 Daily from 8:00 to 20:00
Sign up for a consultation
Symptoms of the disease
In case of injury to the knee joints, the disease can develop rapidly. Most often, the pathological focus appears gradually, which means that symptoms do not appear immediately. From the moment of the first degeneration of adipose tissue until the manifestation of a specific clinic, a significant period of time can pass.
The first thing the patient feels is pain, which is localized in the anterior part of the knee joint. Painful sensations intensify during movements. Hoffa's disease is characterized by a dependence of pain on the position of the knee joint. When the leg is bent at the knee, the pain decreases, and when the leg is extended, it becomes more intense. Over time, the pain becomes intense at night.
When walking, squatting, or running, the patient feels a crunching sensation in the affected knee joint. Edema of the limb, swelling of the anterior and lower zones of the knee are visually determined. The longer Hoffa's disease develops, the greater the limitations in flexion and extension of the affected joint.
Patients note areas of bulging fatty tissue around the patella. When feeling the knee, a crunching sensation appears under the fingers on both sides of the patella.
Worsening of the pathological process leads to atrophy of the quadriceps femoris muscle (quadriceps). It can be moderate or significant, depending on the amount of fibrosis. After some time, patients present with gait disturbances and lameness.
Against the background of infringement of adipose tissue by the corresponding parts of the tibia and femur, a blockade of the knee joint may occur. Exacerbation of inflammation is the main factor in synovitis and gonarthrosis.
| HOFF'S KNEE DISEASE (diagnosis and treatment on an outpatient basis) |
Berglezov M.A., Ugnivenko V.I., Vyalko V.V.
The knee is a complex biomechanical system with a large number of anatomical structures contributing to its function. The knee ligaments are the main stabilizing component. No less important are the soft tissue auxiliary apparatus of the knee joint, including mucous bursae, fat bodies in the area of the pterygoid folds, menisci, as well as the functional state of the muscles that perform movements in the knee joint and stabilize it.
The clinical and radiological picture of degenerative-dystrophic, traumatic and inflammatory diseases of the knee joint creates difficulties in the differential diagnosis. In unclear cases, all types of pathology, especially in persons over 50 years of age, are combined under the collective diagnosis of “deforming arthrosis.”
Diagnosis of pathological processes of the knee joint can be difficult for a number of reasons, in particular, due to insufficiently careful clarification of the circumstances and mechanism of injury or onset of the disease, inattentive clinical examination of the joint and incorrect assessment of symptoms, insufficiently qualified interpretation of radiographs .
One of the undifferentiated symptoms of a number of diseases of the knee joint is pain, lameness, discomfort in the joint, crunching, swelling, limited mobility, contractures and deformities, true and false blockades of the joint.
The most common concomitant, complicating the course of deforming arthrosis, or independent diseases of the knee joint are the following: meniscopathy or chronic meniscitis, Hoffa’s disease, chronic synovitis of various etiologies with frequent strangulation of synovial villi, pigmented villous synovitis, bursitis or tendinosis in the lower pole area patella, external patellar compression syndrome with or without patellar subluxation, the presence in the cavity of the knee joint of free cartilaginous and osteochondral bodies of various origins (Golikova N.M., Ushakova O.A., 1988).
In complex cases, clinical and radiological examination is supplemented with arthropneumography and magnetic resonance imaging (MRI).
One of the objective methods for studying the knee joint is arthropneumography.
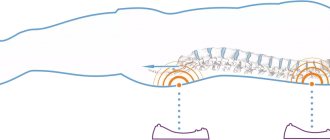
. The method of introducing oxygen into the knee joint is not complicated and consists of puncture of the knee joint with a thin needle, followed by slow injection under a pressure of 120 mm. rt. Art. medical oxygen in a volume of 60 to 120 ml. An X-ray is taken within the next 10 to 15 minutes after the procedure. An x-ray in a lateral projection is especially informative. The arthrography technique of the knee joint makes it possible to assess the condition of the joint capsule and the presence of so-called Becker cysts (Funke K., 1981; Ricklin P., 1964). The image shows: the oxygen-filled upper and posterior inversions of the synovial bursa, the state of the area of the pterygoid folds (Fig. 1), which is a fairly reliable diagnostic sign in the case of hypertrophy of the Hoffa fatty bodies (N.M. Golikova, 1975, 1979).
Figure 1. Arthropneumogram of the knee joint is normal (after administration of oxygen at a pressure of 100 mm Hg). The superior inversion (A) is well defined. Contours of Hoffa bodies (B) without signs of hypertrophy.
Before the advent of magnetic resonance imaging, assessment of knee function and morphology was limited to physical examination, arthrography, and computed tomography. MRI image analysis techniques
With its unique ability to depict soft tissue components, it has revolutionized the assessment of the ligamentous and soft tissue apparatus of the knee joint (Nicholas JA, Frieberger RH, Killoran PJ, 1970; Brown DW, Allman FL Jr, Eaton SB, 1978; Crabtree SD, Bedford AF, Edgar MA, 1981 ; Thijn CJP, 1982; Selesnick FH, Noble HB, Bachman DC, 1985). The most easily assessed image is in the sagittal plane.
An MRI of the anterior inferior knee joint shows a thin layer of subcutaneous soft tissue, followed by an accumulation of fat called the fat pad prepatellaris or Hoffa bodies. The most localized area of signal intensity is normally determined under the lower pole of the patella, which should not be considered a pathological condition (El-Khoury GY, Wira RL, Berbaum KS, et al, 1992). The signals from the internal and external menisci are connected by the ligament of Winslow (Watanabe AT, Carter BC, Teitelbaum GP, et al, 1989). Hoffa fatty bodies are distinguished on MRI by size and intensity of manifestation (Fig. 2).
Figure 2. MRI of the knee joint in the sagittal plane. Goff bodies.
Hoffa's disease, lipoarthritis or chronic inflammation of fatty tissue in the area of the pterygoid folds
- Hoffa's bodies of the knee joint against the background of its hyperplasia, often accompanied by pinching it between the articular surfaces of the bones and blocking the knee joint. According to the ICD (1996), it corresponds to code 272.8 of the section “Other disorders of lipoid metabolism Hoffa's disease or liposynovitis prepatellaris Launois-Bensaude's lipomatosis Lipoid dermatoarthritis”
In 1904, A. Goffa described a disease of the pterygoid fold of the knee joint, which currently bears his name. “I discovered this disease during surgery on the knee joint, when I suspected the presence of a damaged meniscus. But when the joint was opened, the menisci turned out to be intact. However, I noticed extensive hyperplasia of fatty tissue under the patellar ligament. This observation showed that we are dealing with a very typical picture of the disease. If we dissect a healthy knee joint, then under the patellar ligament we will see two pterygoid and one synovial folds. The first are represented by adipose tissue, which is covered with a synovial membrane, reminiscent of a soft lipoma, spreading from the anterior edge of the tibia into the joint cavity.... Thus, we are talking about a characteristic disease, which is best described as inflammatory hyperplasia of adipose tissue with germination its dense fibrous connective tissue.
This inflammatory process, since there are no other etiological factors, is usually associated with injury. The hypertrophied cord is further pinched between the mice of the femur and tibia, which is a new stimulus for aggravating the inflammation process.
When examining the patient, a characteristic objective symptom is noticeable - more or less pronounced atrophy of the quadriceps femoris muscle. You can almost always see the typical swelling of the knee joint deep under the patella and on either side of it. This pseudo-fluctuating bulging raises the patellar ligament. The upper inversion of the joint is free, and the joint space on the sides remains free. If we palpate the knee joint along the lateral surfaces of the kneecap, we will feel a dough-like bulge that goes under the patellar ligament. I believe that extription of fat mass will allow many patients to be cured of long-term symptoms that could not be eliminated by external applications, baths, or other means used” (Hoffa, 1904 cited by K. Bashurov, 1995 ). This classic description of the disease should be included in major medical reference books.
Chronic inflammation and degeneration, known as Hoffa disease, occurs within the prepatellar fat pad. Uniform hypertrophy can lead to blockage of the fatty tissue between the femur and tibia. Diagnosis is usually made arthroscopically (Ogilvie-Harris DJ and J. Giddens, 1994).
According to modern literature, the treatment of chronic inflammation of fatty tissue and blocking of the knee joint is predominantly surgical and consists of excision of fatty bodies in the area of the anterior part of the knee joint.
Hoffa syndrome often occurs in young people as a result of direct trauma to the anterior knee joint and is usually accompanied by clinical meniscus damage. Arthroscopy performed in such cases is a method of radical treatment of this disease. However, the greatest problem in outpatient orthopedics is presented by patients of middle and older age groups, whose surgical treatment is undesirable for various reasons.
The research and outpatient department of the CITO analyzed the results of the study and treatment of 72 patients aged 35 to 65 years with the syndrome of chronic inflammation of fatty tissue in the area of the pterygoid folds of the knee joint and severe dysfunction of the joint. All patients had previously undergone long-term and unsuccessful treatment with anti-inflammatory drugs, including intra- and periarticular injections of corticosteroids, for arthrosis deformans or meniscus damage. Severe pain syndrome, impaired support and stability of the leg caused by blockade of the knee joint, hypotrophy and decreased function of the leg extensor muscles caused severe dysfunction of the lower extremities (lameness, inability to use public transport, the need for additional support on a cane...). The onset of the disease is “acute”: pain and limitation of extension in the knee joint after a minor injury, prolonged pressure on the anterior region of the knee joint (“crawling on one’s knees”) or for no apparent reason. The course of the disease is chronic and progressive from 2 to 8 months. Night pain is typical 1 to 3 months after the onset of the disease.
According to our observations, Hoffa's disease most often occurs in pre- and postmenopausal women aged 45 to 65 years, which indicates an obvious connection between hyperplasia of the fatty tissue of the knee joint and hormonal imbalance.
All patients had a characteristic clinical picture: incomplete extension of the joint without obvious involvement of the menisci and ligamentous apparatus, swelling of the joint in the anterior-lower section, pseudofluctuating crepitant formation on both sides of the patellar ligament, hypothorophia, decreased function of the 4-headed femoral muscle and its internal head, functional instability of the knee joint. Among all cases of severe dysfunction of the lower extremities caused by orthopedic pathology, severe dysfunction caused by Hoffa's disease, Hoffa's disease accounts for 12%, which indicates not only the prevalence of this pathology, but also the severity of its course.
An X-ray examination revealed signs of arthrosis of the knee joint of stages I-II according to N.S. Kosinskaya, which was probably the basis for the erroneous diagnosis. Arthropneumograms revealed characteristic changes: a decrease in the volume and rigidity of the superior inversion of the knee joint, an increase in the volume of the posterior inversion with the development of a hernial protrusion into the popliteal region - Becker cysts, hypertrophy of fatty tissue in the area of the lower pole of the patella with its introduction between the femur and tibia (Fig. 3 ). Often, X-ray photographs reveal calcium deposits in the area of the pterygoid folds—calculous bursitis.
Figure 3. Arthropneumograms of the knee joint of patients with Hoff's syndrome. Hypertrophy of the fat bodies in the area of the pterygoid folds (A), a decrease in the volume and rigidity of the superior inversion of the knee joint, an increase in the volume of the posterior inversion, a cyst in the popliteal region (Becker’s cyst).
MRI of the knee joint in Hoffa's disease has a characteristic appearance. There is hypertrophy of the fatty bodies in the area of the pterygoid folds. “Introduction” of hyperplastic adipose tissue into the joint space (Fig. 4). When performing a biopsy and cytological examination of the area of the pterygoid folds, hyperplasia of adipose tissue and signs of inflammation are revealed.
Figure 4. MRI of the knee in Hoffa's disease. Hypertrophy of fat bodies in the area of the pterygoid folds. “Incorporation” of hyperplastic adipose tissue into the joint space.
Treatment of Hoffa syndrome of the knee joint on an outpatient basis.
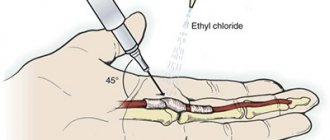
The main pathogenetic principles of treatment of Hoffa's disease are the elimination of blocking of the knee joint by fatty bodies, the elimination of inflammation and the reduction of proliferation activity in the area of the pterygoid folds, as well as the restoration of muscle function, support and stability of the leg and motor stereotype. A comprehensive treatment method for Hoffa's disease, including intra-articular oxygen therapy, local application of corticosteroids, laser therapy, methods for restoring muscle function, has been developed and used in CITO since 1984 (Berglezov M.A. et al., 1987). The technique of intra-articular oxygen therapy has been used in CITO since 1963. For the first time, S.L. Tregubov reported about the successful injection of medical oxygen for deforming arthrosis and tuberculous synovitis in 1908. The pathogenetic substantiation of the use of oxygen in degenerative-dystrophic diseases of the joints was carried out using biochemical studies (N.M. Golikova, 1979). Under conditions of oxygen deficiency, glycolysis in the joint tissues increases, resulting in the accumulation of under-oxidized metabolic products: lactic and pyruvic acids. Their oxidation requires increased oxygen delivery to the joint tissue. In addition, the introduction of oxygen, which stretches the joint capsule and creates an unloading “gas” cushion, leads to mechanical removal of the joint blockade, “squeezing out” the restrained Hoffa bodies from the joint space area. Administration of long-acting corticosteroids to the area of the pterygoid folds of the knee joint can reduce the phenomena of inflammation and proliferation. The use of monochromatic red laser radiation (laser therapy) allows you to obtain a lasting positive effect. From the anterior internal approach towards the articular surface of the lower pole of the patella to a depth of 4-5 cm, a needle is inserted through which 1.0 diprospan or Kenalog is injected (the area of the pterygoid fold). Then the needle is advanced in the posteroproximal direction until a sensation of “failure” is felt and 50-120 ml of oxygen is injected intra-articularly. To achieve the desired result, 1-3 injections are sufficient with an interval of 1 week. The treatment is complemented by laser therapy sessions conducted daily No. 15. The patient is recommended to undergo therapeutic exercises (strengthening the leg extensor muscles in isometric mode), walking with a roll over the forefoot. If necessary, a course of electrical myostimulation is carried out, including multi-channel electrical stimulation of muscles while walking. The effectiveness of treatment was assessed in the short and long term (up to 5 years). Blockade and inflammation of the knee joint area was achieved in all patients. Recurrence of Hoffa's disease was observed in 20% of patients who underwent a second course of treatment. However, in no case was there a need for surgical treatment. Hoffa's disease is a common and severe pathology of the knee joint. 12% of severe dysfunctions of the lower extremities are caused by this particular pathology. Diagnostic errors are associated with the fact that the disease often occurs against the background of arthrosis of the knee joints, as well as with insufficient awareness of doctors about Hoffa’s disease. Clinical examination, arthropneumography, MRI examination of the knee joint allows us to establish a diagnosis with high reliability. The method of complex treatment of Hoffa's disease, including intra-articular oxygen therapy, local use of corticosteroids, laser therapy, and exercise therapy, allows for effective assistance to patients and should be widely used in outpatient settings.
Literature:
1. Bashurov K. — Hoffa’s disease of the knee joint. Traumatology and Orthopedics of Russia No. 4 1995 p. 89-91 2. Berglezov M.A., Vyalko V.V., Golikova N.M., Ugnivenko V.I. Laser radiation in the treatment of severe dystrophic injuries of the knee and hip joints. Soviet medicine. No. 7, 1987. 3. Golikova N.M. Our experience of intra-articular oxygen therapy for patients with deforming arthrosis of the knee joint in a clinic setting. Organization of outpatient care for patients with trauma and diseases of the musculoskeletal system in Moscow. CYTO. 1979, p. 109-113. 4. Golikova N.M., Ushakova O.A. Differential diagnosis of diseases of the knee joint. In: Age-related, adaptive and pathological processes in the musculoskeletal system. Abstracts of reports of the VII school on muscle biology (Kharkov, June 8-10, 1988). P.188-190 5. Franke K. Sports traumatology. Translation from German. M., Medicine, 1081, p.238 6. Blencke A. Albert Hoffa // 2. Orthop. - S. 7-11. 7. Brown DW, Allman FL Jr, Eaton SB: Knee arthrography: a comparison of radiographic and surgical findings in 295 cases. Am J Sports Med 6:165–172, 1978 8. Crabtree SD, Bedford AF, Edgar MA: The value of arthrography and arthroscopy in association with a sports injury clinic: a prospective and comparative study of 182 patients. Injury 13:220-226, 1981 9. El-Khoury GY, Wira RL, Berbaum KS, et al: MR imaging of patellar tendinitis. Radiology 184:849-854, 1992 10. Hoffa A. Zur Bedeutung des Fettgewebes Kniegelenks // Deut. Med. Wnschr. - 1904. -S. 337-338; N 11.-S. 388-390. 11. Nicholas JA, Frieberger RH, Killoran PJ: Double-contrast arthrography of the knee: its value in the management of two hundred and twenty-five knee derangements. J Bone Joint Surg Am 52:203-220, 1970 12. Ogilvie-Harris DJ and J Giddens. Arthroscopy Vol 10. p 184-187. 1994. 13. Paul U. Albert Hoffa // Zbl. Chir.-1981.-Jg. 106. N 13. - S. 901-903. 14. Riclin P., Ruttimann R., del Buono MS: Die Meniskuslation. Thieme, Stuttgart, 1964. 15. Schani A. Albert Hoffa // Zbl. Chir. -fur Pathologie des - Jg. 30, N 10. -1908. —Bd. 20.-1908. —Jg. 35, N3.-S. 1-3. 16. Selesnick FH, Noble HB, Bachman DC, et al: Internal derangement of the knee: diagnosis by arthrography arthroscopy, and arthrotomy. Clin Orthop 198:26-30, 1985 17. Spitly. Albert Hoffa // Munch, med. Wnschr. - 1908. - Jg. 55, N 5.-S. 237-239. 18. Thijn CJP: Accuracy of double-contrast arthrography and arthroscopy of the knee joint. Skeletal Radiol 8:187–192, 1982 19. Watanabe AT, Carter BC, Teitelbaum GP, et al: Normal variations in MR imaging of the knee: appearance and frequency. AJR 153:341-344, 1989
Hoffa's disease in children
Hoffa's knee disease in children is rarely diagnosed, since in childhood there are practically no main risk factors for this pathology. The disease can develop in a child as a result of injury to the knee joints.
After a short period of time, the child develops characteristic symptoms:
- pain in the injured knee;
- limitation of joint mobility;
- swelling of the knee and surrounding soft tissues.
When trying to bend or straighten the damaged knee joint, the child feels an internal crunch. In parallel with this, there is a limitation of mobility, the inability to fully straighten the leg at the knee.
Prevention
You can avoid Hoffa's disease by following simple rules:
- avoid heavy loads on the joint;
- compliance with safety regulations, prevention of injuries and damage;
- use of protective devices when playing sports and while working;
- wearing comfortable, stable shoes;
- timely treatment of chronic pathology.
For the purpose of prevention, do not forget that you need to normalize body weight, eat and sleep properly, normalize hormonal levels, and also give up bad habits. All this improves microcirculation and metabolic processes in tissues.
To prevent a complicated pathological process, timely correct diagnosis of the disease is important, which allows for effective conservative therapy and avoidance of surgical intervention.
Diagnostics
Diagnosis of Hoffa's disease is carried out by orthopedic traumatologists. Establishing a correct diagnosis is important for determining therapeutic tactics. First of all, a complete history taking is important. The hormonal status of a woman after 45 years of age is clarified. In young patients, the nature of professional activity, the fact of sports loads, and previous injuries are determined.
To determine the condition of the knee joints, a comprehensive examination is prescribed:
- MRI. MRI images visualize the structure of soft tissues and ligaments of the articulation. In the case of lipoarthritis, pronounced hypertrophy of prepatellar adipose tissue is determined. The greatest intensity is localized above the lower pole of the patella. Foci of fibrin and hemosiderin are identified.
- Arthropneumography. Used when it is impossible to perform MRI. To obtain complete information, a lateral photograph of the knee joint is taken. The images determine the boundaries of adipose tissue, its hypertrophy, and the presence of calcifications in the pterygoid ligaments.
- Ultrasound. Shows the condition of soft tissues, disturbance or preservation of local blood flow.
- Arthroscopy. Minimally invasive surgery on the knee joint is performed for acute injuries (sports, work injuries), in case of suspected meniscus tear.
The data obtained during hardware diagnostics is carefully analyzed to avoid making an erroneous conclusion. It is important to differentiate Hoff's disease from ruptures of intra-articular ligaments, deforming arthrosis, bursitis, and synovitis.
Operation
When conservative treatment methods do not work, surgical intervention is prescribed. Arthroscopy is a minimally invasive operation in which several punctures are made through which an instrument and camera are inserted. With minimal blood loss and a slight risk of complications, excess Hoffa tissue is excised, swelling and inflammation go away.
In most cases, surgical intervention takes place without complications, and the functionality of the joint is completely restored. After manipulation, small scars remain on the knee due to the insertion of an endoscope through a small incision. Full recovery occurs within a few weeks.
Recovery and rehabilitation after Hoffa's disease
- The postoperative rehabilitation period is only three to four weeks.
- Regenerative physiotherapy and physical therapy are carried out, and any stress on the knee is excluded.
- Experts recommend spending your rehabilitation time in a sanatorium, where you can undergo massage, exercise therapy, physiotherapy, and mud treatment.
- Resorts with iodine-bromine, sulfide and radon waters will contribute to a speedy recovery.
About age and profession
Hoffa syndrome occurs in both children and adults, but is most often diagnosed in women
over 45 – 55 years old. Most likely, the hormonal imbalance associated with menopause is to blame for the changes. The pathology is also characteristic of people who subject their knees to heavy loads - these are professional athletes, as well as representatives of professions whose work involves long periods of squatting or kneeling, for example, work in landscaping or agriculture.