Arthritis
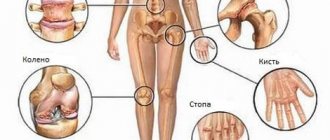
is a generalized name for inflammatory diseases, the localization of processes of which can occur in any joint of the human body. One of the most common types of pathological process is considered to be arthritis of the hands.
An interesting fact is that the disease occurs more often in women, which is explained by the characteristics of everyday and professional activities.
Arthritis of the hands is a disease that leads to degeneration and gradual destruction of the joints
What is hand arthritis?
Arthritis of the hands
is a degenerative-dystrophic disease, the development of which occurs in a situation of increased loads on the joints of the hands and injuries to the upper extremities.
The human hand consists of small bones connected to each other into joints:
- wrist;
- carpometacarpal;
- metacarpophalangeal.
It is worth noting that in the area of the carpal joints there is a large number of blood vessels and nerve endings, which causes increased pain in pathological processes.
Rheumatoid arthritis of the hands
can occur and develop in a person of almost any age and gender. Progress is characterized by the presence of inflammation, the disease is predominantly secondary.
The occurrence of arthritis of the hands
often occurs in adolescence and is accompanied by serious deformities. No less often, pathology occurs in adulthood, when hormonal changes occur in the body. In addition, the disease can be caused by sports, household, and professional injuries.
Lack of quality treatment for arthritis of the hands can lead to disability.
Diagnosis of the disease
Based on a biochemical blood test , changes in the joints visible on x-rays , and the use of basic clinical markers . A blood test examines ESR, rheumatoid factor, platelet count, etc. The most progressive analysis is the titer of antibodies to cyclic citrulline-containing peptide - ACCP, anti-CCP, anti-CCP. The specificity of this indicator is about 90%, while it is present in 79% of sera from RA patients.
Diagnostically important clinical features are the absence of changes in skin color over the inflamed joints, the development of tenosynovitis of the flexors or extensors of the fingers and the formation of amyotrophies, typical deformities of the hands, the so-called “rheumatoid hand”.
The criteria for an unfavorable prognosis are:
- early damage to large joints and the appearance of rheumatoid nodules;
- swollen lymph nodes;
- involvement of new joints during subsequent exacerbation;
- systemic nature of the disease;
- persistent increase in ESR;
- early appearance (during the first year) and high titers of rheumatoid factor;
- early (up to four months) radiological changes in the affected joints - rapid progression of destructive changes;
- detection of antinuclear antibodies and LE cells;
- carriage of HLA-DR4 antigens; poor tolerability of basic drugs.
In the treatment of rheumatoid arthritis, systemic drug therapy with various groups of drugs is used.
Causes of rheumatoid arthritis of the hands
Among the most likely causes of pathology localized in the wrist joints, it is customary to highlight:
- age characteristics
– in particular, mechanical damage and hormonal changes;
- injuries received
– leave damage on the joint, the likelihood of inflammation of which is quite high;
- features of professional activity
– a particularly relevant reason for people whose fingers and hands are under constant tension;
- heredity
– genetic predisposition is a fairly high risk factor;
- reduced immunity
– a decrease in the body’s protective function can lead to various types of diseases;
- infectious diseases
– localization of infection in the joint capsule provokes the development of a strong inflammatory process.
In addition, allergic reactions, constant stress and diseases such as rheumatism, diabetes, etc. are also considered to be indirect causes of the disease.
Symptoms of hand arthritis
To understand how to treat arthritis of the hands
, it is necessary to understand
what symptoms the pathology has
.
The symptoms of degenerative-dystrophic processes may vary, depending on the reasons for their occurrence. Common symptoms of hand arthritis include:
- pain experienced when performing various actions with the upper limbs;
- “torsion” of the joints of the hands due to changing weather conditions and changes in atmospheric pressure;
- decreased mobility and stiffness of joints, which manifests itself mainly in the morning;
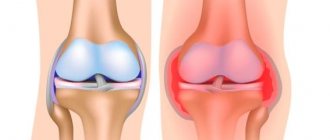
- the appearance of redness, locally elevated skin temperatures and swelling on the knuckles;
- symmetrical damage to joints by inflammatory processes;
- crunching and squeaking (crepitus) when moving your fingers;
- formation of subcutaneous nodules.
In rare cases, symptoms of arthritis of the hands include weight loss, as well as increased fatigue and general weakness of the body, caused by the presence of inflammatory processes in the body.
Caption: Symptoms of arthritis of the hands affect the course of treatment of the disease
Stages of development of hand arthritis
Today, there are several stages of development of arthritis of the hands, each of which has special symptoms:
First stage
Most of the symptoms are absent, however, already at this stage of development of the pathology you can seek medical help.
The only thing. What the patient may notice is strong, but short-term stiffness.
Second stage
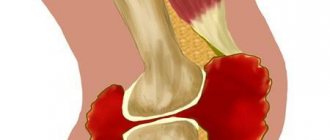
The occurrence of bone erosion, the signs of the disease become brighter. Joint pain appears and stiffness is present throughout the day.
Third stage
There is a symmetrical deformation of the joints, local redness and increased temperature, pain intensifies and does not go away without taking painkillers.
Fourth stage
Pathological processes in articular tissues reach their peak, cartilage tissues grow together, finger movements become impossible. A person receives the status of “disabled person” due to the loss of the ability to self-service.
Arthritis of the fingers
What is hand arthritis | Causes of hand arthritis | Symptoms of arthritis in fingers | Treatment of hand arthritis at Doctor Ost MC
Arthritis of the fingers can be acute or chronic. And if acute arthritis occurs suddenly, literally in one day the main symptoms of the disease begin to appear, then chronic arthritis of the hands develops slowly, gradually.
The inflammatory process can begin in any joint. The hands are the most susceptible to arthritis. The vulnerability of these joints is due to their small size.
Sign up
Arthritis of the fingers, like arthrosis of the hand, was previously considered an age-related disease. It affected people over 50 years of age, mainly women during the period of active hormonal changes in the body (after childbirth, during menopause). Today, this bar has dropped significantly and arthritis of the hands is diagnosed in quite young people and even in children during puberty.
CAUSES OF ARTHRITIS OF THE HAND
There are several main factors that provoke the inflammatory process in the joints:
- various infections. This can be either a common respiratory virus or a serious infectious disease (tuberculosis, gonorrhea, chlamydia, syphilis, etc.). The main causative agents of infectious arthritis of the fingers are streptococci and staphylococci;
- metabolic disorders, autoimmune failure provoke rheumatoid arthritis of the hands, affecting both limbs symmetrically;
- prolonged excessive activity of the hands associated with professional necessity (pianists, painters);
- consequences of injuries, bruises, surgical operations;
- other diseases, such as diabetes;
- hereditary factor. Direct heredity of hand arthritis has not been scientifically proven; however, the pathological condition of the joints can be transmitted from parents.
It is important to note that arthritis of the hands does not only affect the interphalangeal or wrist joints. As a rule, this disease is systemic. Internal organs are also affected (respiratory, genitourinary systems, kidneys, liver, etc.). And these organs require mandatory rehabilitation in the treatment of hand arthritis.
Arthritis of the fingers is a provocateur of arthrosis of the hand. Without treatment, the inflammation will go deeper, the pathological degenerative process will also affect other joints, the bones will be deformed, and growths will form on them. This condition can lead to complete loss of limb mobility.
SYMPTOMS OF ARTHRITIS OF THE FINGERS
- Pain is the main symptom of finger arthritis. At the initial stage, the pain may be mild and aching. In severe cases, the pain is unbearable and requires the use of analgesics.
- Also symptoms of hand arthritis: numbness, aching, tingling, distinct creaking, swelling and redness of the skin in both the fingers and the wrist. With rheumatoid arthritis, body temperature may rise, general malaise, and a feeling of constant fatigue may appear.
- The main signs of arthritis of the hands appear at stages 2 and 3 of the disease - ugly deformation of the fingers and hands.
The deformity can take different forms depending on the type of arthritis: the fingers can become completely swollen, as if “bloated” (the skin becomes red and swollen), peculiar interphalangeal nodules - bumps - can appear, the fingers can completely “curl”, as in one direction , and in different ones. At this stage, it becomes difficult for the patient to perform basic actions: fasten buttons, hold a mug, etc.
Ask a Question
One of the differences between arthritis and arthrosis of the hand is when the main symptoms appear. With arthritis, pain, aches and stiffness of movement occur in the morning, immediately after waking up or after a long period of rest. With arthrosis, the joints hurt and are bothersome mainly at night. With arthritis of the hands, the pain syndrome may decrease during physical work; with arthrosis of the hands, the pain will only intensify.
“The pain in my knees forced me to go to the hospital. Based on reviews, I chose “Doctor Ost” and after the first laser therapy procedure I began to sleep more peacefully, the swelling in my knees decreased.” Read full review
TREATMENT OF ARTHRITIS OF THE HAND AT MC "DOCTOR OST"
It is important to diagnose arthritis of the fingers at an early stage, before changes in the joints begin. It is necessary to establish not only the presence of arthritis itself, but also the root cause of the disease.
It is unacceptable to make a diagnosis and prescribe treatment on your own. The treatment protocol for the two diseases, arthritis and joint arthrosis, is significantly different. The use of anti-inflammatory drugs for arthritis will have a therapeutic effect; for arthrosis, it will only intensify the process of joint destruction.
When treating arthritis of the hands, the first step is to eliminate the cause, then the emphasis is on physical therapy (magnetic therapy, UHF, ultrasound treatment, paraffin and mud baths, etc.). Such a systematic approach requires constant monitoring by a doctor.
Middle-aged and older people, as well as people with constant professional stress on their hands, need to be examined at least once a year for the presence of arthritis or arthrosis of the joints. And at the first symptoms (tingling, numbness, squeezing effect like wearing tight gloves), immediately seek help.
Doctor Ost MC has advanced technologies for treating joints of varying severity. Preference is given to hardware treatment methods that can reduce the harmful drug load on the excretory system.
At the Doctor Ost MC we are ready to relieve even acute joint pain during the first treatment session. A full course of treatment stimulates the active restoration of destroyed cartilage tissue and can cancel the most complex operation to replace a worn-out joint.
how much does it cost? Treatment of arthritis of the fingers at Doctor Ost is carried out by a rheumatologist and orthopedist. The cost of consultation with a specialist is indicated in the “Consultative appointment” section of our price list. Follow the promotions, don't miss out on the best price!
Types of arthritis of the joints of the hand
According to the existing classification, there are several most common types of arthritis of the hands:
- infectious (caused by infections);
- metabolic (caused by the accumulation of uric acid salts);
- rheumatoid (starts mainly in small joints);
- post-traumatic (the result of damage to cartilage tissue);
- proximal, middle or distal;
- rhizarthritis (affects exclusively the thumb);
- secondary arthritis.
Prognosis for the treatment of arthritis of the hands
The prognosis for the treatment of arthritis of the joints of the hands is largely determined by the stage at which the pathological process was diagnosed.
With timely detection of the disease (in the initial stages of development), accurate diagnosis and determination of the most effective, strictly followed treatment plan, the prognosis for recovery is as favorable as possible.
It is worth noting that even if it is impossible to fully overcome the disease, the patient may experience a stable remission of rheumatoid arthritis of the hands, allowing him to live and work fully. Free joint mobility is maintained for a long period.
Thus, we can come to the conclusion that the prognosis of degenerative-dystrophic processes largely depends on the time of seeking medical help and the quality of implementation of medical recommendations.
Therapeutic exercise for rheumatoid arthritis
The rate at which rheumatoid arthritis develops varies from person to person and will be characterized by periods of remission and worsening of symptoms. In most cases, there is no obvious cause of the disease.
rheumatoid arthritis: causes and symptoms
There are a huge number of symptoms of this disease. The main ones include:
- joint pain.
- Painful sensations in the muscles.
- Change in skin color.
- Minor deformation of nails.
- Lack of desire to eat.
- Mild fever.
- Development of small and mobile lumps under the skin (rheumatoid nodules).
The symptoms of this disease should not be confused with those of the flu. They may be similar, since rheumatoid arthritis is a systemic disease. By starting treatment prematurely, severe symptoms can be avoided.
The main factors in the development of the disease include:
- Genetic factor (the disease is inherited).
- Infectious factor (weak immune system).
- Lifestyle factor (presence of bad habits).
- Hormonal factors (lack of or changes in hormones).
Description of exercise therapy
Physiotherapy is a medical discipline that uses physical activity performed by patients to treat diseases. After exercise therapy, patients experience a surge of strength and vigor, as well as a decrease in stiffness and pain in the affected areas.
It must be prescribed to patients by the attending physician. Typically, exercise therapy consists of various gymnastic exercises, walking and swimming. These procedures can also be supplemented with massage sessions, which allow you to relax after training.
Hand exercises for rheumatoid arthritis
Rheumatoid arthritis can affect the joints of the fingers, which may become deformed. To prevent the disease and get rid of hand changes, you need to follow the following things:
- Try not to move your fingers towards your little finger.
- Don't put too much stress on your fingertips.
- During sleep, use special devices to immobilize the limb (orthoses).
- Hold your hands correctly at rest.
- Try not to tilt your joints in different directions.
There are several sets of exercises for hand lesions. Here is an example of some exercises from the best complexes:
- Place your hands in front of you and begin to turn them up and then down.
- Place your hands on a hard surface and begin to lift your hands.
- Place your hands on a hard surface and begin to raise your fingers.
- Place your hands clenched into a fist in front of you and begin to turn them clockwise and then counterclockwise.
- Place your elbows on a hard surface, and then begin to bring them in and out. During this exercise, your hands should be clenched into a fist.
- Rub your palms together.
All complex exercises must be performed five to seven times, but if pain occurs, you must stop training, as this can lead to complications of the disease. In general, the number of repetitions in the exercises largely depends on the patient’s condition.
Leg exercises for rheumatoid arthritis
Exercise therapy can also help with immobilization of leg joints. Here are some good exercises to do this:
- "Sliding steps."
- "Bike".
- An exercise in which you need to bend your knees and spread them in different directions.
- Circular movements with a straight leg.
- Spreading your legs in different directions. While performing this task, you must be in a lying position.
All these exercises must be performed while maintaining the correct breathing rhythm.
Exercises for shoulder injuries
The main exercises for this disease are:
- Raising and releasing the shoulders.
- Circular movements of the shoulders.
- Hugging yourself.
- Raising and releasing the elbows, previously clasped by the palms.
They can help you relieve shoulder pain.
Ankle exercises for rheumatoid arthritis
Rheumatoid arthritis rarely affects the ankle joint, but such cases also occur. They can lead to disability.
To prevent rheumatoid arthritis in such cases, it is recommended to perform the following exercises:
- Stand on your toes, leaning on something (for example, a wall).
- Roll a round object (for example, a ball) with your feet.
- Make circular movements with your feet.
Tips for performing medicated exercise
There are a few simple tips for more successful physical therapy.
- Exercise therapy should be performed daily, without shirking your training. During exercises, do not forget about proper breathing. Try to stick to the right rhythm.
- If the exercises you do become too easy, try increasing the load by increasing the number of sets for each exercise. This should add some challenge to the activity.
- Don't despair if you find yourself with rheumatoid arthritis. It can be destroyed by daily training. This is not at all difficult to do.
- After completing your workouts, conduct a muscle relaxation session.
By following these tips, you will increase the speed of your recovery and eliminate some of the bad symptoms of the disease.
Rheumatoid arthritis is a fairly serious disease, but it can be cured. Physical therapy is one of these methods. It must be prescribed by a specialist.
With timely treatment, the development of quite severe symptoms can be prevented.
To do this, you need to periodically undergo diagnostics. Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Treatment of hand arthritis
Only a specialist can determine how to treat arthritis of the hands, after conducting a thorough diagnosis and reviewing the patient’s medical history.
Today, there are several effective methods for treating pathology. Let us consider in detail the most effective of them.
Medicines
Use of medications
– an integral condition for the treatment of arthritis of the hands, which is due to the systemic occurrence of pathological processes involving a large number of joints.
By adhering to a specific drug regimen, drug treatment can alleviate the symptoms of the disease and reduce side effects to a minimum.
Treatment with medications involves taking such groups of drugs as:
- NSAIDs
– non-steroidal anti-inflammatory drugs that help relieve inflammation and swelling, as well as reduce pain, improving the patient’s overall well-being;
- systemic antibiotics
– prescribed for infectious-bacterial etiology of the lesion;
- vitamin and mineral complexes
– optimize the nutrition of joint tissues.
In addition, to improve metabolic processes and accelerate regenerative processes, the patient is prescribed chondroprotectors. One of the most effective among them is considered to be the drug "Artracam"
.
Treatment of hand arthritis
Physiotherapeutic procedures
Use of physiotherapeutic procedures
due to the need for an integrated approach to the treatment of diseases. Prescribing physiotherapy makes it possible to help improve regenerative and metabolic processes in the tissues of the affected joint, as well as slow down or completely stop the destructive effect of the disease.
The joints of the hands are located quite close to the skin, which determines the greatest effectiveness of ultrasound treatment, the use of electrophoresis, as well as specialized massage or acupuncture.
Therapeutic physical education (PT)
Exercise therapy
- this is a special area of physical activity, the key goal of which is to activate blood flow and metabolic processes within the tissues of the affected joint.
A set of specialized exercises is determined by the attending physician, in accordance with the dynamics of improvements and the characteristics of the course of the disease at a particular point in time. Each exercise helps develop mobility in the fingers and hands.
IMPORTANT! Exercise therapy is permissible only during the period of remission, which will eliminate the possibility of harm to health.
Joint replacement
In advanced cases of pathology, arthritis is treated through surgery, in particular, through endoprosthetics of the joints of the fingers.
The main goal of this type of surgical intervention is to restore the functionality of the hands and improve the quality of human life.
Rheumatoid arthritis. Symptoms of rheumatoid arthritis
Rheumatoid arthritis is one of the most severe joint diseases, occurring with many complications. Rheumatoid arthritis affects people of all ages, but most often those over 30. Among women, about 5 times more suffer from rheumatoid arthritis than among men. In general, according to various scientists, this disease affects 1-2% of the population.
Symptoms of rheumatoid arthritis
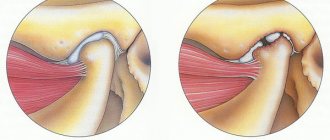
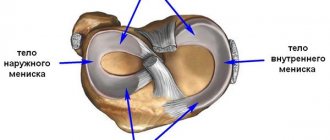
The symptoms of rheumatoid arthritis are difficult to confuse with the symptoms of other joint diseases. In the vast majority of cases, at the onset of the disease, inflammation and swelling of the metacarpophalangeal joints of the index and middle fingers occur. We are talking about the joints located at the base of these fingers, that is, in the area of \u200b\u200bthe protruding bones of a clenched fist. This inflammation of the metacarpophalangeal joints is most often combined with inflammation and swelling of the wrist joints. And sometimes the wrist joints become inflamed and swollen first.
What is characteristic is that inflammation of the joints in rheumatoid arthritis is almost always symmetrical - that is, if the joints on the right hand are affected, then the same joints on the left hand are almost certainly affected. And, unlike rheumatism, with rheumatoid arthritis the inflammation in these joints is persistent, swelling and pain in them last from several months to several years.
Joint pain with rheumatoid arthritis intensifies most often in the second half of the night, in the morning. Until about noon the pain is very intense; patients compare them to toothache. However, in the afternoon the pain becomes weaker, and in the evening it is often insignificant. What is also characteristic is that at the beginning of the disease, joint pain often decreases after active movements or warm-up. And they do not get worse from stress, as happens with arthrosis. However, any relief from rheumatoid arthritis usually lasts only until the middle of the night, and around 3-4 hours the attacks of joint pain resume.
Along with inflammation of the joints of the upper extremities, rheumatoid arthritis almost always affects the small joints of the feet. The joints at the base of the toes become inflamed, which manifests itself as pain when pressing under the “pads” of the toes. It is symptomatic that the joints of the legs become inflamed as symmetrically (on the right and left limbs) as in the arms.
Large joints, such as the shoulders, knees, elbows and ankles, usually become inflamed later, after several weeks or months. Although there are other types of rheumatoid arthritis, in which the first to become inflamed are the shoulder or knee joints, or the heel tendons, and inflammation of the small joints of the hands and feet “joins” later. This form of arthritis most often occurs in people over 65-70 years of age.
In addition to intense pain, rheumatoid arthritis is characterized by the symptom of morning stiffness. Patients describe morning stiffness as a feeling of “stiffness in the body and joints” or as a feeling of “tight gloves on the hands,” less often as a feeling of “a tight corset on the body.”
With a relatively mild course of rheumatoid arthritis, morning stiffness usually disappears within an hour or two after the patient gets out of bed. But in severe cases of the disease, this unpleasant sensation can persist until one o’clock in the afternoon or even longer.
Many patients develop rheumatoid nodules under the skin. They are quite dense to the touch, usually about the size of a pea, and are most often located just below the bend of the elbows. But sometimes rheumatoid nodules also appear on the hands, feet and other places. More often there are few of them (1-2), but sometimes they are formed in large quantities. Usually the nodules are relatively small (2-3 cm in diameter), but quite large ones are also found.
Note from Dr. Evdokimenko.
If a rheumatoid nodule is cut open and viewed under a microscope, you will see that it is a collection of immune cells that surround a small patch of dead tissue. It is not yet clear what attracted them there, but they behave quietly and do not cause much concern to the patients. The nodes may decrease in size, disappear completely and then reappear. In other cases, they remain for many years without significant changes. The knots do not pose any threat and are more of a cosmetic defect.
Very often, the symptoms listed above are accompanied in patients by a feeling of weakness, deterioration of sleep and appetite, a moderate increase in temperature (up to 37.2-38 ° C), and chills. Patients often lose weight, sometimes significantly.
As the disease develops, in its advanced stage, permanent deformation of the fingers and hands occurs. More often than others, “ulnar deviation” of the hands develops, when the hands and fingers are fixed in the wrong position and deviate outward. The mobility of the wrist joints sharply decreases, the arms have difficulty bending and unbending at the wrists. Due to impaired blood supply, the skin on the hands and wrists becomes pale, dry, thinned, and the arm muscles atrophy. These phenomena intensify with increasing disease activity.
Gradually, more and more joints are involved in the pathological process. Knees, elbows, ankle and shoulder joints often become inflamed. Inflammation of the elbow, shoulder and ankle joints usually occurs relatively mildly, but leads to noticeable stiffness of the joint, sometimes to a rather sharp limitation of movements in the joint.
The situation is more complicated with the knee joints. Rheumatoid disease of the knees is often accompanied by the accumulation of a large amount of pathological fluid in the joint cavity, stretching the joint capsule. This accumulation of fluid in the knee is called a Baker's cyst. In the most severe cases, excess fluid in the cyst can lead to its rupture, and then the contents of the cyst spill into the soft tissue of the lower leg along its back surface. In this case, swelling of the lower leg appears, and sharp pain occurs in the leg. After some time, acute manifestations of the rupture usually subside, pain and swelling decrease. But if the inflammatory process in the knee continues, then the joint can “swell” again and again with all the ensuing consequences. And only when the activity of the inflammatory process is suppressed, the increased production of pathological fluid stops, and the rupture gradually heals.
In addition to inflammation of the joints, in the active phase of rheumatoid arthritis, the vertebral joints are sometimes involved in the inflammatory process. More often the cervical spine becomes inflamed, and then pain appears in the neck and under the back of the head. Sometimes they even try to treat such patients, suffering from inflammatory pain in the spine, with massage, manual therapy or heating - which is a gross medical error. All these attempts often lead only to an exacerbation of the disease and increased pain, since such manipulations during an active inflammatory process only intensify the inflammation.
Course of rheumatoid arthritis
The disease has a wave-like nature: periods of deterioration in the patient’s well-being are followed by periods of spontaneous improvements. Without proper treatment, patients suffer for many years, sometimes throughout their lives.
Proper treatment, coupled with restoration of mental balance, can lead to long-term remissions, significant improvement in well-being, and sometimes even complete recovery. However, few patients are able to radically and permanently change their attitude towards life, control their mental and physical state, and live in a state of “inner peace.” Therefore, either after the next unrest, or after a cold or hypothermia, the patient’s condition can again deteriorate significantly.
On top of this, over time, various complications in the functioning of internal organs are added to the damage to the joints. Rheumatoid damage to the lungs, heart, liver, kidneys, blood vessels and intestines often occurs. Sometimes rheumatic muscle inflammation develops - polymyalgia, which is a serious complication of arthritis. All of the above complications can not only seriously worsen the patient’s already imperfect condition, but can even pose a threat to his life. That is why it is important to begin treating rheumatoid arthritis as early as possible, and to treat the patient comprehensively and thoughtfully in order to interrupt the development of the disease at the initial stage, without leading to complications and without waiting for irreversible consequences.
This is useful to know.
In Finland, at the University of Turku, clinical studies were conducted under the guidance of Professor of Psychiatry R. Raymond. One hundred women suffering from rheumatoid arthritis were divided into 2 approximately equal groups. The first group included women whose development of arthritis was preceded by some serious problems, family troubles or troubles at work. Many of these women were experiencing anxiety, chronic sadness, or depression at the time of the study. The second group (which, by the way, turned out to be much more difficult to recruit) included women who had not experienced any special psychotraumatic situations on the eve of the disease. Most of these women from the second group fell ill after suffering from influenza or acute respiratory infections, or due to hypothermia.
Both groups of women were observed for several years, after which interesting circumstances emerged. It turned out that in the patients of the first, “problem” group, the disease progressed much faster, the symptoms grew rapidly, and the medications helped such patients much worse than the patients of the second group. Moreover, if some troubles continued to occur in the lives of these women, or if they were still in a chronically depressed state, many medications caused them intolerance or often “gave out” side effects. Moreover, in such cases, even changing medications often did not help - new drugs also often caused adverse reactions. Interestingly, women in the second, “problem-free” group had practically no such difficulties with medications. And in general, their arthritis progressed very slowly, it was much easier, with virtually no complications.
Article by Dr. Evdokimenko© for the book “Arthritis”, published in 2003. Edited in 2011 All rights reserved.
READ MORE:
- Causes of rheumatoid arthritis
- Diagnosis of rheumatoid arthritis
- Treatment of rheumatoid arthritis
- The first chapters from the book “The Secret Formula of Health”
- Chapters from other books by Dr. Evdokimenko