Full Russian-language electronic version of the International Classification of Diseases, 10th revision, with changes and additions WHO 1990-2019. (current in 2021)
A temporary code for COVID-19 has been added to section U00-U49
- U07.1
Codes U00-U49 should be used to temporarily assign new diseases of unknown etiology. In emergency situations, codes are not always available in electronic systems. Category U07 specifications allow them to be used in every electronic system at any time on behalf of WHO immediately.
Diagnostics
Arthrosis is often confused with the more dangerous arthritis, in which pain occurs primarily at rest. You should not engage in self-diagnosis; only a qualified doctor can determine the true cause of your ailment.
Arthrosis does not affect the general condition of the body in any way, affecting only the wrist area, and is not accompanied by fever and weakness.
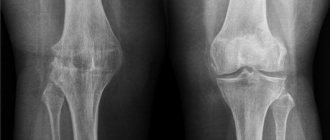
After examining and collecting anamnesis, the doctor will send the patient for an X-ray examination, which can be used to determine pathological changes in the joints. In order to be able to diagnose arthritis even in the initial stages, when the symptoms are not yet clearly expressed, additional laboratory tests of blood from a finger and vein are performed for a rheumatic test.
Treatment with folk remedies
For a speedy recovery, the treatment of arthrosis must be approached comprehensively, using several types of therapy. If it is not possible to attend auxiliary medical procedures, you still should not limit yourself to taking medications prescribed by your doctor. Self-massage will help you relax and improve blood circulation in the affected area. Massage your wrists with gentle movements every day for 10-15 minutes and you will soon see noticeable improvements. Also effective in the fight against exercise therapy disease. A regular set of exercises prescribed by your doctor will allow you to maximally develop the joint and keep it in good shape.
Compresses with medical bile, medicinal mud, birch or burdock leaves will help relieve pain.
This disease can be overcome not only by medication, but also by complete observance of rest. It is necessary to prevent any stress on the joint; to securely fix the wrist, it is recommended to wear a special orthopedic wristband or an elastic bandage. If the rules of caution are not followed, there is a risk of getting microtraumas, which will further aggravate the situation.
M18 Arthrosis of the first carpometacarpal joint
Osteoarthritis is a heterogeneous group of diseases of various etiologies with similar biological, morphological, clinical manifestations and outcome, which are based on damage to all components of the joint (cartilage, subchondral bone, synovial membrane, ligaments, capsules, periarticular muscles). It is characterized by cellular stress and degradation of the extracellular matrix of all joint tissues, occurring against the background of macro- and microdamage, while abnormal adaptive restorative responses are activated, including pro-inflammatory pathways of the immune system. Changes initially occur at the molecular level, followed by anatomical and physiological changes (including cartilage degradation, bone remodeling, osteophyte formation, inflammation).
Primary and secondary osteoarthritis - develops against the background of various diseases and joint injuries. Primary occurs, as a rule, after 45 years. The most common and characteristic locations are the knee joints, interphalangeal joints of the hands, spine, first toe and hip joints. Women more often than men suffer from arthrosis of the knee joints and joints of the hands.
Secondary arthrosis in its clinical manifestations does not differ from primary arthrosis, develops in almost any joint and has a specific cause of the disease.
Overweight occupies a special place among the risk factors for development. Thus, osteoarthritis of the knee and hip joints develops 4 times more often in obese women. It has been established that excess weight contributes not only to the onset of the disease, but also to its more rapid progression, leading to disability.
Schools for patients
Patients with osteoarthritis are recommended to attend Schools for patients, where they can receive comprehensive information about their disease, the advisability of losing weight (if they are overweight), learn physical therapy (physical therapy), proper nutrition and lifestyle. Specialists will explain the principles of therapy and answer your questions.
It must be remembered that weight loss measures must be combined with exercise therapy. Physical methods play an important role in the treatment of the disease, as they help improve joint function and increase endurance and muscle strength. Regular exercise therapy classes lead to a reduction in pain and improvement in joint movements, but it is best to start classes under the guidance of a specialist in physical therapy, for example, in health groups. Physical exercises should be carried out without static loads (sitting, lying down, in the pool). Patients with severe joint pain and contractures need to consult a physical therapy specialist to create an individual exercise program.
Recommendations for exercise therapy
The main principle of exercise therapy is frequent repetition of exercises throughout the day. You should not do exercises while overcoming pain. Perform the exercises slowly, smoothly, gradually increasing the load. You need to exercise for at least 30–40 minutes a day, 10–15 minutes several times during the day. For osteoarthritis of the knee joints, the main ones are exercises that help strengthen the thigh muscles (for example, raise a straightened leg by 25 cm while lying on your back and hold it for several seconds); exercises aimed at increasing range of motion (“air bike”); exercises that help improve the general aerobic condition of the muscles (walking on level ground at a moderate pace).
Walking should begin at a distance that does not cause pain, and gradually increase the duration of walking to 30-60 minutes (5-7 days a week). These aerobic exercises also promote weight loss. Patients should be aware of the peculiarities of the motor regime, the main principle of which is to unload the affected joint. Long walking and standing, and frequent climbing of stairs are not recommended.
With osteoarthritis, it is extremely important to reduce the load on the joints, which is achieved by using various devices. You should wear shoes with low, wide heels and soft elastic soles, which helps absorb the shock that spreads along the leg when walking and injures the cartilage. Shoes should be wide enough and soft on top. If the knee joints are affected, experts advise wearing knee pads, which fix the joints, reduce their instability, and slow down the progression of the disease. To reduce the load, it is recommended to walk with a cane, which should be held in the hand opposite the affected joint. In addition, it is very important to choose the right height of the cane - the handle should be at the level of the base of the first finger of the hand. In case of bilateral severe damage to the hip or knee joints, walking with the help of Canadian-type crutches. If you have flat feet, it is recommended to constantly wear special shoes (at home and on the street) with arch supports (insoles that support the arch of the foot and reduce the load on the joint), and in certain cases, custom-made insoles.
Treatment consists of a comprehensive approach to the disease, which involves the use of non-drug and medicinal methods, and, if necessary, surgical intervention. Although osteoarthritis is a chronic disease, treatment interventions tailored to each patient can reduce pain and inflammation, improve joint movement, and slow progression. It is important that the diagnosis be made by a doctor, since there are a number of other joint diseases that have similar symptoms to osteoarthritis.
As for drug therapy, it is stage-by-stage and individually selected by a specialist. Do not self-medicate and seek help. The more correct and timely the treatment is prescribed, the greater the chance of regaining the lost quality of life.
Active substances related to code M19.9
Below is a list of active substances related to ICD-10 code M19.9 (names of pharmacological groups and a list of trade names associated with this code).
- Active ingredients
- Aminophylline + Diphenhydramine + Indomethacin
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Amtolmetin guacil
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds - Bovhyaluronidase azoximer
Pharmacological group: Enzymes and antienzymes - Valdecoxib
Pharmacological group: NSAIDs - Coxibs - Hyaluronic acid
Pharmacological groups: Correctors of bone and cartilage tissue metabolism, Regenerants and reparants - Hydrocortisone
Pharmacological groups: Glucocorticosteroids, Ophthalmic drugs - Glucosamine + Chondroitin sulfate
Pharmacological group: Correctors of bone and cartilage metabolism in combination with other drugs - Dexamethasone
Pharmacological groups: Glucocorticosteroids, Ophthalmic drugs - Dexketoprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Diclofenac + Misoprostol
Pharmacological group: NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Diclofenac + Pyridoxine + Thiamine + Cyanocobalamin
Pharmacological groups: Vitamins and vitamin-like drugs in combination with other drugs, NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Dimethyl sulfoxide
Pharmacological group: Dermatotropic agents - Bile
Pharmacological group: Local irritants - Ibuprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Indomethacin
Pharmacological groups: Ophthalmic drugs, NSAIDs - Acetic acid derivatives and related compounds - Ketoprofen
Pharmacological group: NSAIDs - Propionic acid derivatives - Ketoprofen lysine salt
Pharmacological group: NSAIDs - Propionic acid derivatives - Cat's claw bark extract
Pharmacological group: General tonics and adaptogens - Lidocaine + Tolperisone
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs - Mabuprofen
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Meloxicam
Pharmacological group: NSAIDs - Oxicams - Meloxicam + Chondroitin sulfate
Pharmacological groups: Correctors of bone and cartilage tissue metabolism in combination with other drugs, NSAIDs - Oxycams in combination with other drugs - Methylprednisolone
Pharmacological group: Glucocorticosteroids - Naproxen
Pharmacological group: NSAIDs - Propionic acid derivatives - Naproxen + Esomeprazole
Pharmacological groups: Proton pump inhibitors in combination with other drugs, NSAIDs - Propionic acid derivatives in combination with other drugs - Nimesulide
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Niflumic acid
Pharmacological group: Other non-narcotic analgesics, including non-steroidal and other anti-inflammatory drugs - Capsicum fruit extract
Pharmacological group: Local irritants - Prednisolone
Pharmacological group: Glucocorticosteroids - Salicylamide
Pharmacological group: NSAIDs - Salicylic acid derivatives - Tenoxicam
Pharmacological group: NSAIDs - Oxicams - Tolperisone
Pharmacological group: Drugs affecting neuromuscular transmission - Tolperisone + Lidocaine
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs - Phenylbutazone
Pharmacological group: NSAIDs - Butylpyrazolidines - Celecoxib
Pharmacological group: NSAIDs - Coxibs - Etoricoxib
Pharmacological group: NSAIDs - Coxibs
6368
Post-traumatic arthrosis of the knee joint is a chronic progressive disease in which the patient experiences pain. It is difficult for him to move. The disease can lead to disability if it is detected at the last stage (or there is no adequate treatment).
Up to 20% of people suffer from it. The risk group includes elderly people and athletes.
Arthrosis of the wrist joints ICD 10
Note. In this block, the term “osteoarthritis” is used as a synonym for the term “arthrosis” or “osteoarthrosis”. The term "primary" is used in its usual clinical meaning.
Excludes: spinal osteoarthritis (M47.-)
Included: arthrosis of more than one joint
Excludes: bilateral involvement of the same joints (M16-M19)
[localization code see above (M00-M99)]
- arthrosis of the spine (M47.-)
- rigid big toe (M20.2)
- polyarthrosis (M15.-)
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
ICD-10 classification will help you understand your illness
Having gone to the clinic for joint pain, patients are left bewildered when they hear the diagnosis of “arthrosis ICD 10”. Many people take this frightening phrase to heart; it frightens a person, because the victim does not know what this incomprehensible term is, how to react to such a diagnosis, what complications it faces. Therefore, it is important to understand the current topic and finally find out what kind of pathology it is and what codes are assigned to it.
Brief description of the pathology. Statistical data
Osteoarthritis (osteoarthritis) is a common joint disease. The pathology may manifest itself as morning stiffness and limited mobility. She is characterized by moderate to severe pain. The development of symptoms occurs gradually. The disease is hidden for many years, manifesting itself only in moderate pain. According to ICD 10, arthrosis refers to diseases of the musculoskeletal system and connective tissue. In this class, this disease has a separate block. Arthrosis belongs to ICD code M15-M19. Spinal osteoarthritis is excluded from this block; it is in the spondyloarthropathy section under code M47. Also, acquired deformities of the fingers and toes due to arthrosis are excluded. Their current location is under code M20.2
The prevalence of the disease is increased among the 40–60 year old population of the world. More than 20% of people go to the clinic with joint and muscle pain. The disease occurs in half of cases at the age of 55 years. In elderly people, arthrosis ranks first among pathologies of the musculoskeletal system. By the age of 80, it is found in every patient. About 30% of people pay a disability pension with this pathology.
Preventive measures
The prognosis of the disease depends on its severity. Full restoration of functions is not possible. With a favorable prognosis, minimal thinning of the cartilage occurs. The main task with arthrosis is to preserve the joint in the condition in which it was at the time of examination of the patient. In severe cases of the disease, the prognosis is negative. In this case, endoprosthetics is considered the only method of restoring the patient’s ability to work.
Prevention of gonarthrosis consists of a healthy diet and weight control. If a patient leads an active life, he needs to perform exercises specially developed by a physical therapy doctor. Persons over 35 years of age are advised to take chondroprotectors. It is not recommended to relieve pain with folk remedies without consulting a doctor. Gonarthrosis is considered a lifelong pathology that must be constantly monitored.
Home > ICD-10
Forms of chronic inflammatory disease according to nosology
According to the International Classification of Diseases, 10th revision, in the “Nosology” section, more than one form of arthrosis is distinguished. Classification:
- Primary form. The etiology of deforming arthrosis of this form is unknown. It is characterized by destruction of the structure of cartilage and joint capsule. The disease is characterized by multiple joint damage.
- Secondary arthrosis progresses against the background of a decrease in the stability of cartilage tissue. The reasons for its development are most often known. Its formation is promoted by injuries, obesity, weakness of ligaments and muscles. Various factors and pathologies contribute to the emergence of the secondary form.
- Unspecified species. The essence of the pathology is the complete destruction of cartilage tissue. Affects the knee and hip joints.
Post-traumatic arthrosis is detected after damage to the joint (impact, bruise, fracture). It can also appear as a result of surgery. Post-traumatic arthrosis occupies the following codes according to ICD 10:
- coxarthrosis - M16.4, M16.5;
- gonarthrosis - M17.2, M17.3;
- first carpometacarpal joint - M18.2, M18.3;
- other arthrosis of the joints - M19.1.
Each form of arthrosis has its own signs and symptoms. Most patients complain of pain localized deep in the joint areas, which intensifies with physical activity.
Therapy for every degree
If the first degree is detected, therapy is rarely carried out. The pain bothers me periodically, but no attention is paid to it. More often, the pathology is discovered by the doctor by chance. The disease at the first stage occurs without radiological signs. During the examination, the doctor examines the skin in the problem area.
If the rheumatologist-orthopedic surgeon is qualified, the patient will be prescribed complex treatment. The first degree of the disease is eliminated with the help of medications, the action of which is aimed at stopping inflammation and eliminating pain. Taking medications in tablets is indicated. Unlike arthrosis, post-traumatic gonarthrosis with ICD 10 first degree is treated with injections that doctors inject into the damaged joint. Such injections have a local effect.
Additionally, the patient is recommended to undergo physiotherapeutic procedures. Diet therapy is not prescribed at this stage. To prevent the disease from going into remission, you need to eat a balanced diet and give up bad habits.
If the doctor has diagnosed post-traumatic arthrosis of the knee joint grade 2, urgent treatment is required. At this stage, joint disorders are externally noticeable. A crunching sound is heard when moving. The danger of stage 2 of the disease is that untimely therapy contributes to the complete destruction of the joint.
To stop this process, taking medications that restore blood flow and innervation is indicated. Therapy includes chondroprotectors. Exercise therapy, physiotherapy, spa treatment and other methods are considered the main measures that provide remission for post-traumatic arthrosis and gonarthrosis.
- Arthrosis of the ankle joint - symptoms and treatment
Stage 3 disease is accompanied by severe pain. To relieve it, the patient is prescribed appropriate medications. The regimen also includes medications that relieve inflammation. Therapy is long-term and intensive. In some cases, complex treatment is ineffective. Doctors come to this decision when deforming arthrosis is accompanied by complete destruction of cartilage.
The patient requires surgical treatment. The affected area of the joint is replaced with an endoprosthesis. The purpose of the operation is to restore the functions of the joint. The pain that accompanies the pathology disappears after surgery. Therapy for post-traumatic arthrosis, prescribed when the first signs appear, can slow down the pathology. In this case, 100% restoration of innervation is impossible.
Any degree of the disease requires long-term therapy. The first and second degrees are eliminated within 6-18 months.
Use of non-drug medications
Therapy for gonarthrosis can be surgical or non-surgical. The choice of treatment tactics depends on the stage of the disease. In the first two stages, drug treatment is prescribed. The operation is not performed. In grade 2, when conservative therapy is ineffective, surgical treatment is indicated.
Rheumatologists use non-drug therapeutic methods:
- diet;
- exercise therapy;
- cane;
- orthoses;
- massage.
Particular attention is paid to eliminating factors that increase the axial load on the diseased joint. Hardware physiotherapy includes electrophoresis with Dimexide, Novocaine, Analgin. Additionally, SMT, ultrasound, phonophoresis with Hydrocortisone, and laser are used. In the absence of contraindications, mud applications, hydrogen sulfide and radon baths are performed.
Drug groups
To combat gonarthrosis, rheumatologists use several groups of drugs. At the first stage, Paracetamol is prescribed. It quickly relieves pain. If the patient has gastrointestinal diseases, an NSAID + gastroprotector regimen is used. Additionally, Glucosamine sulfate is prescribed. Externally, the joint is treated with NSAID ointment.
At the second stage, when the symptoms are severe, taking NSAIDs is indicated. If the drugs are ineffective, glucocorticoids are injected into the joint. If there is effusion, treatment lasts 3 weeks. For this diagnosis, Betamethasone 1-2 ml or Methylprednisolone acetate 20-60 mg is prescribed. If NSAIDs are contraindicated for the patient, hyaluronic acid is injected.
If there is stage 3 joint damage, the patient is prescribed antidepressants and opioids. Surgical intervention consists of partial or total endoprosthetics, osteotomy, arthroscopy.
Surgical methods
Using arthroscopy, the doctor visually examines the composition from the inside. If necessary, affected cartilage fragments and inflammatory elements are removed. Resection of problem areas is carried out. Osteophytes are removed. The main purpose of arthroscopy is to make a diagnosis in order to plan subsequent actions.
Using an osteotomy, the axis of the lower limb is restored to relieve stress on the affected area.
A similar operation is performed for grade 1–2 gonarthrosis with varus or valgus deformity of the leg. Partial or total endoprosthetics are prescribed for patients over 50 years of age, with stage 2-3 arthrosis, damage to joint areas, and bone necrosis.
Resection arthroplasty is indicated for patients after endoprosthetics when there is a recurrence of the surgical infectious process. After the manipulation, it is recommended to walk with support, in an orthosis. If the joint is loose, and the doctor has confirmed the terminal stage of the disease, the symptoms are acute, endoprosthetics is impossible, arthrodesis is performed.
The operation will relieve the patient of pain while preserving the limb as a support. If you shorten your leg, after a certain period degenerative processes in the spine will begin to progress. In the absence of therapy or its ineffectiveness, complications such as subluxation, contracture, and complete immobilization of the joint may develop.