Have you noticed that it is difficult for you to turn your head? Does any movement of your neck cause discomfort and pain? Does your head literally not rest on your shoulders? Then it’s time for you to go to the doctor, since all these are symptoms of cervical osteochondrosis.
The neck area is most susceptible to various injuries. This part of the body is quite mobile, but its muscle corset is often weak. The load on small vertebrae is considerable, and the spinal canal is quite narrow. Excessive pressure leads to pinching.
Hundreds of thousands of people of different ages feel heaviness in the back of the head and unpleasant tingling in the upper extremities every day. Considering that these are trifles, they attribute the symptoms of cervical osteochondrosis to banal fatigue or a cold, not even suspecting how dangerous and insidious this disease can be.
There are many nerve endings and blood vessels in the neck. Also, it contains the vertebral artery, which is responsible for feeding the cerebellum and some parts of the brain. With osteochondrosis, it becomes pinched, which leads to impaired coordination of movements, decreased visual acuity, and in extreme cases, to a stroke.
The connection between the heart and the spine
It should be said right away that tachycardia itself is not a disease. It occurs against the background of other abnormalities or may be a normal physiological reaction to exposure to various stimuli. Normally, it appears after exercise, stress, strong coffee or, for example, an energy drink. But at the same time it arises and passes without a trace. Anxiety is caused by increased heart rate when it does not go away with rest or occurs with a certain frequency.
The mechanism of the effect of osteochondrosis on contraction frequency
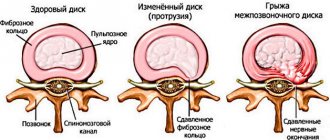
Displacement of the vertebrae and degeneration of the discs between them lead to compression of nerve endings and blood vessels - compression syndrome develops. The impulses travel along the vegetative fibers to the nodes, from which the signal is transmitted to the heart muscle and can provoke a rapid pulse.
Another mechanism for the problem to occur is poor circulation in the spine and nearby tissues. The more pronounced osteochondrosis is, the more they need blood flow. Under these conditions, the body compensates and increases pressure, forcing the heart to contract more often so that the organs do not lack blood and receive the necessary substances in full.
An additional effect on the nervous system is exerted by constant tension in the neck and muscles of the upper body. Along with chronic pain, sleep disturbances, irritability appear, and the influence of the sympathetic nervous system increases. Therefore, against the background of problems with the spine, blood pressure (hypertension) may increase and the heart rate may increase.
Can osteochondrosis cause tachycardia?
A person who is not familiar with the specifics of osteochondrosis does not know whether the disease can cause tachycardia, therefore, when turning to a doctor, he will most likely name signs of cardiac dysfunction, but forget to mention pain in the neck, back, and numbness of the limbs.
In any case, you should seek medical help, even if the main symptoms of cardiac dysfunction are absent, but the person feels neck pain and numbness in the limbs. A doctor who knows whether tachycardia can occur with osteochondrosis will begin treatment in a timely manner and prevent the development of complications.
Symptoms
The main symptoms of cardiac dysfunction are palpitations, which are accompanied by:
- sudden hot flashes;
- dizziness;
- attacks of suffocation;
- feeling of tightness in the chest area;
- increased fatigue;
- pain in the cervical spine.
There are a number of features that distinguish heart pathology from complications arising from vascular spasm during degenerative processes occurring in the spinal column.
Long-term heart pain:
- appear suddenly and disappear after a few weeks;
- from the beginning of the attack they gradually intensify, but after at least three days they weaken;
- are not fraught with a heart attack.
If the cause of tachycardia is osteochondrosis, the doctor will not notice changes in cardiac activity on the cardiogram.
In most cases, heart pain is preceded by physical exertion, sudden careless movements, such as turning or bending, and even coughing. If cervical osteochondrosis is complicated by pathology of the thoracic spine, the pain may become permanent.
Why does it occur
The connection between cardiac symptoms and osteochondrosis is based on two reasons.
- Heart pain occurs when damaged vertebrae compress nerve roots and spinal cord vessels. Painful sensations in the case of compression syndrome occur because impulses from compressed nerve endings spread to the sympathetic center for regulating heart rate.
- Damaged nerves do not send impulses to the receptors in the cervical spine. Because of this, the heart contracts more often and the pulse accelerates. The phenomenon is called reflex syndrome.
If the vertebral artery is pinched, the situation becomes dangerous because the main blood vessel supplies the spinal cord and part of the brain. If arterial blood flow is disrupted, the heart, respiratory organs, and brain centers that are responsible for hearing, vision, and coordination suffer.
Consequences
As mentioned above, osteochondrosis, which caused tachycardia, can lead to:
- partial hearing loss;
- blurred vision;
- loss of coordination, severe dizziness;
- nausea, even vomiting;
- headache.
In an advanced state, the disease provokes attacks of arrhythmia. To compensate for the lack of nutrients and oxygen, the brain sends a signal to the body and blood flow in the clamped vessels increases. A person develops high blood pressure, which becomes normal.
How to install a dependency
A careful study of the symptoms allows us to establish a connection between tachycardia and osteochondrosis.
If its cause is degenerative changes in the discs and pinched nerve fibers, the following is observed:
- rhythm disturbance occurs at rest;
- the condition worsens when changing body position, which increases the load on the spine;
- when the heart rate increases, sinus rhythm is maintained;
- improvement occurs after therapy for osteochondrosis.
In my practice, cardiac pathology is often found in combination with problems of the musculoskeletal system.
Therefore, there is a need for additional research:
- ECG (it will not detect ischemic changes);
- radiography (will show deviations in the structure of hard tissues);
- MRI or CT scan of the affected segment of the spine (will give a clear picture of changes at all levels).
Tachycardia is also a symptom of thyroid dysfunction during an allergic reaction. It can be provoked by anemia, fever and intoxication. In some cases, this symptom is observed when using drugs or certain medications.
Which departments should you look for the problem in?
Cervical osteochondrosis and tachycardia are most often associated. Due to the high mobility and weakness of the neck muscles, it is this part of the spine that is affected more quickly. The thoracic region is deformed less frequently, and changes in the pulse are rarely observed when the neurovascular bundle is pinched in the lower part. In the latter case, there is a reflex effect that is transmitted along the nerve fiber of the ridge.
During palpation examination in the affected area, muscle tension will be determined. A sharp turn or bend causes pain. Chondrosis of the cervical vertebrae is often accompanied by deterioration of vision and hearing, and periodic dizziness. With pathology of the thoracic region, pain often occurs when inhaling or exhaling deeply.
Features of tachycardia that occurs with osteochondrosis
Tachycardia that occurs with osteochondrosis is quite rarely accompanied by arrhythmia.
- Attacks occur not only during physical work, but also at those moments when a person is in a relaxed state.
- With timely treatment of osteochondrosis, the heart rate normalizes. The patient does not need to take drugs for tachycardia.
The heart rate can increase with a sharp change in body position and an increase in the load on the spinal column.
If a person has tachycardia due to osteochondrosis, pain cannot be eliminated with the help of hot compresses. In addition, the patient is not recommended to visit the sauna. Thermal effects on the affected area lead to exacerbation of osteochondrosis.
Patients should not self-treat the disease. If he tries to put the vertebrae in place with his own hands, his health may worsen. In some cases, self-medication leads to death. After all, the patient does not have special skills, and an attempt to independently adjust the vertebrae can end in failure.
With tachycardia due to osteochondrosis of the cervical spine, there are a number of distinctive possibilities.
Patients complain about:
- fast heart rate;
- vestibulopathy;
- throbbing headaches, especially in the morning;
- flashing of “flies” and multi-colored spots before the eyes;
- cognitive impairment.
Tachycardia in osteochondrosis of the thoracic region is accompanied by pain behind the sternum; the patient complains that a stake has been “driven” into his chest.
You can associate chest pain with spinal degeneration if you have:
- pain in other internal organs;
- feeling of lack of air;
- increased sweating;
- increased discomfort when inhaling;
- when the solid pulse accelerates.
Osteochondrosis is often accompanied by hypertension, fatigue, and decreased performance.
Having figured out whether tachycardia can occur with osteochondrosis, we will supplement the information with signs characteristic of compression of the VA and nerve roots.
Most often, patients complain of the following ailments:
- feeling of heat and stiffness in the chest area;
- sleep problems;
- disturbance of urination, up to leakage of urine;
- pain on palpation in the area of the spinous processes of the vertebrae;
- lack of air.
If a diseased spine can provoke rhythm disturbances and the described problems, then what should be treated first: tachycardia itself or osteochondrosis?
How to get rid
Treatment of tachycardia from osteochondrosis begins with eliminating the underlying cause. For this purpose, medications, traction, massage, and physiotherapy are used. Muscle relaxants and non-steroidal anti-inflammatory drugs help well; in case of severe pain, it is relieved with novocaine blockade.
When stable remission is achieved, the rhythm disturbance disappears. This result also serves as confirmation of a correctly made diagnosis. The prognosis is usually favorable. It is important to complete the full course of treatment and follow preventive measures.
For such a deviation, I usually recommend muscle relaxants with a sedative effect. They will not only eliminate muscle spasms in the affected area, but will also help normalize the functioning of the nervous system.
If the pulse exceeds 110 beats, and such attacks occur frequently, then the use of antiarrhythmic drugs is required. If treatment is not carried out in time, constant overload of the heart muscle will lead to failure. It is best to use beta blockers for this; they will not only reduce the heart rate, but also help prevent the development of ischemia. Hypotension is a contraindication to their use. At the same time, you can normalize the pulse with the help of drugs containing potassium and magnesium.
Features of treatment
If the heartbeat has increased due to osteochondrosis due to the fact that the vertebral artery was compressed by intervertebral discs, then it is necessary to improve the condition of the spine. This can be achieved using a set of therapeutic measures. Treatment is carried out to:
- swelling and inflammation in the area of the affected vessels have decreased. This will stabilize the blood flow through the veins and arteries;
- improve metabolic processes in the bone and cartilage tissues of the spine, restore the condition of damaged nerve cells.
If tachycardia is a concern as a complication of osteochondrosis, then it is treated using:
- drugs to reduce the frequency and strength of heart contractions;
- non-steroidal anti-inflammatory drugs;
- medications to relieve pain and dilate blood vessels;
- diuretics;
- chondroprotectors.
But these drugs can cause allergic rashes on the skin and inflammatory processes.
Massages are also recommended. In addition to them, point techniques are used.
They are needed for:
- working out deep-lying muscles and intervertebral discs;
- acceleration of metabolic processes in the superficial and deep layers of tissues.
Each patient, taking into account the individual characteristics of the body and the course of the disease, is prescribed physical therapy exercises.
They are used to:
- relieve static tension from the spine;
- strengthen the lumbar region, neck, shoulder girdle.
If the course of osteochondrosis worsens, then the need for physiotherapeutic techniques arises. When the manifestations of the disease decrease, ultrasound is performed. Under the influence of physiotherapeutic procedures, blood flow in damaged areas is accelerated, muscle functions are restored and the patient’s condition improves.
The operation will eliminate growths on the vertebrae, relieve blood vessels and nerve endings from high pressure, and normalize blood flow.
In order for therapeutic techniques to have the desired effect, it is necessary to get rid of the negative influence of provoking factors. Each patient is recommended:
- stop drinking alcoholic beverages and smoking;
- introduce vegetables and fruits into your daily diet that will saturate the body with vitamins;
- devote more time to rest, especially with frequent attacks of palpitations;
- take regular walks in the fresh air;
- Avoid the influence of emotional stress on the body.
The patient in such a situation should refuse:
- conflict situations and stress;
- visiting baths, saunas, using heating pads and compresses. If these methods are used, the course of the disease will worsen, exacerbations will occur, accompanied by swelling, inflammation in the area between the vertebrae, compression of the artery and nerve endings;
- trying to fix the problem yourself. You cannot take medications without your doctor’s permission;
- engage in self-reduction of displaced spinal discs into place.
Their reduction is the exclusive competence of a doctor in the field of manual therapy. Before this, it is necessary to determine exactly what caused the pain in the heart and increased myocardial contractions.
We advise you to study - Dorsalgia: what is it
If you strictly follow all the doctor’s instructions, this will not only stabilize the heart rate, but also relieve the manifestations of osteochondrosis, stop degenerative processes in the spine and reduce the likelihood of developing other, more serious pathological complications. Therefore, at the first manifestations, it is necessary to visit a doctor, undergo diagnosis and treatment.
Case from practice
A patient came to see me who was constantly tormented by attacks of tachycardia. The heart rate increased at rest, as well as after exercise, and reached 120–160 beats per minute. At the time of the attack, shortness of breath, weakness, and dizziness were observed.
No abnormalities were found on the ECG. X-ray revealed changes in the cervical spine. MRI showed the presence of a hernia between the IV and V vertebrae of the thoracic segment.
I prescribed non-steroidal anti-inflammatory drugs, muscle relaxants, and after achieving remission, I recommended massage of the cervical-collar area and exercise therapy. After 2 weeks there was a significant improvement, the pulse rate was 69–70 beats/min.
Why does it occur
In most cases, increased heart rate is physiological, that is, it occurs in response to stress or excessive physical activity. This condition is considered a normal reaction of the body and quickly passes when the provoking factor is eliminated. Also, the heartbeat increases when the air temperature rises, after drinking alcohol, coffee or strong tea, due to taking certain medications.
If tachycardia occurs for no apparent reason, it is a serious disease provoked by the following conditions:
- congenital anomaly of the cardiac conduction system;
- acquired diseases - atherosclerosis, coronary heart disease, arterial hypertension, endocrine pathologies (increased thyroid function, adrenal tumor).
But can osteochondrosis cause such a phenomenon as tachycardia? The answer is yes, there is a connection between these diseases. Most often, pathology in the cervical spine leads to an increased rhythm. With osteochondrosis, the vessels of the neck that supply the human brain can be compressed.
A smaller amount of blood passes through the narrowed vessels, therefore, in order to avoid oxygen starvation of the brain, the heart begins to work in an increased mode, throwing out as much blood as possible.
If you suffer from a severe form of lumbar osteochondrosis, there may be compression of the internal organs, which affects the adrenal glands. Dysfunction of these glands can also provoke tachycardia.
Expert recommendations
Paroxysmal or constant tachycardia with osteochondrosis requires not only the use of medications. They help in acute conditions, but do not in any way affect the duration of remission. The spine deforms slowly, but with each exacerbation the process gets worse. To prevent the condition from worsening and the attacks to recur, I would like to recommend the following:
- review your diet towards greater consumption of fruits, vegetables and other healthy foods;
- give up coffee, energy drinks, medications and other substances that increase heart rate;
- develop resistance to stress, this is helped by yoga, breathing practices, meditation;
- be sure to get enough sleep and follow a daily routine;
- Perform regular physical exercises to stretch the spine and strengthen the muscles of the back and neck.
If you want to know everything about tachycardia, we recommend watching the video below at the link. Causes, symptoms, diagnosis and signs that it’s time to see a doctor - talk about all this in 7 minutes. Enjoy watching!
Treatment
If tachycardia due to osteochondrosis is detected, it is urgently necessary to undertake comprehensive treatment of the spine. It is designed to reduce swelling with inflammation at the points of compression of blood vessels, as well as improve metabolism in the tissues of cartilage and bones of the spine, and restore the functions of injured neurons. Medicines prescribed:
- chondroprotectors;
- vasodilators;
- pain medications;
- diuretics;
- non-steroidal anti-inflammatory drugs;
- drugs to reduce the strength and frequency of heart contractions.
You can get rid of rapid heartbeat with osteochondrosis using ointments and creams based on the venom of bees and snakes. Such drugs:
- remove swelling;
- improve blood circulation;
- dilate the blood vessels.
Acupressure works the deep muscles and discs between the vertebrae. It also accelerates metabolic processes in all tissues.
Physiotherapy is eight sessions of Bernard currents during an exacerbation or a dozen ultrasound sessions during a relatively calm period. These procedures accelerate blood circulation in the affected tissues, restore the functioning of the paravertebral muscles, and improve the patient’s well-being. Other physical therapy methods may be used.
If conservative methods are not very effective, doctors prescribe surgery. During the operation, they get rid of growths on the vertebrae that compress blood vessels and nerve roots.
Treatment errors
You should not use antihypertensive drugs without conducting an examination. They will not help with osteochondrosis. However, by causing addiction, they will make life difficult in the future. No saunas, steam rooms or heating pads. Heat only increases swelling, increasing pinching of the roots and causing new attacks.
The most important nerves and blood vessels are located in the neck. Lack of qualified assistance can lead to serious complications. Be treated only under the guidance of an experienced doctor.
Features of manifestations in cervical or thoracic osteochondrosis
Pinching of a vessel due to a disease of the cervical or thoracic spine is a dangerous complication. This artery supplies the spinal cord, partly the brain, with oxygen and important nutrients. The lack of supply of these components leads to pathology of the heart muscle, functions of the respiratory system, hearing and visual apparatus, and impaired coordination of movement.
The main differences in the symptoms of tachycardia associated with osteochondrosis:
- Painful sensations are observed for several weeks.
- The pain syndrome has an increasing character, after a couple of days it becomes less pronounced.
- The manifestation of symptoms of osteochondrosis does not pose a threat to life and the organ itself - the heart.
- After several electrocardiographic examinations, abnormalities associated with tachycardia are not detected.
- The patient's condition is stable at the psycho-emotional level.
- The manifestation of symptoms increases with heavy loads on the spinal column.
- Painkillers cannot relieve pain.
Cervical osteochondrosis and tachycardia are common. Tingling in the heart area is felt during sharp turns, bending, coughing, and various physical activities. The duration of the attack does not exceed 20 minutes. In some, more serious cases, the duration of the attack is more than 2 days.
An increased heart rate in cervical osteochondrosis can be characterized by the following manifestations:
- increased body temperature;
- feeling of stiffness in the chest, loss of coordination, dizziness, possible fainting;
- sleep mode failure;
- fast fatiguability;
- pain in the neck.
The mechanism of development of osteochondrosis and tachycardia is identical to the formation of pathology in the cervical spine. The spinal artery is compressed, causing the heart to work more actively to supply the organs with the necessary amount of blood.
What are the differences?
It is now known whether the heart can hurt from osteochondrosis.
First of all, pay attention to the localization of unpleasant sensations. Most often this is discomfort behind the sternum or on the left side of the chest.
The pain can radiate to a person between the shoulder blades, in the left arm or in the lower jaw. Next, it is worth focusing on the characteristics of sensations. In the classic version, we are talking about pressing, squeezing, baking or dagger pain.
The next important factor is that heart problems most often have provoking factors in the form of a physical or emotional reset. This means that there is no pain at rest, but during exercise it appears again. Against the backdrop of a critical narrowing of the blood vessels that supply the heart muscle, the disease can appear even with minimal exertion at night and at rest.
When assessing the origin of chest pain, the time factor is always taken into account. True heart pain is not long-term; the count, as a rule, is in minutes
In other words, the heart will not be able to pull, ache and pound for several hours, days or day after day. Such discomfort is often a manifestation of pathologies in the skeletal and muscular system. True, true heart pain lasting more than twenty minutes indicates the development of a dangerous complication, namely myocardial infarction.
It is worth, among other things, to pay attention to the circumstances under which such discomfort in a person goes away. Angina usually goes away on its own within about a few minutes, for example, if the patient calms down or stops.
Some people are helped by Nitroglycerin, which reduces or completely stops heart pain within one or maximum two minutes. If the patient develops a myocardial infarction, then the chest pain will not be relieved even after using such tablets. In this case, emergency assistance will be required.
We advise you to study - S-shaped scoliosis
Against the background of heart disease, only a temporary disturbance of blood flow occurs in the coronary arteries affected by atherosclerotic plaques. Taking Nitroglycerin makes it possible to expand the lumens of blood vessels, improving blood flow and thereby pain goes away, which ultimately leads to regression of pathological discomfort. When a heart attack develops, the narrowing of the lumen is so pronounced that it leads to irreversible damage to the heart muscle. In this case, the pain has other causes, and taking such medications no longer has an effect.
In addition to the classic characteristics, heart problems can have a so-called atypical form, even manifesting in the form of shortness of breath or abdominal pain. Thus, in most cases, cardiac pathology can be recognized, although it is not always so easily recognizable
It is in this regard that it is very important that if a person has similar sensations in the chest, he feels a lack of air, then it is necessary to consult a doctor immediately. When the heart presses with osteochondrosis, you need to be examined.
Which doctor should I contact?
Most patients with complaints of palpitations turn to a cardiologist, and sometimes a therapist. These doctors prescribe all necessary diagnostic tests, including x-rays. Based on its results, a diagnosis is made and the patient is sent for further treatment to a vertebrologist or neurologist.
Osteochondrosis is treated by a vertebrologist.
Features of treatment
Osteochondrosis and arrhythmia are diseases that can become the basis for the occurrence of serious pathologies. Treatment is aimed primarily at combating the manifestations of osteochondrosis:
Normalization of nutrition (a specialized diet is prescribed, the consumption of minerals and vitamins is recommended). Various physiotherapeutic procedures are used: acupressure massage, manual therapy
For pain, it is very important that the massage be deep. Various creams and ointments based on snake and bee venoms have a very good effect. Products based on tea tree oil and containing pain-relieving ingredients have an incredibly positive effect.
Thanks to the warming effect, dilation of blood vessels is achieved, which reduces the level of compression, restores proper nutrition of various tissues, which reduces the level of pain. If the pain is very significant, then analgesics are necessarily used, which provide a quick process of pain relief, but such drugs are prescribed in extreme cases, since they negatively affect the functioning of the stomach and intestines.
Anti-inflammatory drugs (Ibuprofen) and vasodilator drugs (Dibazol, Papaverine) are also used in treatment.