Damage to the knee meniscus, according to official statistics, occupies one of the leading places among injuries to the joint of the same name.
Most often it is the result of a fall on straightened lower limbs or another sports injury, as well as a degenerative process that arose against the background of repeated damage to cartilage tissue, metabolic disorders, rheumatism, and chronic intoxication.
Damage to the meniscus of the knee joint is one of the most common injuries
Symptoms and treatment of injuries to the meniscus of the knee joint have their own characteristics, and therefore require careful diagnosis and a professional approach. Only competent treatment of the disease will allow a person to completely restore a sore knee without serious consequences for its normal functioning.
Causes of damage
As is known, the menisci are a paired organ consisting of cartilage cells and located in the cavity of the bone joint. They are designed to provide protection and additional cushioning during movements, as well as to reduce unnecessary movement and reduce the intensity of friction in it.
The main cause of damage to the meniscus is an unexpected, sharp blow to the cup with sliding, a fall of this area onto steps or other ribbed surface, which are accompanied by a sudden turn of the tibia outward, as well as inward.
The pathological condition is often diagnosed in representatives of sports professions, in particular football players.
Damage to the meniscus of the knee joint is very common in athletes
This type of injury often affects people who spend a lot of time standing.
Rupture or partial tear of the cartilage pad is sometimes the result of its degenerative degeneration, provoked by a number of factors, including:
- chronic intoxication;
- rheumatoid process;
- frequent microtrauma of the menisci;
- gouty lesion of the knee joint.
Degenerative damage to the meniscus is a long-term process. As it progresses, a person's articular surfaces slowly erode, and the functioning of the knee joint is disrupted. Such changes without adequate therapy lead to inevitable disability and complete loss of the ability to make full movements in the joint.
Classification of the disease
The choice of tactics for further treatment of the disease depends on the severity of the disorders.
Modern traumatologists decide on the advisability of using one or another type of therapy based on the classification of meniscus damage according to Stoller.
According to this classification, there are four main degrees of pathological changes in the cartilage tissue of the knee:
- 0 degree – absence of any changes, indicating the normal state of the menisci;
- 1st degree – the presence of a local focal signal with increased intensity without reaching the surface of the cartilaginous structure;
- 2nd degree – the presence of a linear horizontal signal of increased intensity with a partial violation of the integrity of the cartilage, which also does not reach its surface (damage to the meniscus of 2nd degree according to Stoller does not imply a violation of its general anatomical structure);
- Grade 3 – the presence of a linear signal with a high level of intensity reaching the surface of the cartilage (grade 3 meniscus damage according to Stoller is also characterized by complete separation of the cartilage pad or its partial displacement relative to its normal location).
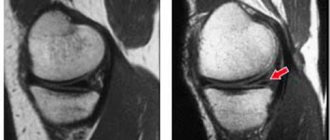
Degree of damage to the meniscus of the knee joint
Depending on the damage to the anatomical structures, in traumatology the following types of meniscus damage are distinguished:
- tearing at the point of attachment, namely in the area of the anterior or posterior horn, as well as the body located directly near the articular capsule;
- rupture of the internal part of the body, which is located away from the capsule of the knee joint;
- combination of pericapsular avulsion and internal rupture of the cartilaginous plate;
- chondropathy of the meniscus caused by its degeneration;
- cystic transformation of the cartilaginous tissue of the meniscus.
In medical practice, a distinction is also made between longitudinal and transverse injuries, complete and incomplete tears, flap-like and fragmented meniscus tears.
Features of the clinical picture
At the initial stages of the disease, the symptoms of damage to the meniscus of the knee joint are very similar to the signs of other ailments of the specified anatomical structure.
As the reactive inflammatory manifestations subside, other pathological signs begin to come to the fore, more accurately characterizing the nature of the disease:
- severe diffuse pain in the knee area;
- increase in size of the joint;
- increase in local temperature;
- disruption of muscle tissue trophism in the affected area;
- inability to play sports due to severe pain;
- difficulty getting up or down stairs;
- the appearance of a characteristic click when bending the knee joint.
You will learn more about how to determine meniscus damage from the video:
Signs of damage to the meniscus of the knee joint are rarely specific and can also be observed with bruises of the joint, arthrosis changes and sprains.
In this regard, the disease requires careful diagnosis, which will establish the true nature of the disorders and help determine their degree.
Diagnostic highlights
How to determine meniscal damage? Currently, there are many instrumental techniques that allow confirming such a diagnosis.
In the process of diagnosing the disease, doctors prescribe the following examinations to the patient:
- MRI, which allows you to accurately determine the localization of the pathological process, its severity and the presence of complications;
- X-ray examination of the knee joint in several projections, which is relatively informative;
- ultrasound diagnostics with tissue visualization, which allows you to determine signs of the inflammatory process and assess the amount of synovial fluid;
- arthroscopy, which makes it possible not only to diagnose disorders, but also to correct them.
Read more about hardware methods for diagnosing joint pathologies in this article...
Modern approach to treatment
How to treat meniscus damage? Pathology is one of the ailments that require an integrated approach to therapy. Before treating damage to the meniscus of the knee joint, the doctor prescribes a series of tests for the patient aimed at diagnosing the disease itself and the degree of its severity.
The doctor will conduct a thorough diagnosis and prescribe treatment
Read also: Bruised meniscus of the knee joint
Treatment of grade 1 injuries to the meniscus of the knee joint is carried out conservatively. In this case, only medications are used, including:
- chondroprotectors to stimulate the restoration of cartilage tissue and improve intra-articular metabolism;
- non-steroidal anti-inflammatory drugs;
- painkillers.
During the period of subsidence of general clinical symptoms, patients are recommended physiotherapeutic treatment using electrophoresis, UHF therapy, electric current, as well as sanatorium treatment, which significantly reduces the period of rehabilitation after illness.
Degenerative changes in the functionality of cartilage 2 degrees do not require surgical correction. Treatment of injuries to the meniscus of the knee joint without surgery is performed by prescribing intra-articular injections to the patient, as well as drugs from the group of chondroprotectors, NSAIDs, and medications that promote rapid regeneration of cartilage tissue.
If the development of disorders is traumatic, arthroscopic surgery is indicated for sick people, after which a course of antibiotics and restorative drugs is recommended.
After stage 3 of the disease is established, the patient must undergo surgery to remove part of the meniscus and replace it with prosthetics. More often, such therapeutic measures are used in relation to damage to the internal meniscus of the knee joint.
Knee meniscal endoprosthesis
Other indications for surgical treatment of medial meniscus injuries of the knee joint are:
- meniscus displacement or rupture;
- complete separation of the body of the cartilaginous structure along with the horns;
- hemorrhage into the joint cavity.
Thanks to modern equipment, doctors are able to save even a completely torn meniscus.
Naturally, this is facilitated by young age and the absence of gross metabolic disorders.
It is important to remember that complete restoration of the function of damaged cartilage depends on a number of factors, including timely seeking medical help, competent and comprehensive diagnosis, as well as adequate treatment, maximally aimed at preserving the anatomical integrity of the joint.
Meniscus tear
A meniscal tear is the number one most common injury among all knee joint injuries. Doctors at Mirt MC have accumulated vast experience in its treatment and are ready to help their patients.
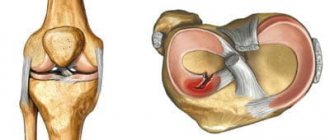
The menisci are the shock-absorbing system of the knee joint, which also performs a stabilizing function. There are two of them in the knees, they are located on the sides of the joint, connected by a ligament in front, and their shape resembles crescents. One of them is turned more anteriorly, and the second - posteriorly. In medicine, they are usually called the lateral (anterior) and medial (posterior) menisci, respectively.
The shape of the menisci determines their structure; each can be visually divided into three parts:
- Body (middle)
- Front horn
- Posterior horn
The vascular network in them is distributed unevenly: there is a red zone, rich in capillaries, which is located at the edge, and a white zone, completely devoid of blood supply. It is located in the center.
The healing speed of an injured meniscus depends on the location of the injury: the “red” zone of cartilage is restored faster and better.
A rupture of the meniscus of the knee joint is a consequence of direct, indirect and indirect injuries to the knee or long-term degenerative changes in tissues against the background of gout, rheumatism, accelerated wear of joints in people who work most of the time while standing.
There are also combined injuries, in which other parts of the joint are damaged along with the cartilage - ligaments, capsule, fatty body. A rupture of the meniscus joint (the name is fundamentally incorrect, but is used in everyday life by people ignorant of medicine) is a serious injury, the treatment of which takes a very long time.
To determine the nature of the damage, the situations in which they were received are important.
Thus, direct injuries occur when falling due to a sharp impact with the knee on the edge of a curb or step, or due to a collision with a fast-moving object.
Indirect and indirect damage to the menisci is a common problem for athletes and dancers - people who, in order to perform certain elements of exercises or dances, rotate on one leg for a long time, run a lot, jump, and walk in single file. Those who like to squat are also at risk for meniscal tears.
Elderly people with existing age-related or degenerative changes in cartilage tissue turn to a traumatologist with combined injuries. They experience a rupture of the horn of the medial meniscus (posterior).
Medial meniscus tear and other injuries: types of knee cartilage injuries
The lateral (anterior) cartilage suffers from injuries relatively rarely. A tear of the posterior meniscus is the leader among all injuries of the knee cartilage: complete, incomplete, transverse and longitudinal, crushed tear, as well as a flap-shaped tear are observed.
In this case, the anterior horn is least susceptible to injury, and most often the body itself suffers with the transition to one of the horns. Isolated rupture of the posterior horn of the medial meniscus occurs in approximately one third of cases.
Traumatologists also classify cartilage damage by location and severity:
- A full avulsion rupture is the most severe degree of injury. In such cases, the cartilage is separated from the paracapsular zone by all its parts
- Ruptures of both horns and the body of the meniscus in the transchondral region
- Rupture of the ligament between the menisci, degeneration of cartilage tissue, leading to abnormal mobility
- Valgus knee is a consequence of chronic injuries of the menisci and their age-related or post-traumatic degeneration
- Cystic formations in cartilage (most often the lateral meniscus is affected by cysts)
When injured, the torn part of the cartilage may move or remain static. A rupture of the posterior - medial - meniscus in many cases is aggravated by damage to other parts of the joint - capsule, fat body and ligaments, especially in older people who already have problems with the bone apparatus.
How are meniscal tears diagnosed?
In the acute period, a rupture of the horn of the meniscus or its body is very difficult to diagnose if it is not possible to use arthroscopy - the most reliable way to distinguish a cartilage injury from other injuries of the knee. The reason is the great similarity of their symptoms:
- Severe pain
- Edema
- Hematomas
- Limited or complete immobility of the knee
However, there are also characteristic signs of meniscal injury - pain in the joint space, hemorrhage in the joint. They are determined by special tests (McMurry and Apple tests) and radiographic methods.
The full picture of the injury appears only two to three weeks after the injury, in the so-called subacute period, when the symptoms of cartilage rupture “specify”:
- Pain remains along the joint space
- An infiltrate appears in the capsule
- The joint is blocked (does not bend or extend)
A number of voiced tests are also carried out - special movements during which the characteristic sounds of the meniscus sliding, their movement, and also clicks are clearly audible.
A tear of the medial cartilage is reliably determined by the true blockade of the joint, when it is fixed at a very large angle - approximately 150 degrees. However, even here specialists need to be on guard: even such an eloquent symptom can only be a sign of muscle contracture - a consequence of bruises, injuries to the capsule and ligaments. Sometimes it occurs against the background of chondromalacia, chondromatosis, Koenig's and Hoffa's diseases, or a completely harmless and easily removable infringement of the pterygoid ligament.
Diagnosis of meniscal injuries at the Mirt MC has not been particularly difficult for a long time thanks to the diagnostic equipment available at the center - a modern video arthroscope, which helps to completely determine the type of injury, its severity and immediately carry out treatment - fast and effective.
Knee meniscal tear: treatment of injury
Medical tactics are chosen depending on the nature of the meniscus tear: treatment can be prescribed either conservative or surgical.
Conservative methods are more often used for acute uncomplicated injury:
Splinting the injured knee to completely immobilize it for two weeks
- Joint puncture
- Removing the blockade of the joint
- Prescription of desensitizing drugs
- Physiotherapeutic methods for eliminating swelling
- Isometric exercise therapy of the thigh muscles
Treatment of a meniscus tear without surgery is justified for ruptures of the posterior horn, when the injury is not very complex and it is possible to eliminate the blockade of the joint. The depth of the tear also matters: if the medial disc is torn longitudinally by no more than 10 mm, and the transverse tears below or above do not exceed three millimeters, then such injuries often heal on their own.
With timely and correctly prescribed conservative therapy, paracapsular tears heal with a durable scar due to good blood circulation in the pericapsular area.
Rupture of the meniscus of the knee joint: surgery at the Mirt MC
Surgery is inevitable when the doctor diagnoses a complete or deep meniscus tear: surgery in such cases is the only way to save the knee joint. Patients with chronic cartilage injury cannot do without it.
Before the advent of arthroscopy, surgery always meant complete removal of the damaged cartilage on the open joint, which in the future entailed a long recovery period and premature wear.
Now surgeons use a gentle technique for suturing damaged parts, which allows preserving the meniscus. They also perform arthroscopic meniscectomy if the cartilage is completely torn off, crushed, or many cysts appear on it.
No preparation for surgery using arthroscopy is required: just an examination is enough.
Surgery on the meniscus is performed under one of the types of anesthesia chosen by the anesthesiologist - local or conduction. Next, the thigh is tightened with a tourniquet and two incisions are made on the skin of the injured knee: one for an arthroscope with a video camera, and the second for the introduction of special surgical instruments.
During the intervention, the doctor assesses the condition of the bent knee joint, observing the resulting image on the monitor, removes debris, and sews together what can be sewn.
During meniscectomy, the cartilage is completely removed, and the joint cavity is sanitized - small foreign bodies are removed from it, then treated with an antiseptic.
After the operation, a pressure bandage and cold are applied to the affected leg. The patient can get up and walk with support the very next day and is observed in the department for another two to three days, after which he is discharged.
Then for several more weeks he walks with support and is treated on an outpatient basis right there, at the Mirt MC, where our specialists continue to monitor him.
In the future, patients are recommended to undergo rehabilitation physiotherapeutic courses and exercise therapy classes in the clinic’s gym.
Damage and tear of the meniscus - what's the difference?
It is very important to distinguish between a knee meniscus injury and a tear, as this determines different prognosis and treatment options.
A damaged meniscus is still able to absorb stress if the outer part remains intact. In addition, the injury may avoid surgery when the injury is stable and located in the most vascularized part of the knee joint structure. A strong quadriceps muscle is able to compensate for deficiencies in the meniscus and other ligaments that stabilize the knee.
If the meniscus is torn , which is often the result of a past injury, surgery is necessary because it can no longer perform its function.
What is meniscus
The meniscus is a crescent-shaped fibrous cartilage located in the knee joint.
The functions of the meniscus are:
- increasing the depth of the glenoid to improve the fit between the bone tips;
- absorption of shock load;
- cushioning the load on the knee joint.
In cross-section, the meniscus has the appearance of a wedge, since it is thicker on the outside, while the internal structures are thinner.
The two menisci are connected at the front by the transverse knee ligament (which allows them to move in concert during various movements of the joint). The ends, which are called “horns,” of the meniscus are fixed in the anterior and posterior zones of the tibia (tibia).
The two menisci of the knee joint differ in both location and names - “lateral meniscus” and “medial meniscus”.
- Lateral meniscus. Located on the outside of the joint. It is smaller and more mobile than the medial one, and is weakly attached to the fibers of the articular capsule. Its ends are very close to each other, causing it to take the shape of the letter "O".
- Medial meniscus. This meniscus is stably anchored in the joint capsule and on the medial collateral ligament. It is less mobile than the lateral one and is shaped like the letter “C”.
Causes of meniscal injuries
Mechanisms of meniscus tear are divided into two types: degenerative and traumatic.
The first case especially affects middle-aged people and is often caused by stress that is harmless to a healthy meniscus. The meniscus tissue weakens due to the lack of nutrients from the synovial fluid, which leads to abrasion and injury.
As for traumatic injury, it typically occurs as a result of a forceful rotation of the femur on the tibia (tibia), with the leg planted on the ground and the knee slightly bent.
Which athletes are at risk?
We are used to thinking that football players most often encounter meniscus injuries, but this is not entirely true. Look at the following table to see what other sports are considered high risk.
The most common cause of injury is degenerative processes and therefore wear and tear of the joint (especially in middle-aged people).
Runners with valgus and varus knees and laxity of the anterior cruciate ligament are prone to meniscal injuries.
Strong quadriceps muscles can reduce your risk!
A ride on the bicycle
Incorrect bike settings, poor physical fitness, and low flexibility increase the risk of meniscus tear.
It is important to optimally adjust the saddle to increase the knee-pedal axis and optimize the placement of the foot on the pedal, as well as wear suitable shoes.
Skiing
Inappropriate equipment and insufficient training increase the risk of meniscal injuries by 50%.
How are meniscal injuries classified?
There are several classifications of meniscus injuries and tears.
According to this classification, three main types of meniscal injuries can be distinguished:
- Longitudinal injuries. Most often they affect the posterior horn of the medial meniscus in the peripheral part. May have a vertical or oblique direction relative to the articular surface, and may affect the femur, tibia, or both bones. Typically associated with damage to the anterior cruciate ligament.
- Radial injuries. They pass along the inner edge of the meniscus and cross it (fully or partially). They are most common for the lateral menisci.
- Horizontal injuries. They form in the deepest part of the meniscus, dividing the meniscus into two “layers”: upper and lower.
Read also: Signs of a torn meniscus of the knee joint
Classification depending on the type of damage:
- Damage to the bucket handle. Represents a worsening of a longitudinal injury with tearing of the edges of the meniscus.
- Parrot beak injury. Develops from untreated radial damage.
- "Flap" type lesions. Represents an aggravation of a horizontal injury and can lead to displacement of part of the meniscus.
Classification based on magnetic resonance imaging:
- I degree. Indicates the presence of small areas of degeneration in the very central part of the fibrocartilage.
- II degree. Represents the development or expansion of stage I phenomena without involving the knee joint.
- III degree. These are significant injuries involving at least one side of the knee joint.
Is surgery necessary for grade 2 meniscus damage? Arthroscopic procedure
Many people are hesitant to undergo surgery because they do not know that manipulation of the meniscus of the knee joint is not so scary. Partial or complete resection is done in the most gentle way: without pain, cuts and blood, using a safe and effective regional anesthetic. Patients are concerned about whether they can run after removal of the meniscus of the knee joint (
In the operating room.
Let's just say that people are allowed to lead their usual lifestyle, where running, jumping, cycling, and so on are not contraindicated, but only after a thorough restoration of the operated area. There are many real examples where even football players return to the game after such an intervention, and actively take part in competitions, playing at a professional sports level.
Exercise not on an unstable platform.
It is very important for the patient’s life to undergo rehabilitation so that after surgery the meniscus of the knee joint does not change for the worse. It will be as dynamic and rich as before. Well, we already discussed the dangers of inaction at the very beginning of the article. Now, actually, let's talk about the surgical procedure itself.
Modern medical technologies allow injured cartilaginous structures to be restored minimally invasively. Thanks to this, recovery after surgery, usually a suture is placed on the meniscus, is quick and without any difficulties. For therapeutic and restorative purposes, the arthroscopy method is used. The procedure is performed using a fiber-optic endoscopic device equipped with a video device called an arthroscope.
- The optical device looks like a thin probe. The probe is inserted through a puncture in the skin (diameter 5 mm) inside the joint and brought directly to the damaged object, which is visualized on the operating screen in enlarged sizes. The minimally invasive technique can also be used as a diagnostic tool if traditional diagnostic methods turn out to be insufficiently informative.
- Having decided on the treatment tactics, which will depend on the type and severity of the damage, the surgeon, using an additional puncture and special instruments, begins to perform the main tasks of eliminating defects on the meniscal body. The doctor, as far as possible, will try to preserve the cartilage tissue as much as possible, sparingly removing only clearly non-viable areas.
- There are two most common correction techniques: suturing the linear tear or excision of the marginal dislocated areas. In the first case, a suture will be applied using medical threads using a special technology. In the second, microsurgical instruments will be used to resect the flaps in the peripheral part, and then polish the edges of the meniscus. If free fragments are detected, the specialist removes them from the joint space.
- At the end of the session, the surgical field is washed. Small skin incisions are sutured, treated with antiseptic agents and covered with a sterile dressing. No plaster needed.
Symptoms of meniscus cracks and tears
The appearance of intense pain in the knee joint is the first alarm bell: if the medial meniscus is damaged, the pain will be localized on the inside of the knee; if it is lateral, the pain will be present on the outside.
Subsequently, the pain is accompanied by swelling of the joint , signs of effusion in the joint and the inflammatory process.
If fragments break off from the meniscus and remain in the space of the knee joint, then, affecting flexion-extension, they can cause blocking of the joint or its weakening. In this case, extensive damage to the structure of both the meniscus and the joint also occurs.
When bending the knee joint, there is often some crunching sound .
With degenerative type injuries, the symptoms will be less pronounced, knee pain appears only with exertion and joint swelling rarely occurs.
Definition and functions of the meniscus
The meniscus is a cartilage pad measuring about 6 cm and about 3-4 mm thick that is present in the knee, shoulder, ankle and some other joints. This spacer is located inside the joint (between the articular surfaces) and has a C-shape. Each knee has 2 menisci - one on the inside (medial menisci, firmly secured by ligaments) and on the outside (lateral menisci, more mobile). They perform the following functions:
- depreciation - absorbing shock loads on the joint when running, walking, jumping;
- protection of subchondral bones - the meniscus protects the bones that form the knee joint from the loads associated with upright posture (distributes them evenly over the entire surface of the joint, preventing rapid wear of the protruding parts);
- ensuring congruence (coincidence and optimal interaction) of the articular surfaces - plays the role of a seal in the joint.
How are meniscus injuries diagnosed?
Diagnosis is primarily based on clinical manifestations during orthopedic maneuvers. The presence of pain on the inside of the knee with hyperflexion, hyperextension and external rotation of the bent knee at 90° is a sign of damage to the medial meniscus. While the appearance of pain during hyperflexion or internal rotation of the leg bent at 70° and 90° is a sign of a lateral meniscus tear.
As for instrumental diagnostics, it is carried out using magnetic resonance imaging. This often helps identify degenerative changes.
Diagnosis of meniscus tear
As mentioned above, diagnosing meniscus injuries is complicated by injuries to nearby soft tissues. Therefore, even contacting a traumatologist does not guarantee an accurate diagnosis without additional hardware tests. Palpation and motor tests can be made more difficult by swelling or pain in the knee or long-term use of painkillers.
Functional tests for diagnosing a meniscus tear include: Chaklin's test, Shteiman's symptom, Baikov's method, Polyakov's symptom, Landau's test, McMurray's method, Perelman's symptom.
The most common diagnostic methods include:
- computed tomography or magnetic resonance imaging (also helps to determine the condition of ligaments, tendons, cartilage, muscles, and to determine the presence of microfractures that are invisible on an x-ray);
- arthroscopy.
These techniques are necessary to accurately determine the location of the rupture and the extent of damage. X-ray and ultrasonography are not informative methods of research, since they do not provide a complete picture and can give false results.
Diagnostic studies help determine the presence of microtrauma that is undetectable by simple examination. Although microtrauma to the meniscus is not a tear, it can have unpredictable consequences for the knee joint as a whole and therefore also requires treatment.
Treatment in case of injury or meniscus tear
As with any type of lesion, treatment depends on several factors, in particular the age and activity level of the patient, as well as the location and nature of the lesion.
In what cases is surgery used and in what cases is it not required?
First, surgery is not always an effective solution. There are cases when the patient's knee retains full mobility and functionality, and the blockage resolves spontaneously. The joint can also be unblocked using manipulative techniques.
Surgery may be necessary in cases of severe injury or when conservative treatment fails.
There is a method for surgical correction of the meniscus:
- Partial meniscectomy: used in cases of complex injuries with the formation of free fragments, and in cases of rupture of the central part of the meniscus.
- Meniscus repair: used in cases of rupture of the outer meniscus, but recently it is increasingly used in cases of rupture of internal fragments in young or not very young patients, but physically active.
- Total meniscectomy: Currently used only in cases of extensive lesions of the entire meniscus or when the meniscus cannot be repaired.
In young or physically active patients who require removal of the meniscus, meniscus transplantation is offered.
Treatment of damaged MRMM
Basically, temporary disability occurs during the treatment period. The sick leave period can last from several weeks to four months. Basically, if the MRMM ruptures, it cannot be done without surgical intervention; treatment is carried out by removing the entire cartilage or its broken part. This operation is called meniscectomy. Only a few small incisions are made on the knee; open manipulation is performed in extremely rare cases.
In case of minor damage to the MRMM, the treatment cycle will look approximately as follows:
- Long rest using elastic bandages and various compresses.
- Surgery that corrects the functions of tissues and organs.
- Physiotherapy.
The rehabilitation period is reduced to the relief of pain symptoms with an emphasis on reducing swelling and normalizing the motor activity of the injured organ. For a complete recovery, you need to be patient, since the rehabilitation period can last quite a long time.
Rehabilitation for meniscus injuries
This is a very important stage in the treatment of meniscus injuries (if the outer meniscus is damaged, then rehabilitation will be faster) and restoring the functionality of the knee.
In the following table you will find a description of the different stages of rehabilitation and physical therapy after meniscus injuries.
(first 4 weeks)
Characterized by persistent pain and effusion in the knee joint.
The joint is protected with braces that are worn day and night.
- reduction of pain and effusion;
- restoration of the range of joint mobility;
- preventing the development of restrictions in the patella;
- muscle control;
- restoration of postural stability;
- Improved hip and ankle strength and flexibility.
How to do it:
- application of cold and compression against pain and effusion (medication with Voltaren is also often used);
- when walking with the help of crutches, they create a partial load on the knee;
- exercises of continuous passive movement from a sitting position;
- exercises to develop the quadriceps muscle;
- development of the ability to balance in a vertical position;
- stretching the hamstrings and leg flexors.
(from 4 to 10 weeks)
Effusion and pain are minimal. The knee can be fully extended and extended to 120°.
- restoration of normal mobility of the knee joint;
- improving flexibility, strength and endurance of the entire lower limb.
How to do it:
- control of knee mobility (especially extensor muscles) by using a bandage;
- regaining mobility through stretching exercises;
- strengthening muscles using exercise bikes, soft resistance machines;
- regaining the ability to maintain balance (for example, going up and down stairs);
- increasing the range of mobility of the leg and rectus femoris.
(between 9 and 12 weeks)
There is no pain or effusion, the range of motion of the joint is fully restored, and muscle strength reaches 60-80% of what it was before the injury.
- preparation for return to full functional activity;
- teaching the patient behavior that preserves the meniscus.
Read also: Meniscus fracture
How to do it:
- exercises that simulate functional activity;
- increasing the duration and intensity of exercises that increase muscle strength;
- after 5-6 months you can completely return to the standard training program (in the case of athletes).
Always remember that the rehabilitation process is very long and requires complete dedication from the patient , especially in the early stages when you have to endure pain.
Causes of degeneration
The anatomical features of the location and structure of the menisci determine the high incidence of pathologies both among young people and among mature people. Most often, athletes, ballerinas, dancers suffer from ruptures, damage and cystosis - that is, people who are in constant motion and experience high loads.
Other possible reasons:
- dysplasia – abnormal formation of the knee joint;
- gout, syphilis, tuberculosis, rheumatism and other diseases that can affect joints;
- sprains of ligaments, as well as their incorrect formation;
- flat feet (low shock absorption of the foot is compensated by increased load on the knee);
- high physical activity;
- excess weight.
Stages of meniscus damage
Damage to the cartilage structures in the knee joint occurs due to injury and as a result of thinning caused by natural aging. The degree of damage to the meniscus is a kind of indicator of the severity of the degenerative process. Physiological criteria corresponding to the destruction of knee cartilage in a certain phase of the disease help to make an accurate diagnosis and select the correct therapy for each individual case.
Treatment methods
Therapy for degenerative changes in the menisci completely depends on the nature of the damage. Acute injuries serve as a direct indication for the use of conservative treatment methods:
- First of all, a puncture of the joint is performed, eliminating its swelling and restoring mobility. Sometimes several procedures are required, since active exudation (secretion of inflammatory fluid) in the joint lasts up to three to four days.
- Analgesics are prescribed, preference is given to narcotic drugs (Promedol and its derivatives), because other drugs in this case, as a rule, are not able to relieve the patient of pain.
- Chondroprotectors provide the body with the necessary substances to restore the damaged area of the meniscus.
- Anti-inflammatory drugs.
- At the rehabilitation stage, physiotherapeutic methods are used as an auxiliary means - ozokerite, UHF, iontophoresis, shock wave therapy.
- For 14 days, a splint is applied to the straightened leg to secure the joint in the required position.
In case of ruptures, surgical intervention is indicated: instruments are inserted into the knee joint through two miniature incisions and the damaged area is sutured. Serious injury may require the cartilage lining of the joint to be removed and replaced with an artificial one. All surgical procedures are performed only after signs of inflammation have subsided.
Chronic dystrophies, joint dysplasia and abnormal development of the ligamentous apparatus require exclusively surgical treatment.
If the cause of degeneration is chronic diseases, such as rheumatism and gout, along with surgical methods, the underlying disease is also treated (diet, immunocorrectors and other methods).
Degenerative transformations of the menisci are a fairly common pathology that requires immediate consultation with a specialist. The future functioning of the joint depends on the timeliness of treatment, and delays can cause the spread of degenerative processes to other elements of the joint. Therefore, do not delay your visit to the doctor, take care of yourself and be healthy!
Causes of damage
Meniscal tears occur in people of all ages. In young patients, cartilage damage has the features of a primary disease, while in more mature people it is secondary in nature - it accompanies the natural aging processes occurring in the joints. Rupture of cartilaginous structures accompanied by pain occurs for the following reasons:
- Injury. Cracks and tears occur when the knee moves suddenly inward or outward, during deep squats, impacts, falls, or heavy lifting. The lateral meniscus of the knee joint (outer) can shift under mechanical stress, so it is less likely to be injured. According to statistics, the medial (internal) one suffers much more often, since it is firmly secured by ligaments.
- Age-related degenerative changes. As you age, the joint gradually wears out and loses its elasticity.
- Excess weight. Weight gain increases stress on the knee joint, wears down the cartilage, and increases the risk of tearing.
- Chronic inflammation.
- Gout, rheumatism.
Prevention of knee meniscus tear
To ensure you never wonder how to treat a knee meniscus tear, you should take the following precautions:
- Be sure to warm up before any physical activity.
- Avoid deep squats, sudden and twisting movements.
- Monitor your weight and consume a balanced menu high in vitamins and minerals.
- Do not neglect moderate sports loads to maintain the muscular-ligamentous apparatus and stabilize the knee joint.
- After 40 years, start taking prophylactic chondroprotectors, even if there are no symptoms of a meniscus tear.
Source
Degrees and symptoms according to Stoller
To make it easier for doctors to navigate when assessing the condition of cartilage tissue, American orthopedist David Stoller identified several degrees of severity.
David Stoller divided cartilage pathologies into three groups.
The stage of meniscus destruction is determined using MRI diagnostics, which is based on changes in signal intensity when abnormalities are detected in the meniscal tissue in one or more areas. The more intense the signal, the more contrast the damaged area is highlighted on the screen with a three-dimensional image of the joint. Most often, problems are recorded in the medial (internal) cartilage, where more than 2/3 of all damage occurs in the posterior horn. According to Stoller, the condition of the menisci is divided into 3 degrees.
initial stage
Stoller grade 1 medial meniscus injury causes uneven focal signals on scanning. The pathology is localized in the inner part of the cartilage and does not affect the outer shell. In the initial stage, the damage is minor; problems with the meniscus are indicated by variable pain, especially noticeable after a long walk and when climbing stairs. A crunching sound is heard in the knee when bending.
2 degree of change
Stoller grade 2 damage to the internal meniscus is characterized by high-intensity linear or focal signals localized from the center to the edges of the cartilage, not extending beyond its surface. This means that incomplete tissue destruction has occurred without fragmentation. Grade 2 meniscus damage is manifested by pain in the joint with every movement of the leg and is accompanied by crunching and clicking sounds. Swelling and redness of the skin may occur.
3rd degree tears
In the last stage, the anatomical integrity of the meniscus is completely destroyed. With this pathology, hyperintense signals appear in several areas, reaching the edges of the cartilage shell and emerging to the surface. The person suffers from severe pain and cannot bend or straighten his leg. Swelling, redness, synovitis appears
Degree of damage to ZRMM and Stoller classification
A tomographic examination using an MRI machine according to Stoller does not require special preparation. Despite the rather high cost, the method is informative, and this irreplaceable research cannot be neglected.
Important! MRI cannot be performed if you have a pacemaker or a metal artificial implant. All metal objects (piercings, rings) must be removed before the study. Otherwise, the magnetic field will force them out of the body.
Damage is classified into 3 degrees of change according to Stoller.
- First degree. It is characterized by the appearance of a point signal in the interarticular cartilaginous plate. A slight violation in the structure of the meniscus.
- The second degree includes a linear formation that has not yet reached the edge of the meniscus. ZRMM crack.
- Third degree. Stage 3 is characterized by a tearing signal reaching the very edge of the meniscus, in other words, its rupture.
The accuracy of MRI data in diagnosing rupture of the spinal cord is 90-95%.
Meniscus treatment
The choice of appropriate therapy for a particular patient is based on a combination of several factors - age, concomitant diseases, characteristics and extent of the rupture. Taking into account all the data obtained during diagnosis, the doctor prescribes appropriate conservative treatment if the cartilaginous structure is not destroyed, there is no pinching, displacement, there are no ligament ruptures and the meniscal tissues are fused.
Treatment for stage 2 lesions
Conservative treatment is suggested for degenerative damage to the menisci of grade 2 according to Stoller, if the tears are minor (no more than 10 mm), joint stability is maintained, and the area has a good blood supply. Among the medications, chondroprotectors are prescribed to help regenerate and improve metabolism in the joint. Inflammatory processes are controlled by NSAIDs; for severe pain, analgesics are prescribed. Grade 2 damage to the posterior horn of the medial meniscus is repaired using arthroscopic technique using the meniscal suture method - connecting parts of the cartilage by suturing the tears. For areas devoid of blood vessels, the second method is recommended - partial resection (partial removal) of destroyed tissue.
Symptoms
The clinical picture of damage to the posterior horn of the meniscus has the following features:
- Injury can occur spontaneously from any sudden movement.
- Persistent, continuous aching pain that increases with joint movement.
- Slow increase in swelling above the kneecap.
- Locking of the knee joint is possible, resulting from a sudden movement, that is, flexion-extension.
The symptoms are expressed rather weakly, and the degree of degenerative changes in the cervical tumor according to Stoller can only be determined after an X-ray or MRI image.
Traumatic damage to the MRMM
Based on the name, it is not difficult to understand that the cornerstone is a knee joint injury. This type of injury is typical for the younger age category of people, that is, under 40 years of age. Meniscus injuries occur in the following cases:
- when jumping from high;
- when landing sharply on your knees;
- torsion on one leg leads to rupture;
- running on uneven surfaces;
- subluxation of the knee joint.
You can independently determine the injury of the cervical mucosa, regardless of the level of the pain symptom, using the following techniques together:
- Bazhov's technique. During extension of the joint and when pressing on the back side of the kneecap, the pain intensifies.
- Land's sign. In a supine position, the palm of the hand should pass under the injured knee with gaps - freely.
- Turner's sign. The sensitivity of the skin around the knee increases.
Painful sensations come in three degrees of severity, with accompanying symptoms.
- Mild 1st degree. There is no obvious pain, no restrictions in movement are felt, only with certain loads a slight increase in pain is felt, for example when squats. There is slight swelling above the kneecap.
- Moderate 2nd degree of severity. Accompanied by severe pain. The patient walks with a limp, with periodic blocking of the knee joint. The position of the leg is only in a half-bent state; it is impossible to straighten the leg even with help. The swelling intensifies, the skin takes on a blue tint.
- 3rd degree of severity. The pain is unbearable and sharp. The leg is bent and motionless, there is severe swelling of a purple-violet color.