Antibiotics are substances of biological or semi-synthetic origin. They are used in medical practice to combat pathogenic microbes and viruses. Before the advent of these medications, typhoid fever, dysentery, pneumonia, and tuberculosis had the status of incurable diseases. Today, treatment of infectious diseases is possible with the use of 1-6 generations of antibiotics.
At this moment, the pharmacological industry produces more than 2000 varieties of drugs of this type. Doctors have described the effects of about 600 positions, and about 120-160 drugs are used in medical practice.
Important! For any disease, it is recommended to take antibiotics after consulting a doctor. Otherwise, antibiotic resistance may develop (decreased sensitivity of pathogenic microorganisms to antibacterial agents).
Classification of antibiotics
All antibacterial agents can be divided into 5 categories according to their characteristics and range of application. Let's take a closer look at this classification:
Mechanism of action:
- Bactericidal - the active substances of the drugs completely destroy bacteria and viruses. After taking such strong drugs, all pathogenic microflora in the human body dies.
- Bacteriostatic – inhibits the growth or spread of viruses. Thus, the cells remain “alive” without forming pathogenic flora.
Osteotropic antibiotics: what they are and what they are used for
Osteotropic antibiotics are often used in dental practice. An antibacterial drug (ABP) is prescribed:
- to eliminate the inflammatory-purulent process (chronic and acute) with peristitis, abscess, odontogenic sepsis, pericoronitis;
- as a prophylaxis against infectious complications after implantation and surgery;
- patients at risk (patients with diabetes, cardiovascular problems).
Antibacterial therapy is contraindicated for surgical interventions on bone tissue, bleeding, and large-area wounds in the oral cavity.
Spectrum of action
There are antibacterial agents:
Antibiotics for gumboil and inflammation of tooth roots -
Let's look at what antibiotics can be used for adults for gum gum disease. The choice here is quite large, for example, ranging from inexpensive antibiotics - such as lincomycin or amoxicillin, to more expensive drugs (for example, β-lactam antibiotics, 2nd generation fluoroquinolones and macrolides). Below we will look at the most popular antibiotics and tell you whether they work well for this type of dental inflammation.
1) Amoxiclav (or Augmentin) - these drugs contain a combination of “the antibiotic amoxicillin and clavulanic acid.” Many modern pathogenic bacteria produce β-lactamase enzymes that destroy amoxicillin. Clavulanic acid protects amoxicillin from the action of beta-lactamases, which greatly increases the effectiveness of the antibiotic. But using the most common amoxicillin (without combination with clavulanic acid) is pointless in dentistry.
The dosage regimen for adults is 500 mg 2-3 times a day (2 or 3 times depending on the severity of inflammation), the duration of administration is usually 5 days, but if necessary, the doctor can extend the drug for another 2-3 days. A package of the antibiotic Amoxiclav (15 tablets of 500 mg) costs from 330 rubles, and a package of the antibiotic Augmentin (14 tablets of 500 mg) costs from 180 rubles. And we do not recommend purchasing their Russian analogues containing a combination of “amoxicillin and clavulanic acid,” especially since they will not be cheaper.
Important: if you decide to purchase inexpensive amoxicillin (without clavulanic acid), then it should be used at least in combination with the antibiotic metronidazole (Trichopol). The latter is taken for purulent infections according to the same regimen - 500 mg 3 times a day (5-7 days in total). Only in this case can we expect at least some acceptable effectiveness from the treatment.
2) Ciprofloxacin (Tsiprolet) - this inexpensive, popular antibiotic belongs to the 2nd generation fluoroquinolones. The recommended regimen for use in adults is 500 mg 2 times a day (for 5 days), and the cost of a package of the Indian-made drug will be about 120 rubles. It works well for apical periodontitis, i.e. inflammation at the apex of the tooth root. In addition, the risk of developing diarrhea with this drug is lower - compared to β-lactam antibiotics (Amoxiclav, Augmentin).
Antibiotic Tsiprolet (10 tablets, 500 mg each) –
However, if we are talking about long-term apical periodontitis (especially if there have been cases of a fistula with purulent discharge in the projection of the tooth root), if there is acute pain indicating the formation of a purulent abscess at the apex of the tooth root, it would be optimal to prescribe an antibiotic containing the combination “ciprofloxacin” + tinidazole." These are drugs - “Ciprolet-A” or “Tsifran-ST”, in which, in addition to 500 mg of ciprofloxacin, each tablet also contains 600 mg of tinidazole.
Tinidazole is an antibacterial drug with antiprotozoal activity, i.e. it is effective against anaerobic microorganisms (which are especially numerous during the formation of pus at the site of inflammation). In addition, tinidazole is very effective against Clostridium difficile and Clostridium perfringens, which are responsible for the development of diarrhea while taking antibiotics, and thus, when taking combination antibiotics with tinidazole, diarrhea is practically excluded.
3) Azithromycin (Azitral) - it is usually prescribed for allergies to β-lactam antibiotics (for example, amoxicillin). There are different regimens of use, but according to studies for purulent odontogenic infections, the optimal treatment regimen is to take a single dose of 1000 mg for 1 day, after which the drug is taken for another 2 or 3 days at a dose of 500 mg once a day. But the price of this antibiotic will be high if we do not take into account Russian manufacturers.
For example, a good Indian drug with azithromycin “Azitral” will cost you 220 rubles per package of 3 capsules of 500 mg (it turns out that you will need to purchase 2 packages for the course). The short course of use is due to the fact that this antibiotic has a cumulative effect, and therefore, even after taking it, therapeutic concentrations of the antibiotic remain in the body for several days.
Is it worth using Azithromycin for complications of caries (apical periodontitis, swelling or fistula on the gum, or gumboil on the face) - it’s definitely not worth it. This is due to the fact that in patients with inflammation at the apex of the tooth, drugs with azithromycin show good effectiveness only in 50% of cases, and in the remaining half of patients, the sensitivity of the microflora in the inflammation site to azithromycin is regarded as “low”. Below we will also demonstrate scientific works that confirm this.
4) Lincomycin or Clindamycin are quite old antibiotics belonging to the lincosamide group. Moreover, clindamycin is a more effective analogue of lincomycin (in terms of effectiveness against certain types of pathogenic bacteria that cause purulent inflammation, it is 2-10 times more effective than lincomycin). The peculiarity of these antibiotics is a certain affinity for bone tissue, which is an advantage for purulent inflammation in the teeth, as well as their low price. The disadvantages include a narrow spectrum of antimicrobial action, as well as the fact that they often cause diarrhea.
The regimen for taking Lincomycin is 2 capsules 3 times a day, for a total of 5 days (a package of the drug costs only 60 rubles). Clindamycin dosage regimen: 1 capsule 150 mg 4 times a day for 4 days. The latter is the drug of choice for allergies to β-lactam antibiotics, which include penicillins, amoxicillin, cephalosporins, etc. Affordable price – pack of 16 tablets. 150 mg each (made in Serbia) costs approximately 160 rubles. To prevent diarrhea while taking antibiotics, they should also be combined with tablets. Metronidazole.
Is it worth using Lincomycin - modern studies show that lincomycin shows good effectiveness only in 36.8% of cases (in at least 63.2% of cases, pathogenic bacteria at the site of inflammation have only weak sensitivity to lincomycin). Moreover, if we are talking about a long-existing focus of inflammation in the area of the tooth root (in the presence of a fistula or purulent abscess), lincomycin is effective only in 19% of cases, at the same time in 47.6% of cases it demonstrates only weak effectiveness, and in 33. 4% of cases – patients have complete resistance of the microflora in the inflammation site to lincomycin.
Summary (which antibiotic is better for inflammation at the root of the tooth) –
To compare the effectiveness of antibiotics in this article, the author of the article used personal experience in prescribing them, as well as the scientific work “Sensitivity of microbial associations of exudate of a periodontal pocket and odontogenic lesion to antibacterial drugs” (Makeeva I.M., Daurova F.Yu.), which was performed in 2016 at the Medical University. Sechenov, Moscow.
From this work we learn the following. In patients with apical periodontitis (inflammation at the apex of the tooth root), antibacterial drugs with the combination of amoxicillin + clavulanic acid were highly effective in 79-80% of cases, for ciprofloxacin (without tinidazole) - in 76% of cases, for azithromycin - from 66 % to 52% of cases, and for lincomycin - only from 36% to 19% of cases. Thus, if you have swelling of the gums or gumboil on your face, or there is acute pain when biting on a tooth, you should definitely not use lincomycin or azithromycin.
The 1st choice drugs are 2nd generation fluoroquinolones, namely the antibiotic ciprofloxacin (you can use the usual “Tsiprolet”, but the best drugs are those where ciprofloxacin is combined with tinidazole - these are “Ciprolet-A” or “Cifran-ST” ). Moreover, the last 2 drugs are the first choice drugs also for those patients who have a history of diarrhea during antibacterial therapy. In second place are β-lactam antibiotics such as Amoxiclav or Augmentin, which can be used as monotherapy or in combination with metronidazole (to enhance the effect in purulent inflammation).
If we are talking about the need for antibacterial therapy in a hospital setting (purulent abscesses, phlegmons, odontogenic osteomyelitis, etc.), then the drugs of first choice will be antibiotics of the cephalosporin group (i.m.), for example, the antibiotic Ceftriaxone.
Important: Remember that you should not take antibiotics on your own without a doctor's prescription. The choice of antibiotic is made by the doctor, taking into account the specific situation in the oral cavity, the severity of purulent inflammation, and also taking into account your chronic diseases. Antibiotics for gum gum disease are prescribed immediately after opening the tooth by a dentist, as well as after making a small incision in the gum (if necessary). But antibiotics cannot be a replacement for these medical procedures, because... Antibiotics are not able to “sterilize” infection in root canals and around the apex of the tooth.
Treatment with antibiotics for swelling of the gums near a tooth or acute pain when biting on a tooth is not the main treatment. If it is possible to save a tooth, the root canals must first be opened (to create an outflow of purulent discharge from the source of inflammation at the apex of the tooth root). And only after this are antibiotics prescribed. If you use an antibiotic just to suppress inflammation, you create a situation in which the infection at the site of inflammation becomes resistant to the antibiotic, and subsequent exacerbations of inflammation will be much more serious.
Antibiotics for toothache -
Tooth pain is a consequence of either inflammation of the nerve in the tooth (this disease is called pulpitis) or inflammation at the apex of the tooth root (apical periodontitis). Antibiotics for toothache do not quickly reduce it, because... they do not have an analgesic effect. True, they can reduce pain indirectly - by reducing inflammation, but this effect will develop for so long that it does not have any clinical significance.
An effective remedy for relieving toothache are non-steroidal anti-inflammatory drugs (NSAIDs), which include Nurofen, as well as other much stronger analgesics. You should start taking antibiotics before visiting the dentist only in one case, for example, if in the evening or at night you have acute pain when biting on a tooth or swelling of the gums/face, but you are planning an urgent visit to the dentist the next day.
By composition
Antibacterial drugs are divided into 6 groups:
- Penicillins are the first antimicrobial drugs, obtained back in 1928 from a biological substance (Penicillium fungi). For a long time they remained the most popular medicine for the treatment of infectious diseases.
- Cephalosporins belong to the group of the most powerful antimicrobial agents with a wide range of applications. They completely destroy pathogenic flora and are well tolerated by humans.
- Macrolides are the name of a group of narrow-range antimicrobial agents. They do not destroy the diseased cell, but only stop its growth. This category includes the following drugs: erythromycin, spiramycin, azithromycin.
- Tetracyclines are good drugs for the treatment of infectious diseases of the respiratory and urinary tract.
- Fluoroquinolones are antimicrobial agents with a wide range of effects. Completely destroy pathogenic microorganisms. You can find 1st-2nd generation medications on sale. Doctors usually prescribe them to combat Pseudomonas aeruginosa.
- Aminoglycosides are antimicrobial drugs with a wide range of applications. Popular drugs in this group - streptomycin (therapy of tuberculosis, plague) and gentamicin - are used as ointments, eye drops, and injections for ophthalmic infections.
Generations of drugs. Advanced antimicrobial drugs already have six generations. For example, penicillin was the first drug of natural origin, while the third or sixth generation is an already improved version, which includes the strongest inhibitors. The relationship is direct: the newer the generation, the more effective the effect of drugs on pathogenic microflora.
By method of administration. Oral – taken by mouth. These are various syrups, tablets, soluble capsules, suspensions. Parenteral - administered intravenously or intramuscularly. They work faster than oral medications. Rectal medications are injected into the rectum.
Important! Taking antibiotics is allowed only after consulting a doctor, otherwise antibiotic resistance will develop.
Injections of antibiotics into the gums –
I would like to say a few words about such a treatment method as injections of antibiotics into the gums. This method of treatment has never been used abroad due to the enormous harm that such injections cause to the gums. In Russia, this method of treatment was previously very common due to its low cost and low qualifications of dentists (in conditions where the treatment of periodontal diseases is not carried out by periodontologists specially trained for this, but by any ordinary dentist).
Below we will explain why, if a clinic offers you a course of antibiotic injections into your gums, you should immediately run away from this clinic and look for another clinic/another doctor. The visible part of the treatment is basically that injections into the gums can actually lead to a decrease in the intensity of inflammation (bleeding, pain, swelling and redness of the gums are reduced). Although some patients may already experience gum abscessation at this stage, this is especially common in the presence of deep periodontal pockets.
Injecting an antibiotic directly into the gum results in the creation of a terrifyingly high concentration of antibiotic in the gum and bone tissue around the tooth. The antibiotic lincomycin is usually prescribed. In low concentrations it is bacteriostatic, but in high concentrations it begins to have a bactericidal effect, which leads to the immediate destruction of a very large number of pathogenic microorganisms (and not gradually, as it should be). The death of pathogenic bacteria is always accompanied by the release of a large number of toxins, various pathogens, as well as so-called “cytokines” (inflammatory mediators).
When too many of them are thrown out at the same time, this leads to the appearance of multiple foci of necrosis in the periodontium (the periodontium is the ligamentous apparatus of the tooth, with the help of the fibers of which the tooth is connected to the bone tissue). Such areas of necrosis heal with the formation of scar tissue, the formation of which initially gives the appearance of strengthening the tooth, but, unfortunately, the joy does not last long. Normal periodontium of teeth is adapted to bear a large mechanical (chewing) load, which cannot be said about scar tissue. And as soon as the area of attachment of the tooth to the bone decreases due to the normal periodontium, a mechanical overload of the ligamentous apparatus of the tooth occurs.
As a result, the bone tissue around the tooth begins to dissolve, which leads to an even greater increase in its mobility. Moreover, in this case, mobility will no longer be associated with inflammation, but with a decrease in bone level, as well as a decrease in the area of periodontal attachment of the tooth root to the bone. And this is irreversible mobility, which cannot be corrected by any treatment.
New generation antibacterial agents
The difference between the latest generations of antibiotics and their earlier versions is a more advanced formula of the active substance. Active components specifically eliminate only pathological reactions in the cell. For example, new generation intestinal antibiotics do not disrupt the microflora of the gastrointestinal tract. At the same time, they fight an entire “army” of infectious agents.
The newest antibacterial drugs are divided into five groups:
- Tetracycline – tetracycline.
- Aminoglycosides – streptomycin.
- Penicillin series - amoxicillin and others.
- Amphenicols – chloramphenicol.
- Carbapenem group – meropenem, imipenem, invaz.
Let's consider several well-known antimicrobial agents of imported and Russian production.
Amoxicillin is an imported antimicrobial drug from the penicillin group. Used in medical practice to treat bacterial infections. Effective for intestinal infections, sinusitis, sore throat, Lyme disease, dysentery, sepsis.
Avelox is the latest generation of medications from the group of fluoroquinolones. It has a strong effect on bacterial and atypical pathogens. Does not harm the kidneys and gastrointestinal tract. Used for acute and chronic diseases.
Cephalosporins are third generation antibiotics. This group includes Ceftibuten, Ceftriaxone and others. Used to treat pyelonephritis and pneumonia. In general, these are safe products with few side effects. However, they should be taken only after consulting a doctor. There are many medications, but a specialist will recommend which one to choose.
Doriprex is an imported antimicrobial drug of synthetic origin. Showed good results in the treatment of pneumonia, advanced intra-abdominal infections, pyelonephritis.
Invaz is an antibacterial agent from the carbapenem group. Available in ampoules for parenteral administration. Shows a rapid effect in the treatment of bacterial disorders of the skin, soft tissues, urinary tract infections, pneumonia, septicemia.
Augmetin is a third generation semi-synthetic penicillin with the addition of enhancing inhibitors. Pediatricians recognize it as the best comprehensive medication for the treatment of childhood sinusitis, bronchitis, tonsillitis and other respiratory tract infections.
Cefamandole is a Russian-made antibacterial agent. Belongs to the group of third generation cephalosporins. Used to treat intestinal infections, pathogens of genital infections. As an antimicrobial agent with a wide range of effects, it is used for colds.
Indications for prophylactic antibiotics
Antibacterial drugs may not always be prescribed during implantation. For example, when installing artificial roots without tilting the mucoperiosteal flap, antibiotics are usually not prescribed. This is due to the low traumatic nature of the operation, in which even no stitches are applied. In other cases, antibiotics are mandatory for dental implantation. Among the indications:
- simultaneous installation of several root substitutes with the formation of a large flap;
- replanting of bone material simultaneously with implantation;
- ridge augmentation (hard tissue augmentation) using grafts or own bone blocks transplanted from another location;
- multiple simultaneous implantation with immediate loading of artificial roots with temporary or permanent crowns;
- the use of closed or open sinus lift when installing implants under the maxillary sinuses.
Antibiotics for all types of dental implantation can also be prescribed for unsatisfactory initial oral hygiene, installation of root substitutes against the background of periodontitis, and chronic diseases of the nasopharynx.
The best broad-spectrum antibacterial drugs
New generation antimicrobial agents are usually synthesized from natural raw materials and stabilized in laboratories. This helps enhance the effect of the drug on pathogenic microflora.
What drugs are the most powerful? Doctors classify these as broad-spectrum antibacterial agents. Below is a short list of drugs by name:
- AMOXICLAV - belongs to the group of aminopenicillins. It has a mild effect and is used to treat infectious diseases. The drug can be used with caution and only after consultation with a doctor during pregnancy, as well as during breastfeeding. Available in tablets or in bulk form for oral administration, as well as in powders for injection.
- SUMAMED is a popular antimicrobial drug for the treatment of infections of the gastrointestinal tract, genitourinary system, respiratory tract diseases - sore throat, bronchitis, pneumonia. It affects the liver and kidneys, so it is not prescribed for patients with hypersensitivity to macrolides.
- CEFOPERAZONE – belongs to the group of cephalosporins. Prescribed by doctors for the treatment of urinary tract infections, prostatitis, skin disorders, and respiratory diseases. A good drug for recovery after gynecological, orthopedic and abdominal surgeries. Available in a form for parenteral administration - injection.
- UNIDOX SOLUTAB is the latest generation tetracycline. Used for extensive treatment of gastrointestinal infections, colds, prostatitis. It acts gently, without causing dysbacteriosis.
- LINCOMYCIN is a drug prescribed for the treatment of osteomyelitis, sepsis, and staphylococcal infections. It has a strong effect on pathogenic cells, therefore it has a long series of side effects. Among them are hypotension, weakness, dizziness. Do not use during pregnancy, or in patients with hepatic-renal insufficiency.
- RULID is a fourth generation macrolide. The main substance is roxithromycin. Prescribed for urogenital infections, diseases of the gastrointestinal tract and upper respiratory tract. Available in tablets.
- CEFIXIM – by name, it is a drug from the group of cephalosporins. Has a bactericidal effect on pathogenic cells. Helps with gastrointestinal infections, prostatitis, and also treats colds. It is quite toxic, so it should not be taken if you have kidney or liver problems.
- Cefotaxime is the last group of cephalosporins. The drug is indicated for the treatment of gynecological, urological, and colds. It copes well with inflammatory processes and suppresses pathogenic microflora.
Possible consequences of violating prophylactic antibiotic therapy
After implantation, tissue swelling occurs and pain may be bothersome. Taking antihistamines and painkillers helps eliminate these consequences. But these groups of medications will not be able to cope with pathogenic microbes. Infectious inflammation does not develop immediately, so some patients believe that an antibiotic is not necessary. But if the prescribed regimen for taking the antibacterial drug is violated, peri-implantitis may occur - inflammation of the tissues surrounding the artificial root. In this case, the full engraftment and stability of the implant cannot be guaranteed, and in case of failure, the patient will have to take responsibility. But when taking antibiotics, the risk of developing an inflammatory process is significantly reduced.
Summary
We reviewed Russian and imported broad-spectrum antibiotics and briefly described the classification of drugs. Let's answer the question: which antibacterial agents to choose?
It is important to understand that antimicrobial drugs for extensive use are toxic and therefore negatively affect the microflora. In addition, bacteria mutate, which means the drugs lose their effectiveness. Therefore, antibacterial agents with the latest structure will be a priority over their earlier counterparts.
Self-medication with antibiotics is dangerous to health. In case of an infectious disease, the first step is to consult a doctor. The specialist will determine the cause of the disease and prescribe effective antibacterial agents. Self-medication “at random” leads to the development of antibiotic resistance.
Dental antibiotic in adult and pediatric dentistry - features
Antibacterial agents have proven themselves in the treatment of various diseases caused by infections and pathogenic microbes. They are used to eliminate the inflammatory and infectious process in the oral cavity and maxillofacial region, as well as to suppress pathogenic microflora.
This group of drugs is used in the treatment of chronic and acute pathologies (implantation, surgery, periodontology, dentistry).
Dental antibiotics are prescribed for the following complications and infections:
- tooth abscess - an inflammatory process of the roots with abundant accumulation of pus;
- various inflammatory and purulent processes;
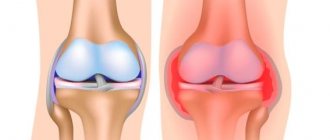
- periodontitis – inflammation of connective tissues (periodontal);
- pulpitis - a symptom of advanced caries, which often leads to the destruction of hard tissue;
- before surgery - to prevent inflammatory processes and complications;
- gumboil - gum disease.
In some cases, the drug is prescribed after tooth extraction and for the prevention of dental disease. The effect of the drugs is different. Use: to disrupt the formation of supporting polymers of cell walls, block the actions of microorganism enzymes, accumulation in bone tissue. Antibiotic therapy has also proven itself in pediatric dentistry.
Commonly used drugs for inflammation
In dentistry, several types of antibiotics are used for toothache and inflammation.
- Penicillin group. Prescribed at any age, with minimal side effects and easy tolerability. The main use is for periodontal inflammation. Effective against anaerobic bacteria.
- Cephalospoirins. They are used when it is necessary to perform dental manipulation with the risk of injury, as well as during periodontal and odontogenic inflammatory processes.
- Tetracyclines. Relieves swelling in the area of bone and soft tissue.
- Imidazole and derivatives. They have a depressing effect on pathogenic microorganisms and quickly penetrate bone tissue. Recommended for extensive inflammatory lesions.
- Macrolides. Used during pregnancy and allergies to drugs of the penicillin group. Eliminates gram-negative and gram-positive bacteria.
- Lincosamides. Do not cause allergies. Used for severe bone tissue infections.
The prescription of osteotropic antibiotics is combined if the tests reveal different types of pathogenic microbes.
Side effects and contraindications
Despite the fact that the antibiotic has proven itself well for toothache and inflammation, its use is contraindicated in case of kidney and liver pathologies, diabetes mellitus, and taking certain medications. Prescribed with caution to children, elderly patients, and pregnant women.
Possible side effects:
- dermatitis, urticaria, skin rashes and other allergic reactions;
- diarrhea, nausea;
- kidney and liver damage;
- headache;
- anemia;
- candidiasis of the mucous membranes.
Dental antibiotics are an irreplaceable thing. The drugs prevent a serious complication, but subject to the right choice and strict adherence to the doctor’s recommendations.
Author: Zhukov M.A.
Tetracyclines
Basic chemical structure of tetracyclines Like penicillins, they are one of the earliest classes of antibiotics. They were discovered in the 40s of the last century, but currently their use is limited. They have a bacteriostatic effect associated with disruption of protein synthesis in the microbial cell. Currently, many microorganisms have become resistant to tetracyclines, but drugs (natural tetracycline and synthetic doxycycline) remain important for rickettsiosis, chlamydial infections, and severe acne. Tetracyclines have a large number of side effects. They disrupt the functions of the gastrointestinal tract, affect the central nervous system (dizziness, increased intracranial pressure), cause metabolic disorders (impaired protein metabolism with a predominance of catabolism, increased azotemia), lead to disturbances in the formation of bone tissue, and cause allergic reactions that cross all tetracyclines. Tetracyclines have a very high hepatotoxic effect, up to the development of fatty degeneration or liver necrosis. Risk factors for hepatotoxicity include rapid intravenous administration of the drug, underlying liver dysfunction, pregnancy, and renal failure. When tetracyclines are taken orally simultaneously with antacids containing calcium, aluminum and magnesium, sodium bicarbonate and cholestyramine, their bioavailability may decrease due to the formation of non-absorbable complexes and an increase in the pH of the gastric contents. It is not recommended to combine tetracyclines with iron supplements, since this may interfere with the absorption of both. Carbamazepine, phenytoin and barbiturates increase the hepatic metabolism of doxycycline and reduce its concentration in the blood, which may require dose adjustment of this drug or replacement with tetracycline. When combined with tetracyclines, the effect of estrogen-containing oral contraceptives may be weakened. Tetracyclines may enhance the effect of indirect anticoagulants due to inhibition of their metabolism in the liver, which requires careful monitoring of prothrombin time. There are reports that when tetracyclines are combined with vitamin A preparations, the risk of pseudotumor cerebri syndrome increases.