What is gonarthrosis?
Gonarthrosis (syn. arthrosis deformans, osteoarthrosis, osteoarthritis, degenerative arthritis of the knee joint) is a polyetiological degenerative-dystrophic disease accompanied by joint deformation, destruction of hyaline cartilage, the appearance and growth of osteophytes, and loss of limb mobility. It leads in number among all arthrosis in the musculoskeletal system. The knee is a very important place of articulation of bones, because the possibility of free movement depends on it.
Fact!
Pathology of one department can deform another. For example, gonarthrosis worsens the condition of the spine.
The cause of primary damage to large joints is explained by the heavy daily load placed on them. Women suffer from arthrosis 10 times more often (due to hormonal characteristics). In 75% of cases, the part that articulates the femur and tibia is affected. The patellofemoral side is affected less frequently, but more often leads to disability. In practice, bilateral gonarthrosis occurs predominantly.
What are the differences between degenerative changes and lesions?
Degenerative processes in joints are not always dangerous. They are divided into changes and lesions:
- changes are a natural process of aging of joints, which does not have a serious impact on their functionality;
- lesions are a pathological condition that occurs at any age and leads to the development of arthrosis of the knee, shoulder or hip joint.
Degenerative lesions may have more than one cause, which overlap and reinforce each other. For example, the cartilage may be genetically defective, the joint may have anatomical defects or traumatic damage. The development of the disease is facilitated by overload, joint inflammation, and pathology of the endocrine system. One or more reasons trigger the mechanism of joint destruction from the inside.
Causes of the disease
Physiological aging is an inevitable process for living beings. Changes occur in all tissues, including bones, muscles, cartilage, etc. Against this background, joints weaken, become worn out, and lose flexibility and elasticity. This begins at the 40-year mark.
If for some reason the wear and tear of biological tissues accelerates, joint damage progresses faster, that is, with arthrosis, the process of destruction begins to predominate. Hormonal imbalance plays a special role in this - failure of the thyroid gland, menopause, taking hormones.
Cartilage loses its natural elasticity and density. It can no longer absorb movement and is gradually replaced by bone tissue, which grows in the form of spines - osteophytes. The functionality of the joint is lost.
The development of gonarthrosis is preceded by predisposing factors: mechanical, biological, physiological, etc.
The main reasons may be:
- Congenital anomalies of the knee joint - hypermobility, congenital dislocation of the patella, articular dysplasia, valgus and varus deformity;
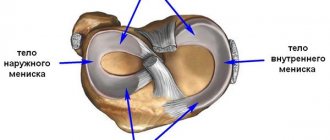
- Past injuries - menisci with displacements/ruptures, joints, local dislocations, sprains, bone diaphyseal fractures, knee surgeries.
- Metabolic disorders - obesity, hemochromatosis, gout, Wilson's disease.
- Endocrinopathies - thyroid disorders, diabetes mellitus, acromegaly.
- Changes in joints of a neurodystrophic nature.
- Inflammatory processes in the knee joint.
According to the etiology, gonarthrosis can be primary or secondary. In the first case, it is often hereditary or idiopathic in nature and occurs without external causes. Secondary gonarthrosis of the knee joint develops against the background of aging and various previous diseases.
Provoking factors include old age, female gender in menopause, obesity, physical inactivity, constant stress on the joints, professional activity with constant squatting or kneeling, previous injuries, inflammation, heredity (pathology of the type II collagen gene).
The disease can be provoked even by starting to exercise too actively after a long break. This is often done by retirees who decide to start leading a healthy lifestyle. Unprepared knee joints are easily injured and micro-tears occur in them. Even minimal damage ends in gonarthrosis, not to mention more serious injuries.
How does arthrosis develop?
Normal, healthy cartilage is elastic and smooth. These two properties allow the joint surfaces to move in relation to each other, thereby providing a sufficient level of shock absorption while reducing the load on all adjacent structures, such as the joint capsule, ligaments, muscles or bones.
When the disease occurs, cartilage loses its smoothness and elasticity, and its surface becomes uneven. As a result, the surfaces of the joints stop moving smoothly and begin to rub with any movement. After some time, particles can separate from the cartilage and penetrate into the joint, where they move inside the joint fluid, thereby compromising the integrity of the synovial membrane, further injuring the joint.
Symptoms of gonarthrosis of the knee joint
The most important symptom of damage is pain. It does not appear immediately, so early diagnosis is delayed, because as long as it doesn’t hurt, no one worries. A person does not think, for example, when climbing stairs, about the complexity of the biomechanics of movements in the knee joint. But when the pain comes, he begins to realize that he overcomes a huge number of steps a day and this is hard work.
So, among the initial signs of gonarthrosis are morning stiffness and minor discomfort (not even pain), which quickly disappear with movement. After the joint warms up, they disappear. This is characterized by the so-called “starting pain”. It manifests itself not only at the beginning of walking, but also when changing position, for example, getting up from a chair. As soon as the patient “diverges”, it will disappear, but after the load it will appear again.
There may be slight swelling of the joint, but without visible external changes. From time to time, when walking, clicking, creaking, weakness, and tingling sensations occur in the legs. All this is short-term in nature. The pain symptom is not very disturbing and the person comes to his senses already at stage II.
Gonarthrosis of the knee joint of the 2nd degree manifests itself with a more intense pain syndrome, which is localized along the anterior-inner surface of the joint. Pain occurs even with minor exertion and intensifies during intense walking. You can't confuse it with fatigue. After a long rest, it goes away for a while, but then resumes again.
Painful sensations in this phase already occur much more often and are more intense. With gonarthrosis, the flexion function is impaired, resulting in a limp. To help such a patient, doctors often resort to surgery even at this stage.
Crunching and creaking when walking are already obvious, movements become more limited, and when you try to bend your leg, sharp pain occurs. The joint becomes swollen and changes its configuration.
The third stage is characterized by permanent pain, including at rest and at night. The pain is constant, lameness progresses, and muscle atrophy begins. The patient needs supportive devices. At this stage, varus curvature of the legs is provoked, when the limbs acquire an O-shape, as they say, “legs like a wheel.”
Every movement provokes friction between the articular surfaces, which causes pain and disturbs sleep. The leg cannot bend or straighten. The gait becomes duck-like and a cane or crutches are required.
At this stage, the osteophytes are already massive; they often break off into the cavity of the joint capsule, which makes the pain even more unbearable. At this time, knee replacement surgery becomes vital and urgent. Otherwise, you will face excruciating suffering and life in a wheelchair.
The fourth stage is the end point. All functional articular structures have already been lost - the hyaline cartilage has been erased, there is no joint space left, the epiphyses of the bones are deformed, and the osteophytes have become large. Pain is not relieved by analgesics. A persistent flexion-extension contracture sets in - maximum loss of support, coordination and ability to move. The person finds himself confined to a wheelchair; at best, he moves with the help of a walker.
Important!
The consequence of gonarthrosis is often an increase in body weight and an increased risk of heart disease due to decreased physical activity.
The degree of self-care decreases sharply: not only walking is difficult, but also turning in bed, getting up, and sitting down. The patient constantly remembers, fears and expects pain. Usually, one of the joints suffers from irreversible changes to a greater extent than the second.
Symptoms of arthrosis
In order to accurately identify the disease, you need to know the main symptoms of arthrosis:
Pain
One of the most common symptoms of the disease at any stage is pain.
Pain appears even with the slightest exertion, when climate conditions change or at night. With prolonged stress on the joints (standing, running or walking), the pain becomes stronger, and with rest it subsides. These changes are due to the fact that the cartilage's ability to provide sufficient shock absorption during movement has decreased. The pain syndrome intensifies due to external factors such as a humid climate or low temperature. Starting pain
One of the key indicators is starting pain with arthrosis.
It appears at the moment the movement begins, and then disappears if the movement continues. Crunching
Another sign of arthrosis is the presence of a “crunching” in the affected joint, which becomes audible due to a decrease in the elasticity of the moving elements of the joint.
The more the disease progresses, the more pronounced the crunch will be felt. Each click is accompanied by pain. Deterioration of joint mobility
Deterioration of joint mobility is one of the main symptoms of arthrosis. At first, the pain does not bother a person, but as it progresses, bone growths appear, which lead to the fact that the muscles begin to spasm, and the joint spaces disappear almost completely. This is the main reason for limb immobilization.
Diagnostics
An appointment with a doctor begins with listening to the patient’s complaints, which are of a specific nature. Next, a physical examination is carried out, which helps to detect the presence of joint deformation, smoothness of its contours, fluctuation, pain on palpation, and curvature of the limb.
To the preliminary diagnosis, the doctor adds instrumental examination methods, and sometimes laboratory ones. The first step or the simplest method is to x-ray the joint. It will show the degree of narrowing of the joint space, changes in the contours of the adjacent bones, and osteophytes.
X-ray signs of hoarthrosis by degree:
- Gonarthrosis of the knee joint 1st degree - the joint space is narrowed slightly; in some cases, unexpressed subchondral osteosclerosis is observed.
- Gonarthrosis of the knee joint 2nd degree - narrowing of the joint space exceeds the physiological norm by 2 times. Subchondral sclerosis is more pronounced; small bone growths are detected along the edges of the joint space/in the area of the intercondylar eminence.
- Gonarthrosis of the 3rd degree - the joint space is practically absent, there are zones of osteoporosis, the articular surfaces are deformed, subchondral sclerosis is replaced by necrosis, extensive osteophytes are characteristic.
The early stage is characterized by scarcity of tissue changes, so x-rays may be ineffective.
An ultrasound of the joint is performed, but it often does not provide a clear image and does not allow changes to be assessed. For such cases, a CT scan (if bone pathology is suspected) or MRI (if soft tissue damage is suspected) is prescribed. Change detection is 85-90% accurate. This study helps to detect even small osteophytes and cartilaginous growths.
Laboratory diagnosis of gonarthrosis serves only as an addition. With gonarthrosis, the composition of the synovial fluid changes: the level of calcium and phosphorus increases, which confirms the diagnosis.
Degenerative lesions look like this in stages:
- the amount of moisture in the cartilage decreases - it loses functionality;
- chondrocytes in cartilage tissue partially die and are not restored;
- the amount of protein glycons decreases – mainly chondroitin;
- blood circulation in the articular ends of bones is impaired;
- the biochemical composition of the synovial fluid changes;
- cartilage experiences even more moisture deficiency, loses elasticity, and becomes less stable;
- in the joint the balance of damage and recovery processes is disturbed - in the direction of damage;
- degenerative lesions start – arthrosis begins.
The whole process takes years. A person has no idea that his joints are damaged and deteriorating. At certain stages, it is still possible to stop the destruction and restore the water balance with the help of a synovial fluid prosthesis. Sometimes it is enough to increase your daily water intake to normal. But, if arthrosis has already been diagnosed, treatment cannot be avoided.
Every glass of beer instead of a glass of clean water is another step towards arthrosis
Conservative treatment of gonarthrosis of the knee joint
Such therapy will be effective in the early stages of the disease. The complexity of conservative treatment involves not only pharmaceuticals, but also non-medicinal methods, for example, physiotherapy, exercise therapy, exercises, wearing orthoses, etc. In any case, all treatment regimens and drug dosages are prescribed only by a doctor!
Early manifestations are quite effectively treated with the use of locally irritating ointments. During periods of exacerbation of pathology, nonsteroids, glucocorticosteroids, and analgesics are used.
PRP or plasma therapy can also help - intra-articular injection of your own plasma enriched with platelets. The result will be a reduction in inflammation and the launch of regeneration processes. After the acute process subsides, they switch to physical therapy, exercise therapy, massages, etc.
The drugs prescribed are chondroprotectors and drugs to improve microcirculation. This is already maintenance treatment.
During the period of remission, exercise therapy, massage of the muscles of the lower leg and thigh are indicated, which will help improve lymphatic drainage, relieve swelling, strengthen the muscular-ligamentous apparatus of the legs and slow down the progression of the pathology.
Physiotherapeutic procedures will also be effective: UHF, ultrasound, magnetic and laser therapy, electro- and phonophoresis with drugs, microwave therapy, ozokerite applications, inductothermy, sinusoidal modulated currents, etc.
It is impossible to completely eliminate arthrosis. Treatment stops or slows the progression of the disease, eliminates symptoms (pain, stiffness) and allows the patient to improve their quality of life. After a diagnosis of arthrosis is made, you have to monitor your joints and undergo preventive and symptomatic treatment for life.
Surgical treatment of gonarthrosis
Conservative treatment with its drugs and non-drug methods is effective only in the early stages of the disease. For advanced cases, the only option for salvation will be surgery. Direct indications for surgery are severe dysfunction of the joint, severe pain and loss of performance (full/partial).
Surgical treatment is essentially endoprosthetics, when a natural joint is replaced with a synthetic one. Endoprosthesis replacement is used for grade 3 and 4 gonarthrosis. It can be total or partial.
Another method of surgical treatment is arthroscopy. This is not only diagnostics, but also removal of disorders and defects inside the joint using the endoscopic method. The procedure is minimally invasive, that is, non-traumatic. It is used as a treatment for factors that provoke arthrosis - meniscus damage, ligament ruptures, etc.
Two more methods are corrective osteotomy and arthrodesis. In the first case, an artificial redistribution of the load on the joint is implied. In the second, surgical immobilization of the joint by connecting bone tissues together. This relieves pain, but the leg will only serve as a support.
The last two methods are rarely used. Only when endoprosthesis replacement is not possible.
Regardless of the type of operation (except arthroscopy), the patient undergoes rehabilitation for 3–4 months, and full recovery takes up to six months or more.
Endoprosthetics is the only method that, in advanced cases, relieves the patient of pain and disability caused by gonarthrosis. Modern knee replacement designs have been so improved that in most cases they serve patients for 20–25 years. But installing a prosthesis is an extreme method that should be used only after using all possible conservative methods, since preserving “your” joint is always better than installing an artificial one.
Fact!
At stage 4 of degenerative processes with bilateral damage, the pain syndrome is pronounced and “does not go away” either day or night, so “emergency” total bilateral endoprosthetics is performed.