Kinds
Idiopathic brachial neuritis
Idiopathic brachial neuritis is a disorder of unknown etiology with an asymmetrical arrangement of the brachial plexus. It occurs in all age groups, but is more common between the third and seventh decades. Men are more often affected than women. Intervening events occurring days or weeks before the onset were noted in 28-83% of cases in various ways. Respiratory infections, influenza-like illnesses, immunizations, surgery, and emotional stress were common symptoms, with no triggers found in half of the cases. Idiopathic brachial neuritis is more common in men who engage in vigorous athletic activities such as wrestling, weight lifting, and gymnastics.
The pathophysiology of idiopathic brachial neuritis is not fully understood, and the disease is considered an immune-mediated disorder.
Idiopathic hypertrophic brachial neuritis
This disease is uncommon and tends to gradually affect the brachial plexus. The disease continues for several months or even years, and gradually progressive weakness and wasting of the segments affected by this disease is a key, but at the same time, often ignored symptom.
This disease differs from the above-described idiopathic brachial neuritis in its painless course, although some patients may have minor pain and weakness.
Hereditary neuralgic amyotrophy
Hereditary neuralgic amyotrophy is an autosomal dominant disorder characterized by repeated episodes of paralysis and sensory impairment of the affected limb, preceded by severe pain. Hereditary neuralgic amyotrophy is genetically linked to chromosome 17q25, where mutations in the septin-9 gene have been found. Hereditary neuralgic amyotrophy is a rare disease and its worldwide prevalence is unknown.
Onset of hereditary neuralgic amyotrophy occurs at birth or later in childhood, with a good prognosis for cure. However, individuals with hereditary neuralgic amyotrophy may have permanent residual neurological deficits after repeated attacks.
Neurogenic thoracic outlet syndrome
Neurogenic thoracic outlet syndrome is characterized by pain, paresthesia, and weakness of the upper extremities, which may be aggravated by raising the arms or frequent movements of the head and neck. This is usually seen in women.
Cancer-associated brachial plexiopathy
Brachial plexus involvement is a well-known complication of cancer. Pectoral plexopathy in such cases may be caused by metastatic spread or a consequence of radiation therapy for cancer.
Traumatic form of brachial plexopathy
Trauma is one of the most common causes of brachial plexopathy. These injuries usually result from a motorcycle or high-speed traffic accident, a fall from a significant height, or an impact. This can occur with penetrating trauma and gunshot wounds. This may be the result of iatrogenic trauma. In injured patients, the consequences should be carefully assessed. Determine the extent of head, neck and shoulder injuries. With open injuries, there may be damage to large blood vessels and lungs, in which case urgent surgical intervention is necessary.
Arthroscopic release of the transverse scapular ligament
Arthroscopic decompression of the suprascapular nerve in the suprascapular notch and spinoglenoid groove has found widespread use in clinical practice. It provides the opportunity for good visualization of neurovascular structures, more accurate tissue dissection under arthroscopic magnification, and less severe pain in the postoperative period, since the tissues are subject to less trauma and the attachment site of the trapezius muscle remains intact.
Arthroscopic release of the suprascapular nerve is used both for isolated nerve damage and as part of arthroscopic restoration of massive rotator cuff injuries in order to prevent kinking when tensioning the repaired muscles.
Rehabilitation
During the first 2-3 days after surgery, a support bandage is prescribed for comfort. Pendulum exercises and exercises to restore range of motion begin immediately, and a gradual transition to full physical activity begins as the pain subsides.
Complications
The most common complications are persistence of symptoms due to incomplete release of the ligament, damage to neurovascular structures, or irreversible changes in the nerve due to its compression that developed before surgery. Good visualization and a clear understanding of the anatomy are key to performing these procedures safely.
Thorough hemostasis is achieved with the help of an arthroscopic pump that maintains the necessary pressure and fluid flow, as well as with hypotensive anesthesia. Gentle blunt spreading of the soft tissue around neurovascular structures also reduces the risk of injury.
Conclusion
Entrapment of the suprascapular nerve, isolated or against the background of another pathology (damage to the rotator cuff), is regarded today as one of the important causes of pain in the shoulder joint and dysfunction. The impingement may occur in the suprascapular notch or spinoglenoid groove.
As a result of compression of the suprascapular nerve, atrophy of both the supraspinatus and infraspinatus muscles develops in the suprascapular notch, while pathology at the level of the spinous glenoid groove is limited to damage to the infraspinatus muscle. It is important to carefully approach the diagnosis and take this condition into account in the differential diagnosis in order for the patient to achieve an optimal clinical outcome.
Causes
These nerves can be damaged by stretching, pressure, or cutting. A strain can occur when the head and neck are forced away from the shoulder, such as during a fall from a motorcycle or sometimes a car accident. In more severe cases, the nerves may become torn from the spinal cord. Pressure can occur when the brachial plexus between the collarbone and the first rib is damaged, which can occur during a fracture or dislocation. Swelling in the area from excessive bleeding or damaged soft tissue can also lead to injury.
Clinical picture
At the very beginning of the disease, sudden, constant and severe pain occurs in the shoulder girdle. The pain may radiate to the trapezius muscle, shoulder, forearm, or hand. The pain is usually diffuse, worsens at night and can cause night awakenings. The pain is described as very severe, aching, throbbing, radiating from the shoulder distally down or proximally up into the neck. The pain usually goes away on its own and lasts 1-2 weeks, although in some cases it can last longer.
Other symptoms include:
- Sensory disturbances.
- Muscle weakness.
- Muscular atrophy.
If the long thoracic nerve is involved in the pathological process, then the patient may have a “pterygoid scapula”, because this nerve innervates the serratus anterior muscle. Weakness may also be related to muscles innervated by a peripheral nerve, a combination of peripheral nerves, or the brachial plexus. The electromyogram shows extensive denervation of the damaged muscles. MRI may show nonspecific inflammation in the brachial plexus.
Diagnostics
Many adult injuries will not recover on their own, and early evaluation by physicians who are experienced in treating these problems is important. Some injuries can heal over time or with quality therapy. Recovery time may be weeks or months. When the situation is unlikely to improve, several surgical techniques can be used to improve recovery.
To decide which injuries are most likely to resolve on their own, your doctor will rely on several exams of your arm and shoulder to check muscle strength and feeling in different areas. Additional tests such as MRI scans or CT/myelography may be used. A nerve conduction study/electromyogram, a test that measures electrical activity transmitted by nerves and muscles, may also be performed.
In some cases where nerve repair does not occur, tendon transfer surgery may be performed.
Signs of illness
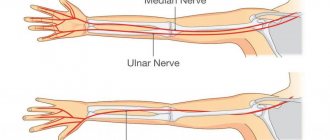
Pinching of various nerves (in particular, axillary, radial and median) can occur. As practice shows, during diagnostic examinations it is often determined that the radial nerve has been affected. It belongs to the nerve trunks, consisting of a motor and sensory part.
When a nerve is pinched in the shoulder, the symptoms may differ slightly from patient to patient (depending on the cause that provoked the disease). However, there are common characteristic features. First of all, the person experiences severe pain. It can be of a different nature (for example, sharp or aching), and occur even at rest, when there is no additional load on the shoulder. As a rule, it continues for a long time.
In general, all clinical manifestations are divided into three main groups: acute, subacute and chronic. Acute signs are characteristic of compression, which arose against the background of traumatic influence. Most often they accompany a fracture, sprain or rupture of ligamentous tendon tissue. Subacute symptoms are characteristic of complex pathologies of the musculoskeletal system (for example, deforming osteoarthritis).
Chronic symptoms are associated with degenerative-dystrophic diseases of the spinal column (for example, in the presence of cervical osteochondrosis with radicular syndrome). They are distinguished by painful sensations of a dull nature. They are constantly present, but due to limited mobility, a person often does not pay attention to them.
In accordance with the specifics of the lesion, experts note the following possible clinical manifestations:
- increased sweating (sweat increases during attacks of pain);
- crawling on the upper limbs and the area between the shoulder blades;
- a feeling of numbness in the thumb, index and middle fingers;
- restriction of movements in the joints of the hand after a night's sleep or a long rest;
- the appearance of involuntary muscle twitching;
- hyperemia and pallor of the skin;
- impaired skin sensitivity (pathological decrease in sensitivity) in the shoulder and forearm area.
The pathology does not pose a particular threat to the patient’s life, however, in the absence of proper therapy, the pathological process can progress to the point of muscle atrophy. Based on this, if the above-described signs are detected, you should not delay your visits to a neurologist.
Treatment
In most cases, treatment takes place on an outpatient basis, in severe situations - in a hospital. For plexopathy, anti-inflammatory therapy is carried out, painkillers, dehydrating drugs are used, and physiotherapeutic procedures are also prescribed. After the pain subsides, special exercises, massage, and a complex of vitamins are prescribed.
In more severe situations, surgical treatment is prescribed to eliminate the compression and restore the functionality of the plexus branches.
Survey
Clinical examination to confirm flexor pollicis longus and flexor digitorum profundus paralysis and index finger weakness. Clinicians should always perform a physical examination of muscles to detect muscle weakness in patients with SPT.
Personage-Turner syndrome affects:
- Muscle tone/mass – leads to atrophy of the infraspinatus, supraspinatus, deltoid, biceps, trapezius, serratus anterior, pronator teres and teres minor muscles
- Muscle strength – leads to weakness of the infraspinatus, supraspinatus, biceps, brachioradialis, pronator teres, trapezius, serratus anterior, teres minor muscles.
- Strength indicators will be normal in the following muscles: rhomboids, triceps, wrist and hand muscles.
- Sensitivity: numbness along the lateral side of the shoulder, forearm and in the area of the anatomical snuffbox.
- Reflexes: biceps brachii and brachioradialis.