Lumbar ischialgia is a term denoting pain in the lower back with irradiation into the buttock, into the leg, along the back of the leg. Pain may be accompanied by numbness and tingling in the area of innervation of the sciatic nerve. The term lumboischalgia (synonymous with lumbosacral radiculitis) refers only to pain syndrome and is not a diagnosis.
Luboischialgia is characterized by one or more symptoms:
- Constant pain only in the buttock or thigh on one side (less often in both legs)
- Pain worsens when sitting
- Burning or tingling sensation spreading down the leg
- Weakness, numbness, or loss of movement in the leg
- Constant pain on one side
- Severe pain that may make it difficult to stand or walk
Pain syndrome with lumbar ischialgia can be of varying intensity depending on the underlying disease that led to the development of lumbar ischialgia. Symptoms of lumbar ischialgia are caused by irritation of the sciatic nerve.
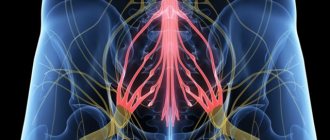
The sciatic nerve is the largest nerve in the torso and is made up of individual nerve roots that originate in the lumbar spine (at L3) and collectively form the “sciatic nerve.” The sciatic nerve runs from the lumbar spine to the leg. Parts of the sciatic nerve then branch in each leg and innervate specific parts of the leg - buttocks, thighs, calves, feet, toes.
Symptoms of lumbar ischialgia (lumbosacral radiculitis) such as pain in the leg, numbness, tingling, weakness may vary depending on where the nerve compression occurs.
The incidence of lumboischalgia (lumbosacral radiculitis) increases in middle age. Lumbar ischialgia rarely occurs under the age of 20; such pain syndromes are most likely at the age of 40-50 years, and in the older age group the likelihood of lumbar ischalgia decreases.
Often, specific events or injuries do not cause inflammation of the sciatic nerve, but over time the damage leads to the development of sciatica. In most patients, conservative treatment can be quite effective, and the pain syndrome decreases significantly within a few weeks, but in a certain number of patients the pain syndrome may be persistent.
Causes
There are 6 most common causes of lumbar ischialgia:
Herniated disc in the lumbar spine.
A herniated disc occurs when the soft inner core of the disc (nucleus pulposus) protrudes through the fibrous outer ring, affecting nearby nerve roots.
Osteochondrosis
Degenerative changes in the intervertebral discs are a natural involutional process that occurs as the body ages. Degenerative changes in the discs can lead to irritation of the roots and the development of pain.
Spondylolisthesis
This condition occurs when the vertebral arches are damaged (spondylolysis), resulting in the sliding of one vertebra in relation to another. Displacement of the vertebra causes damage and displacement of the intervertebral disc, which together can lead to irritation of the nerve roots and irritation of the sciatic nerve.
Spinal stenosis of the lumbar
This condition usually causes inflammation of the sciatic nerve due to narrowing of the spinal canal. Spinal stenosis in the lumbar region is most often associated with natural involutional changes in the spine and occurs in patients over 60 years of age. The condition usually results from a combination of one or more of the following factors: enlargement of the facet joints due to bony overgrowth, soft tissue overgrowth (ligamentous tissue), and disc bulging (herniated disc).
Piriformis syndrome
Irritation of the sciatic nerve can occur in the area in the buttock under the piriformis muscle. If there is a spasm of the piriformis muscle or other changes in this muscle, the sciatic nerve may be affected with the development of pain. And although this syndrome is an independent disease, pain in the leg can be similar to lumbar ischialgia.
Sacroiliac joint dysfunction
Irritation of the sacroiliac joint can also cause irritation of the L5 root, which exits at the top of the sacroiliac joint, and if there is a problem in this joint, inflammation of the sciatic nerve and pain may occur. Pain in the leg can be similar to that which occurs with lumbar ischialgia (lumbosacral radiculitis).
Other causes of lumbar ischialgia
A number of other conditions and diseases can cause inflammation of the sciatic nerve, including:
- Pregnancy. Changes in the body that occur during pregnancy, including weight, a shift in center of gravity, and hormonal changes, can cause inflammation of the sciatic nerve during pregnancy.
- Presence of scar tissue. If scar tissue presses on nerve roots, it can irritate the sciatic nerve
- Crick. In some cases, inflammation associated with muscle strain can put pressure on the nerve roots and cause inflammation of the sciatic nerve.
- Spinal tumors. A tumor in the spine (most often of metastatic origin) can have a compressive effect on the sciatic nerve.
- Infections. Infections rarely occur in the spine, but can also cause an impact on the roots with the development of inflammation of the sciatic nerve.
Examination in Samara for patients with pain on the inside of the knee
In most cases, it is advisable to conduct an EMG examination. Pinching of the sphenoid nerve may occur after vigorous movement rather than at rest. In this case, any examination other than an objective one will be useless. An objective/physical examination involves performing a rolling test on the inside of the knee in the area supplied by the sphenoid nerve. Patients with sphenoid neuralgia exhibit hyperalgesia.
Symptoms
As a rule, with lumbar ischialgia, symptoms occur on one side, and the pain starts from the lower back and goes down the back of the thigh down to the foot.
- Pain in the lower back is usually less intense than in the leg.
- Pain, as a rule, on one side of the lower back with irradiation into the buttock or thigh along the sciatic nerve - along the back of the thigh, lower leg and foot.
- The pain decreases when the patient lies down and when walking and intensifies when standing or sitting.
- The pain is acute and burning in nature.
- Some patients may describe a feeling of tingling, numbness, or weakness in the leg.
- Weakness or numbness when moving your leg.
- Severe or shooting pain in the leg that may make it difficult to stand or walk.
- Depending on the location of the effect on the sciatic nerve, pain may also occur in the foot and toes.
Symptoms of lumbar ischialgia depend on where the root compression occurs.
For example:
- L4 root - Symptoms will usually appear on the hip. Patients may experience weakness when straightening the leg and possibly a decreased knee reflex.
- L5 root – symptoms may occur in the big toe and ankle. Patients may feel pain or numbness in the top of the foot (between the big and second toe).
- S1 root – symptoms may appear on the outer part of the foot, radiating to the toes and little toe. Patients may experience weakness when lifting the foot or trying to stand on tiptoes. There may also be decreased ankle reflexes.
When several roots are compressed, a combination of symptoms is possible.
There are a number of symptoms that deserve special attention, as they require emergency medical attention, sometimes even surgical intervention. These symptoms are:
- Symptoms that continue to worsen rather than improve may indicate possible nerve damage, especially if neurological symptoms have progressed (eg, weakness in the leg).
- Symptoms of lumbar ischialgia occur in both legs and there are signs of bowel or bladder dysfunction, which may be a sign of cauda equina syndrome. For cauda equina syndrome, emergency surgery is indicated.
If you have these symptoms, you should immediately seek medical help.
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Dyachenko Ksenia Vasilievna
Head of the center for the treatment of dizziness and balance disorders.
The doctor is a neurologist of the highest category.
Angioneurologist. Neurorehabilitation specialist. Physiotherapist. Candidate of Medical Sciences.
Experience: 19 years.Volkova Svetlana Anatolevna
Head of the Center for Parkinsonism and Extrapyramidal Diseases.
The doctor is a neurologist of the highest category. Epileptologist. Ozone therapist. Physiotherapist. Experience: 26 years.
Polivanova Yulia Vyacheslavovna
The doctor is a neurologist. Ozone therapist. Physiotherapist Experience: 8 years.
Yushina Maria Alexandrovna
Head of the Center for Epilepsy and Paroxysmal Conditions.
The doctor is a neurologist. Epileptologist. Ozone therapist. Physiotherapist Experience: 7 years.
Ogurtsov Denis Alexandrovich
Traumatologist - orthopedist of the highest category. Candidate of Medical Sciences.
Experience: 23 years.
Treatment
In most cases, conservative treatment of lumbar ischialgia is quite effective. The range of treatment methods for lumbar ischialgia is wide and is aimed at reducing compression of the nerve roots and reducing pain. The most effective is the use of an integrated approach to the treatment of lumbar ischialgia and the use of a combination of various treatment methods (physiotherapy, massage, manual therapy, drug treatment, acupuncture and exercise therapy).
Drug treatment . The use of anti-inflammatory drugs (ibuprofen, naproxen, voltaren), COX-2 inhibitors (Celebrex) can reduce inflammation, which leads to a decrease in pain.
Epidural injections . If severe pain is present, an epidural steroid injection may be given. Epidural steroid administration differs from oral steroid administration in that the drugs are injected directly into the painful area around the sciatic nerve, which can quickly reduce inflammation and relieve pain. The effect of such a procedure is usually temporary, but it helps to relieve severe pain quite quickly.
Manual therapy
Modern gentle manual therapy techniques make it possible to restore the mobility of the motor segments of the spine, remove muscle blocks, improve the mobility of the facet joints and can sometimes significantly reduce compression of nerve fibers.
Acupuncture also helps reduce pain and restores conduction through nerve fibers.
Massage
Therapeutic massage methods can improve microcirculation, relieve muscle spasms, and also increase the body's production of endorphins.
Physiotherapy . Existing modern methods of physiotherapy (cryotherapy, laser therapy, ultrasound, electrophoresis) can reduce inflammation, improve blood circulation and thus reduce pain.
Exercise therapy . Physical exercises, which need to be included after pain has been reduced, allow you to restore the muscle corset and normalize the biomechanics of the spine, improve blood circulation in the motor segments. Physical exercises include both mechanotherapy (exercises on machines) and gymnastics, which allows you to develop both muscles and strengthen the ligamentous apparatus. Exercises for lumbar ischialgia must be selected with a physical therapy doctor (instructor), since independent exercises often lead to a relapse of symptoms.
Surgery
Indications for surgical treatment are the following factors:
- Severe pain in the leg that lasts for more than 4 to 6 weeks.
- Lack of effect from conservative treatment and persistence or worsening of neurological symptoms.
- Pain syndrome significantly impairs the patient's quality of life and the patient's ability to participate in daily activities
Urgent surgery is usually only necessary if there are progressive neurological symptoms (increasing weakness in the legs or sudden loss of bowel or bladder function).
Read also
Periarthrosis or periarthritis?
Let's imagine that you are driving a luxury car along our wonderful roads and suddenly notice that something persistently creaks in the area of the front wheel on the right.
Moreover, this creaking intensifies periodically,… Read more
Contracture
A fairly powerful word to hear, denoting the lack of full range of motion in a joint. The most common causes are prolonged immobilization of the joint. This is possible when after...
More details
Chest pain
The first thing a patient thinks about when he feels chest pain is a heart attack. Of course, chest pain is not something that can be ignored. But you need to understand that chest pain is not...
More details
Arm and neck pain
A man's neck hurt. He walks, periodically independently twists it from side to side, kneads it with one hand, then with the other... Brings his neck to the extreme degree of tilt to the left... then to the right... slowly... and...
More details
Osteoarthritis of the hip joint
In the vast majority of cases, this diagnosis can be suspected when the patient first enters the doctor’s office. The patient spares the affected leg, limping on it, transferring his body weight to the healthy leg, and...
More details