Foot pathologies are extremely common today, which is largely due to the lifestyle of modern people. One of the common disorders is arthrosis of the metatarsophalangeal joints, especially the 1st toe or hallux rigidus. It can be a complication of other orthopedic pathologies, age-related changes, or be the primary source of the development of other disorders. In any case, the disease can significantly reduce a person’s quality of life and cause him a lot of suffering. Therefore, it is important to promptly consult an orthopedist if signs of damage to the metatarsophalangeal joints appear.
Arthrosis of the metatarsophalangeal joints: what is it?
The metatarsophalangeal joints are ball and socket joints. They are formed by the articular surfaces of the heads of the metatarsal bones and the bases of the proximal phalanges. The ends of the bones that form the joint are covered with thin cartilage tissue. The articular capsules are attached along the edge of the articular cartilages and are thinned on the outside of the foot. On the opposite edge and sides they are strengthened by plantar and collateral ligaments, respectively. In this case, between the heads of the metatarsal bones there is a deep transverse metatarsal ligament.
The structural features of the metatarsophalangeal joints make them susceptible to the development of degenerative-dystrophic changes (arthrosis) and inflammatory processes (arthritis). Moreover, arthrosis is often complicated over time by the development of arthritis. This significantly worsens the well-being of patients.
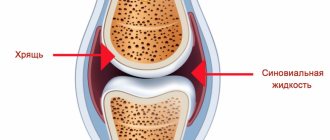
Arthrosis is called damage to the cartilage tissue covering the heads of the metatarsal bones and the bases of the proximal phalanges of varying degrees of severity. Initially, the cartilage becomes dehydrated and thins, becoming covered with microscopic cracks. But gradually, under the influence of loads or other factors, they increase in size and take on the appearance of large cracks and depressions. This leads to a decrease in the size of the joint space, which causes difficulties in movement and prevents the free sliding of the heads of the bones.
As a result, there is an increase in load and increased friction between bone surfaces. This is accompanied by the formation of osteophytes on them, i.e. bone growths. They may have sharp edges that will injure surrounding tissues and the joint capsule. As a result, over time, arthrosis of the metatarsophalangeal joints can be complicated by arthritis, that is, the addition of an inflammatory process.
Most often, arthrosis affects the metatarsophalangeal joint of the 1st toe or big toe. In this case, hallux rigidus is diagnosed. It is somewhat less common to diagnose arthrosis of the joint of the 2nd finger and extremely rarely of the others. This is due to the fact that the first finger bears the main load when walking, standing and physical activity.
The main danger of the disease is the occurrence of severe deformities of the joints, which will lead to a significant decrease or even complete loss of their functionality. As a result, patients may experience difficulty moving, even to the point of losing the supporting ability of the foot. The risk of local circulatory disorders also increases sharply. This increases the likelihood of developing varicose veins of the lower extremities.
Arthrosis and arthritis: what is the difference
Both diseases affect human joints. The quality of life of people who suffer from one of these illnesses is significantly reduced. Although the names of the diseases are similar, their symptoms and manifestations are very different.
Osteoarthritis affects the cartilage of the joint and nearby bones. It is more common in older people. It can be caused not only by age, but also by heavy physical labor or sports activities.
It is difficult to call arthrosis inflammation. But some doctors believe that it is precisely because of the inflammatory process that this disease begins to progress. The cartilage and bone tissues that are located near the joint undergo changes over time. This happens due to the stress that they experience every day. The disease develops slowly.
Arthritis is inflammation that occurs in a joint. It can almost completely destroy cartilage. Unlike arthrosis, this disease is more common among the young population.
The development of the disease and inflammatory process occurs due to autoimmune factors. That is, immunity independently affects the human body. This process can start due to genetic disorders or infectious diseases.
Inflammation is the culprit behind the onset of arthritis. Bacteria that infect the body's cells have antigens similar to its protein. Therefore, he begins to attack his own tissues. Most often, not only joints are affected, but also internal organs. It could be the heart or kidneys. Few people know that in this case, doctors recommend removing tonsils if a person often suffers from sore throats. Otherwise, there is a high risk of complications in the cardiovascular system and other organs.
If we compare arthritis with arthrosis of the foot, the second disease is more acute. Its symptoms are pronounced, so they are difficult to confuse with something else. Arthritis manifests itself in the form of swelling, severe pain, as well as other, not the most pleasant symptoms.
How the disease will develop in the future depends on the type of arthritis. Almost always, after an acute form, the disease “slows down” and then becomes chronic. Some changes in the joints remain forever, so new outbreaks of osteoarthritis are possible. Sometimes relapses occur and the disease again enters an acute form, joint pain and swelling appear, and the temperature rises.
Osteoarthritis, an inflammatory condition, can be controlled with anti-inflammatory medications. But osteoarthritis is much more difficult to treat, since it mostly remains in a chronic form, changing and destroying joints over a long period of time.
Causes
Arthrosis of the metatarsophalangeal joints is a polyetiological disease. It can occur in people of any age. But if for representatives of the older generation the development of degenerative-dystrophic processes in all joints of the body is an inevitable process, then for young people they are most often the result of injuries, active sports, and the wrong choice of shoes.
People of all ages and genders are susceptible to the development of arthrosis of the metatarsophalangeal joints, although they are more common in people over 45 years of age.
In general, the development of arthrosis of the metatarsophalangeal joints can be provoked by:
- metabolic disorders, including gout;
- circulatory disorders in the feet;
- systemic connective tissue diseases, in particular rheumatoid arthritis and lupus erythematosus;
- endocrine pathologies accompanied by hormonal imbalance, including diabetes mellitus, hyperthyroidism, hypothyroidism, etc.;
- foot injuries;
- flat feet;
- clubfoot;
- shortening of one of the legs due to the presence of hip dysplasia or other factors;
- excess body weight, which leads to a sharp increase in the load on the foot;
- prolonged, constant wearing of uncomfortable, tight shoes, especially high heels;
- the need to stand or walk for a long time, carry heavy loads;
- excessively active sports;
- prolonged hypothermia or even frostbite of the toes.
Hereditary predisposition plays an important role in the development of arthrosis of the metatarsophalangeal joints.
Thus, most often, arthrosis of the metatarsophalangeal joints most often affects people with obesity of 2-3 degrees, athletes, as well as elderly people who are forced to stand for a long time.
Brief description and mechanism of disease development
Arthrosis of the first metatarsophalangeal joint of the foot is a chronic degenerative-dystrophic disease of cartilage tissue. The lesion is localized in the lateral area of the big toe, so it is often commonly referred to as a bunion. The pathology affects men and women of different ages. According to statistics, it is more often recorded among representatives of the fairer sex after 50 years.
The mechanism of development of the disease is as follows:
- the firmness and elasticity of cartilage tissue is lost;
- the shock-absorbing function of cartilage decreases;
- constant loads on the joint during movement negatively affect tendons, ligaments, and muscles;
- microcirculation in soft tissues deteriorates;
- a growth (osteophyte) forms on the metatarsal bone;
- the structure and shape of the joint gradually changes;
- the mobility of the finger is limited with subsequent dystrophy of the foot.
As a result, the thumb loses functionality, the destructive process spreads to neighboring joints and leads to immobilization of the ankle.
Arthrosis of the metatarsophalangeal joint, like arthritis of the foot, is treatable, but for the correct choice of therapy it is important to find out the causes of the disease.
Arthrosis is a pathology during which early destruction of cartilage tissue occurs
Symptoms of arthrosis of the metatarsophalangeal joints
The disease is characterized by smooth progression. Therefore, it can develop completely unnoticed over several years, and at this time a person does not even suspect the presence of deviations from the norm in the condition of these small joints of the foot. Only in isolated cases, usually after injuries, does the disease begin acutely.
But gradually the intensity of the symptoms of arthrosis of the metatarsophalangeal joints increases. The disease is characterized by:
- the occurrence of pain that increases over time in the area of the bases of the phalanges of the fingers;
- the formation of subcutaneous dense protrusions that can be felt independently (this may be accompanied by painful sensations);
- swelling;
- gait disturbances in the form of instability, lameness, clubfoot;
- a sharp increase in pain in the foot when standing and walking;
- increased leg fatigue;
- limited mobility of affected joints;
- formation of calluses in the joint area.
Most often, arthrosis of the 1st metatarsophalangeal joint or big toe is observed. This is accompanied by the formation of a bone growth or exostosis in the projection of the affected joint (on the lateral surface of the foot). This kind of thing is usually called a bump or a bone.
In this case, the thumb gradually deviates towards the neighboring ones, and the callus increases in size. This is accompanied by severe pain, and swelling and redness of the soft tissues may also occur. The formation causes discomfort when wearing tight shoes, and over time, patients may notice that previously comfortable shoes or boots have become too tight. In the future, exostosis causes difficulties in choosing shoes, and a big toe that deviates from the normal axis provokes deformation of neighboring ones. Thus, arthrosis of the 1st metatarsophalangeal joint can lead to the development of hallux valgus.
Clinical picture
Symptoms of the disease increase over several years. The first signs are often blurred and almost unnoticeable, while later stages are manifested by significant pain and obvious external changes.
Deforming arthrosis of the 1st metatarsophalangeal joint is characterized by:
- severe fatigue and tiredness in the legs;
- stiffness of fingers while walking;
- discomfort in the sock when putting on shoes;
- sharp or aching pain in the foot area, especially after exercise;
- increased sensitivity of fingers to changes in weather conditions;
- subcutaneous nodules on the outside of the metatarsophalangeal joint;
- feeling of cold, numbness, tingling, aching in the leg;
- stiffness and crunching in the joint;
- hyperemia and swelling around the thumb bone;
- unnatural bend of the finger towards the little finger;
- noticeable deformation of the foot.
To avoid irreversible degenerative changes, it is important to pay attention to any suspicious discomfort. If you have at least one, even minor, symptom, you should immediately undergo examination by a specialist.
The second stage of metatarsophalangeal arthrosis in the majority of patients already causes complaints: pain when walking, swelling of the feet, discomfort when standing.
Stages of the disease
In general, the following stages are distinguished during arthrosis of the metatarsophalangeal joints:
- Stage 1 - symptoms of degenerative-dystrophic changes in the metatarsophalangeal joints occur no more often than once every few weeks or even months. At this time, patients may notice slight discomfort, tingling and a feeling of stiffness in the joints when resting on the toes or when rolling on them from the heel. All unpleasant sensations pass quickly and are therefore not perceived by patients as a serious disorder.
- Stage 2 - the progression of pathological changes in the metatarsophalangeal joints leads to the periodic appearance of pain, as well as a crunching sound during movements. At this stage, you can already notice a slight deformation of the affected joints, as well as signs of arthritis (redness, swelling, pain in the area of the affected metatarsophalangeal joint).
- Stage 3 – pain is constantly present, including at rest. At this stage of development of the disease, curvature of the finger is observed, the metatarsophalangeal joint of which is affected. Typically this is the big toe. As a result of its deviation towards neighboring fingers, a callus or lump begins to form in the area of its metatarsophalangeal joint. It may periodically become red, swollen and painful. But besides this, the curvature of the big toe and the formation of the so-called bunion on the foot leads to significant difficulties when choosing shoes.
- Stage 4 – the affected joint is severely deformed, and corresponding changes occur in the adjacent fingers. This is accompanied by severe pain and difficulty moving. At this stage, the only way to save the situation and return the patient to the ability to walk normally is through surgery.
Physiotherapy
A mandatory measure for arthrosis of the thumb is therapeutic exercises. Special exercises help return the joint to its correct shape, reduce discomfort, and tone the muscles. Indicated at the initial stage of the disease and after surgery.
A set of simple and effective exercises can be performed at home or even at work:
- lay out various small objects on the floor (pens, spools of thread, balls, toys), try to pick them up with your toes, hold them and put them back, and also bring them to your palm;
- while lying on your back, raise your foot and use it to write the letters of the alphabet in order in the air;
- perform the “Bicycle” exercise, use your foot as much as possible, focusing on rotating the pedals with your fingertips;
- walk around the apartment first on your toes, then on the inside and outside of your feet, finishing the exercise on your heels;
- sitting on the floor with your hands behind your back, pull your socks away from you and return them in the opposite direction;
- from a sitting position, try to move each toe individually, controlling the muscles and joints;
- massage each finger with your hands, slightly pulling the thumb to the side.
Remember, gymnastics should not cause severe pain and discomfort. Exercises should be regular and only those recommended by the doctor.
This treatment method is highly effective in the early stages of pathology development.
Diagnostics
If signs of arthrosis of the metatarsophalangeal joints occur, patients should consult an orthopedist. The doctor will conduct a survey, during which he will find out the nature of the patient’s complaints and lifestyle, and then proceed to the examination. At the same time, he always pays attention not only to the condition of the joints themselves, especially the big toe, but also to the condition of the skin. Already on the basis of these data, an orthopedist can diagnose the presence of arthrosis of the metatarsophalangeal joints.
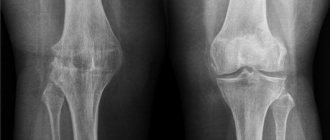
But to accurately determine the degree of degenerative-dystrophic changes, the presence of an inflammatory process and other changes, the following must be prescribed:
- UAC and OAM;
- x-ray of feet in two projections;
- Ultrasound of the metatarsophalangeal joints;
- CT and MRI (prescribed in complex cases when other methods cannot determine the specific course of pathological changes).
Diagnostic methods
A diagnosis of osteoarthritis of the metatarsophalangeal joint of the toe can be made based on existing symptoms. However, for confirmation it is necessary to undergo a comprehensive examination. Initially, the doctor examines the patient visually and by palpation. Next he sends him for x-rays. If necessary, computed tomography or magnetic resonance imaging and ultrasound examination are prescribed. These techniques allow you to accurately determine the degree of damage, the presence of concomitant diseases, and the stage of development of arthrosis.
Treatment of arthrosis of the metatarsophalangeal joints
For each patient diagnosed with arthrosis of the metatarsophalangeal joints, treatment is selected individually in accordance with the degree of pathological changes. Initially, all patients, with the exception of advanced cases of degenerative-dystrophic changes in the joints, are prescribed conservative treatment. But the disease can be completely cured only if it is detected at the initial stages of development. In the future, conservative methods can only stop the further progression of pathological changes in the joints, but not reverse them.
For arthrosis of the metatarsophalangeal joints of grade 3 and 4, surgical intervention is indicated. This is the only way to get rid of pain and other symptoms of the disease that reduce the patient’s physical capabilities.
Conservative treatment for arthrosis of the metatarsophalangeal joints is always complex. It includes:
- drug therapy;
- physiotherapy;
- exercise therapy;
- massotherapy.
In addition, the orthopedist can give individual recommendations for patients. Thus, he will recommend that people who are overweight take measures to reduce it. To achieve this goal, you will need to make adjustments to your diet and increase your level of physical activity. But any single-component and other unbalanced diets are contraindicated. It is extremely important that the body receives all the substances necessary for the proper functioning of the joints. Therefore, the daily diet should contain the required amount of proteins, fats, carbohydrates, vitamins, etc.
If you have flat feet, hallux valgus or other foot deformities, your orthopedist will prescribe the use of orthopedic insoles. But they must be made individually. It may also be recommended to use special fixing bands and splints.
If arthrosis of the metatarsophalangeal joints is detected at an early stage of development and promptly begins to use orthopedic devices (custom insoles, bandages), it will be possible to avoid valgus deformity of the toe and maintain an aesthetically attractive appearance of the foot.
It is also important to avoid wearing tight, uncomfortable shoes and high heels. Patients with this diagnosis are only suitable for comfortable shoes with wide toes and wide heels of low height.
Drug therapy
For arthrosis of the metatarsophalangeal joints, a complex of medications is prescribed that are aimed at relieving pain and stopping the progression of degenerative processes in cartilage tissue. For each patient, a set of drugs is selected individually, taking into account the severity of arthrosis, existing concomitant diseases and a number of other factors. As a rule, they are prescribed:
- NSAIDs are non-steroidal anti-inflammatory drugs that help not only eliminate inflammatory processes, but also help reduce pain. Depending on the characteristics of the disease, the doctor may prescribe ointments, creams, tablets and drugs in other dosage forms.
- Chondroprotectors are a group of drugs that include glucosamine and chondroitin as active ingredients. These compounds are natural to the body and are used by it to regenerate cartilage tissue. The course of treatment with drugs of this group is long (3-6 months). Chondroprotectors can be prescribed in the form of capsules and powders, but injectable forms are most effective.
- Corticosteroids are hormonal drugs that have a pronounced anti-inflammatory effect. They are indicated for severe inflammatory processes and severe pain that cannot be eliminated by taking NSAIDs. Corticosteroids are often prescribed by injection because this route of administration causes fewer side effects.
- Vitamin complexes are prescribed to improve the course of metabolic processes, normalize the functioning of the immune system and provide the body with the substances it needs for proper functioning.
Sometimes patients are given intra-articular injections of synovial fluid substitutes. They help reduce friction between joint components and activate regeneration processes, which will lead to a reduction in pain.
When arthritis occurs, patients are additionally prescribed drug treatment aimed at eliminating the inflammatory process. Antibiotics and other medications can be used for this purpose.
Physiotherapy
Physiotherapeutic procedures are indicated outside of the acute inflammatory process. They are most effective when used for arthrosis of the metatarsophalangeal joints of degrees 1 and 2. In most cases, patients are shown courses consisting of 10-15 procedures:
- UHF;
- magnetic therapy;
- laser therapy;
- electrophoresis;
- phonophoresis.
Thanks to physiotherapy, it is possible to reduce the severity of pain and eliminate swelling. In addition, it helps to improve metabolic processes and activate blood circulation in the foot, which has a positive effect on the condition of the joints. Also, certain physiotherapeutic effects can increase the tone of the muscles and ligaments of the foot, which is very important in the presence of flat feet and other orthopedic disorders.
Exercise therapy
One of the mandatory components of conservative treatment of arthrosis of the metatarsophalangeal joints is exercise therapy or physical therapy. It helps improve muscle tone, strengthen the natural arches of the foot and improve joint mobility. For each patient, the training program and exercises are selected individually, taking into account not only the nature of pathological changes in the metatarsophalangeal joints, but also the level of physical development, the presence of foot deformities, etc.
Initially, it is recommended to engage in special exercise therapy groups under the guidance of a physical therapy instructor. This will allow you to master the technique of performing each exercise as accurately as possible, which will ensure that you get the best effect. Gradually, the exercises can become more complicated, the number of repetitions increased, etc. But all this is carried out only as prescribed by the attending physician or exercise therapy instructor. In the future, you can do therapeutic exercises at home.
The main condition for the effectiveness of exercise therapy is a systematic approach. Therefore, it is necessary to perform the set of exercises recommended by your doctor every day.
Massotherapy
Massage therapy sessions help increase the effectiveness of drug therapy and other measures taken. With their help, it is possible to increase blood circulation in the affected joints and muscle tone. They also help increase joint mobility and restore normal foot anatomy.
Surgery for arthrosis of the metatarsophalangeal joints
In case of arthrosis of the metatarsophalangeal joints of the 3rd and especially 4th degree, as well as in the case of rapid progression of the pathology, severe pain and limitations of mobility against the background of ineffectiveness of conservative treatment, surgical intervention is indicated. Modern surgery can offer the following options for operations for arthrosis of the metatarsophalangeal joints:
- Cheilectomy – removal of osteophytes, i.e. bone growths on the articular surfaces of bones. This allows you to improve the function of flexion and extension of the metatarsophalangeal joints and, accordingly, the toes.
- Arthrodesis is an operation, the essence of which is the fusion of articular surfaces with each other and, therefore, complete immobilization of the joint. Therefore, it is performed mainly in the most difficult cases, when other methods cannot solve the problem of arthrosis. But arthrodesis provides reliable pain relief. Thus, during the operation, the surgeon places the metatarsal bone and proximal phalanx of the finger in the correct position and fixes them with special correctors.
- Endoprosthesis replacement is a high-tech operation performed for arthrosis of the 1st metatarsophalangeal joint of 3-4 degrees. It consists of replacing a worn-out joint with an artificial prosthesis, which completely preserves the functionality of the joint and eliminates the symptoms of the disease. Endoprosthesis replacement involves resection of a fragment of the base of the main phalanx of the big toe and the head of the first metatarsal bone. The legs of the endoprosthesis are mounted inside the bones, after which the artificial joint is repositioned and the wound is sutured layer-by-layer.
When choosing the first two methods, provided that valgus deformity of the finger develops and a protruding bone is formed, Schede's operation is additionally performed. Its essence is to remove the callus formed at the base of the joint affected by arthrosis. Therefore, it is aimed at removing the consequences of the disease, but does not directly affect it. But Shede's operation ensures a good cosmetic defect.
Thus, arthrosis of the metatarsophalangeal joints is an extremely unpleasant disease, which, if left untreated, can provoke a number of undesirable changes in the condition of the feet. But today it can be cured at any stage of development.
Classification of foot diseases and types of arthrosis
There are dozens of small joints in the foot. The problem can start in any of them. In modern medicine, there are different types of arthrosis of the foot, which are distinguished by its location. The disease can develop in:
- subtalar ligament;
- cuboid-calcaneal joint;
- metatarsophalangeal joint;
- arthrosis of the toe.
Arthrosis of the foot is also divided by degree. There are the following types:
- Primary.
May occur due to pathology in the foot or after injury or damage;
- Secondary.
Arthrosis of the foot of this degree appears due to diseases that affect the lower extremities. This could be hormonal disorders or any other;
- Polyarthrosis.
This is a complex degree of arthrosis of the foot. The disease affects not one, but several or more joints at once.
Treatment is prescribed depending on what type of arthrosis affects the foot.
Rehabilitation
Rehabilitation after conservative treatment If the doctor recommends conservative treatment, then if all recommendations are followed, improvement may occur within a few days. As a rule, anti-inflammatory drugs are prescribed, such as indomethacin, diclofenac, ibuprofen. Sometimes an intra-articular injection of corticosteroids is recommended. It is necessary to choose special shoes. In order for the effect of the treatment to appear, it is necessary to unload the foot for up to several weeks.
Rehabilitation after surgical treatment Rehabilitation after surgical treatment takes at least eight weeks. Most likely, in the early postoperative period, a plaster splint and crutches are needed to eliminate the load on the leg. Dressings are carried out as prescribed by the doctor. The sutures are removed after 10–14 days.
During almost the entire rehabilitation period, it is necessary to wear special shoes or a plaster splint (depending on the operation). A consultation with a physiotherapist is required to prescribe a course of physiotherapy. The physical therapy doctor will develop a course of exercises to maintain muscle tone in the postoperative period.
Preventive measures
Simple prevention can delay arthrosis of the 1st metatarsophalangeal joint and possible complications as much as possible, including:
- wearing loose, comfortable, soft shoes with low heels;
- control body weight, preventing severe obesity;
- active lifestyle with moderate physical activity (hiking, cycling, dancing, fitness);
- quitting smoking, drinking alcohol and junk food;
- timely treatment of acute inflammatory diseases, injuries of the lower extremities;
- regular examinations by a specialized doctor if you are prone to joint pathologies.
Preventive measures can prevent an unpleasant disease if you maintain a healthy lifestyle. And proper treatment of existing arthrosis allows you to stop the destruction of the joint and maintain its mobility for a long time.
Folk remedies for arthrosis
An integrated approach to the treatment of arthrosis of the metatarsophalangeal joint involves the use of traditional medicine methods. Natural and safe medications help relieve the condition without causing adverse reactions.
The following procedures have a pronounced analgesic and warming effect:
- Bath of salt and soda. 3 tbsp. Dissolve tablespoons of a mixture of table salt and soda in warm water. Pour the liquid into a basin and immerse your foot in it so that the water covers the foot. Do foot baths for 20 minutes every day before bed.
- Rub from honey and mumiyo. Mix liquid natural honey (100 g) with a teaspoon of mumiyo. Slowly rub your fingers with the resulting ointment, cover with a clean cloth and leave overnight.
- Horseradish compress. Grate fresh horseradish root and pour boiling water over it for a couple of minutes. Place the mixture squeezed out of the water onto a bandage and wrap it around the sore finger, covering it with film. Leave it on for a couple of hours and remove it.
- Cabbage leaf applique. Wash a fresh leaf of white cabbage and prick it a little with a fork to release the juice. Coat one side with a thin layer of honey and place on the foot. Wrap it loosely with a bandage and leave it for several hours.
Home treatment is effective as an addition to primary therapy. On its own, it is not able to cure the pathology, but only alleviate the symptoms.