Bruised toes are one of the most common injuries encountered by trauma surgeons. You can get damaged both during professional activities and at home. Most often, a bruised toe occurs due to carelessness when the patient accidentally touches foreign objects. In this case, acute pain immediately appears, and after a while - redness and swelling of the tissues. A traumatologist treats a bruised toe. This is the doctor you should contact as soon as possible after an injury.
You can make an appointment with a traumatologist in Yaroslavl at the CONSTANTA Clinic. The specialist will examine the injured limb, make a preliminary diagnosis and, if necessary, prescribe additional diagnostic methods. Bruised toes are not as harmless as is commonly believed. Often, after receiving an injury, patients try to deal with pain and swelling on their own for several days, unaware of the presence of an ordinary or marginal fracture of a finger and other serious injuries that can easily be obtained even at home.
Features of the structure of the toes
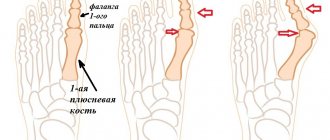
The toes are based on tubular bones. Each finger is formed by three phalanges, except the thumb, which has only two. Thanks to the movable joints and tendons, the fingers can perform various movements and help a person maintain balance while walking. Even minor damage to the soft and hard tissues of the foot leads to movement restrictions and knocks a person out of the usual rhythm of life.
During a bruise, tissue damage and microtrauma of blood vessels occur. This leads to an increase in edema and the development of an inflammatory reaction. Even a minor injury requires appropriate treatment for a bruised toe. Otherwise, swelling and pain will increase, limiting the patient's physical activity. Often, bruised toes are accompanied by blue discoloration and peeling of the nail plate. In this case, it may require partial or complete removal.
Diagnostics
If your toe is swollen, you should consult a surgeon. If such a symptom occurs due to injury, it is better to choose a traumatologist. If joints are affected, you need a rheumatologist or arthrologist. If necessary, the doctor will refer you to another specialist.
Diagnosis begins with listening to complaints, examining and palpating the affected area. They often resort to x-rays - such a study can reveal injury and various changes in bone tissue. Computed tomography may also be used.
If an inflammatory process is suspected, laboratory diagnostics are prescribed - general urine and blood tests. A puncture of intra-articular fluid followed by its examination may be required.
Signs of a bruised or broken toe
The symptoms of a bruise and a broken toe are similar: the patient feels pain that does not allow him to step on the foot, and also notices swelling of the soft tissues. Only a qualified specialist can distinguish a fracture or crack from a bruise. An accurate diagnosis is made based on X-ray data and professional examination.
A patient who has suffered a bruised toe should be alert to the following signs:
- pathological mobility of the toes at the site of injury;
- prolonged pain syndrome, which is poorly relieved by classical analgesics;
- increasing swelling and cyanosis of the skin;
- crunching sound (crepitus) when pressing on the injury site;
- unnatural position of the foot or toes.
If such symptoms appear, it is necessary to make an appointment with a traumatologist and conduct an X-ray examination to make sure that there is no fracture of the toe. Do not self-medicate under any circumstances, even if you are sure that the injury you received is harmless. Our Clinic also employs pediatric traumatologists, and you can show your child to a specialist at any time or seek medical help from an experienced doctor yourself.
With a marginal fracture of the big toe, which often occurs while running, the swelling spreads to the entire foot, and the skin becomes noticeably blue. The patient experiences severe pain and cannot step on his leg; he often takes a forced position, which allows him to spare the limb as much as possible. Signs of a big toe fracture can be supplemented by pathological mobility and the presence of crepitus.
How to prevent the disease
Basic preventive measures help prevent swelling in the toes. You just need to take care of your body and try to avoid the possibility of injury. The key to good foot health will be personal hygiene, which should be present in every person's life on an ongoing basis.
Particular attention should be paid to the choice of comfortable, high-quality shoes, which should be made from natural materials, and also have a not very high heel and a comfortable sole. In addition, you can use special orthopedic shoes or insoles. If fungal or other diseases are detected, treatment should be started immediately.
You should also monitor your diet so that it is complete and includes all the necessary microelements obtained from foods. It is necessary to reduce the amount of salt consumed, as it prevents excess water from leaving the body, which causes edema. It is also better to abstain from drinking alcohol or reduce it to a minimum.
Swelling of the fingers is easy to treat and is often completely eliminated, but only if treatment was provided in a timely manner. By following basic rules, you can prevent the formation of edema and also maintain your health.
Fractured toe: types
A toe fracture can be an open fracture, where soft tissue damage occurs and bone fragments may protrude from the wound. In this situation, there is a direct threat of secondary infection. The patient urgently needs antiseptic treatment. For open fractures of the toes, treatment should not be delayed.
With closed fractures of the fingers, the integrity of the skin is not broken, and displacement of the fragments is usually not observed. But this type of fracture does not exclude the development of infectious and other complications. A closed fracture of the toe is often complicated by a purulent infection, especially when the nail bed is damaged and the nail plate peels off, which becomes an entry point for infectious pathogens.
When a displaced fracture occurs, comparison of bone fragments is required, which will give the finger an anatomically correct shape and restore the impaired functions of the limb.
What to do if you notice signs of gout
If you notice the first signs, you should consult a doctor as soon as possible. He will order an x-ray and ask for basic tests. If the diagnosis is confirmed, treatment begins without delay. The doctor will also give recommendations on changing your diet, choosing it in such a way as not to provoke an excessive accumulation of uric acid salts and help improve metabolic processes in the body.
Treating signs of gout
At the Paramita clinic, each patient is approached individually, taking into account all the features of his health in his prescriptions. After the first session, the pain will subside, and further effects will not be long in coming. Doctors select a comprehensive treatment for gout, which includes the following methods of Eastern therapy:
- Hirudotherapy – improves blood circulation, stimulates nutrition of tissues and joints, removes toxins and wastes
- Pharmacopuncture – helps to establish metabolic processes, helps the kidneys remove salts, strengthens the overall effect of treatment
- Stone therapy – has a relaxing effect and relieves stress
- Herbal medicine – has a healing and anti-inflammatory effect
- Acupuncture – affects biologically active points of the body, relieving pain and eliminating swelling of the affected joint.
Themes
Joints, Gout Date of publication: 10/22/2014 Date of update: 11/27/2019
Reader rating
Rating: 5 / 5 (1)
Complications of toe injuries
Broken toes can lead to dangerous health consequences even when the injury is relatively mild. Without qualified medical care, skin wounds, cracks and bone fractures can provoke the development of the following complications:
- massive hematomas;
- ankylosis (joint immobility);
- deformation of finger joints;
- formation of bone callus;
- sepsis;
- secondary infections.
Damage to the soft and hard tissues of the extremities is especially dangerous for patients who suffer from metabolic disorders and chronic diseases, in particular diabetes. For such patients, even a minor injury can pose a hidden threat.
Arthritis
If the foot is swollen and you can’t even put on your shoes properly, and your legs burn and hurt, then this may be a manifestation of arthritis. The inflammatory process in foot arthritis begins around the joints, but can spread to soft tissues, causing widespread inflammation. If you identify the symptoms of arthritis at an early stage and find out why the inflammation appeared, then the disease is much easier to cure.
The following symptoms are observed with arthritis of the toe:
- the appearance of pain in the limbs, which worsens at night and torments patients with insomnia;
- redness of the skin of the foot;
- stiffness in the legs;
- local hyperthermia;
- deterioration of general health;
- the occurrence of heavy leg syndrome.
Some patients note that their finger turns blue due to arthritis, while others note constant redness and swelling of the finger.
With the development of arthritis in patients, the pathology can be complicated by osteoarthritis - in this case, the inflammatory process affects not only the joint, but also the bone. During this process, the cartilage tissue is actively destroyed, pits appear on its surface, the cartilage becomes thinner and the bone surface is visible. During the process of aggressive destruction, the articular surfaces try to protect themselves and osteophytes appear. If arthritis is caused by a buildup of uric acid in the toe joints, it causes gout.
If arthritis is caused by autoimmune causes, systemic rheumatoid arthritis develops. This disease affects not only the toes, but also the hands and other small and large joints.
How to treat bruises and broken toes
Patients with bruises and broken toes require first aid. It is very important to contact a traumatologist in a timely manner and undergo the prescribed examination. This will allow the doctor to select effective treatment for bruised toes as soon as possible and take all necessary measures to prevent complications.
Medical tactics for bruises and fractures of fingers are selected depending on the nature of the injury. With an open fracture, the wound can quickly become infected and fester, and the risk of developing tetanus cannot be ruled out. Experts practice the administration of anti-tetanus serum and antibacterial treatment of open wounds of the toes, especially if they are caused by contact with the ground and working tools.
Immobilization is indicated for almost all toe injuries. It allows you to relieve the sore foot and speed up the patient’s recovery process. Treatment of a fractured finger with bone displacement requires special professionalism when it is necessary to restore the anatomical shape of the phalanx. In this case, the correct fusion of bone tissue in the future depends on the professionalism of the traumatologist.
Even a minor finger injury is accompanied by pain and signs of an inflammatory reaction. To relieve pain, specialists prescribe analgesics in the form of local agents, tablets or injections. Drugs are selected taking into account the severity of the patient's condition.
Local agents with anti-inflammatory, regenerating and analgesic properties are recommended for long-term use. They alleviate the patient’s condition, have an antiseptic effect and promote rapid resorption of hematomas.
Morton's neuroma
Morton's disease is a disorder of the plantar nerve sheath in which it thickens. The pathology causes pain, especially if patients wear narrow shoes. Usually the neuroma affects the second or middle fingers, rarely the first and fourth. Neoplasms of the nerve are quite common - these pathologies are dealt with by traumatologists or neurologists. Fortunately, neuroma does not degenerate into cancer.
Doctors see the cause of the appearance of a neuroma near the toe in excessive stress on the forefoot. Neuroma is usually provoked by walking in high heels, excess body weight, and even improper gait. Morton's disease often accompanies athletes involved in professional sports with heavy load on the foot; their feet hurt, and neuroma appears quite often.
REFERENCE! Among the diseases that precede neuroma are flat feet, microtraumas, bursitis or tendovaginitis, and atherosclerosis.
Typical signs of Morton's neuroma are pain in the third and fourth toes with shooting. The fingers may become swollen, accompanied by a sensation of a foreign body. As the disease progresses, the pain worsens and becomes constant, accompanied by paresthesia of the fingers.
If the leg is swollen and there is a suspicion of a neuroma, the diagnosis can only be made using magnetic resonance imaging; CT and x-rays will be uninformative. The best diagnostic method is ultrasound - it is cheaper and gives excellent diagnostic results.
When treating the disease conservatively, it is recommended to change the insoles in your shoes and spare your feet. Patients are recommended to take non-steroidal anti-inflammatory drugs; injections of anesthetics will help relieve pain. If the finger is swollen, NSAIDs are applied topically in the form of ointments or compresses. Physiotherapeutic measures are actively included in the treatment regimen. If conservative therapy does not bring results, surgical treatment is used to dissect the intermetatarsal ligament.
Other Lymphedema Treatments
There are other treatments for lymphedema. Talk to your doctor or lymphedema therapist about which ones are right for you.
Other treatments for lymphedema include:
- Treatment of scars. Scarring from surgery can make it difficult for your body to eliminate fluid. Scar treatments help soften the area around the scar and make it less tight. It will help drain fluid from your legs.
- Improved posture.
- Using kinesiology tape for athletes.
to come back to the beginning
About lymphedema
Lymphedema is a swelling condition that can develop in the legs after lymph nodes are removed or injured. Lymph nodes are small, bean-shaped structures that are located throughout the body. They drain fluid away from different areas of your body. The inability to drain fluid leads to tissue swelling.
During surgery, lymph nodes in your pelvis were removed to get rid of any remaining cancer cells. This increases the risk of developing leg lymphedema. The risk will be higher if you have had radiation therapy or had lymph nodes removed in your groin. If you only have lymph nodes in your pelvis removed, you may be less likely to develop leg lymphedema.
Lymphedema may develop immediately after surgery or years later.
to come back to the beginning
How to recognize the first signs of lymphedema
After surgery, swelling occurs at the incision site (surgical suture) in all patients. This is normal and will subside a few weeks after surgery.
Swelling caused by lymphedema usually occurs in the lower leg(s). If left untreated, it can spread throughout the leg and all the way to the torso. At first, this swelling may appear and disappear. It may decrease as you lift your leg higher than your chest.
Other early symptoms may include a feeling of heaviness in your leg(s) or a feeling that clothes, socks or shoes are pressing in on you.
to come back to the beginning
Stages of the disease
The initial stage of the disease is called serous-infiltrative. 2-3 days after the onset of the lesion, it passes into the purulent-necrotic stage.
The serous-infiltrative stage is characterized by:
- moderate pain;
- exacerbation of unpleasant sensations when the hand is lowered down;
- redness on the back of the hand;
- swelling of fingers and hands;
- the affected finger is difficult to bend;
- body temperature fluctuates between 37-37.5 degrees;
- satisfactory health.
When the disease enters the purulent-necrotic stage, the symptoms are pronounced:
- throbbing or jerking pain in the affected finger;
- the patient is forced to keep the hand raised upward;
- paler spots are visible in the center of the reddened areas of the skin;
- the veins of the hand are dilated;
- fever, general intoxication;
- The blood test shows a high ESR and an increased number of leukocytes.
Which doctor should I contact?
To prescribe truly effective treatment, you need to answer the question of why your toes swell. To do this, you should visit an experienced doctor.
Typically, the initial consultation is with a primary care physician. He conducts an initial examination, interviews the patient, but for the most part still cannot make an accurate diagnosis. Instead, the doctor refers the patient to a consultation with another experienced specialist.
This could be a surgeon, neurologist, podologist, traumatologist, endocrinologist, etc.
Only after a specialist examines the patient and draws up a conclusion can a diagnosis be made and treatment prescribed. In most cases, the disease is treated without complications in a short time. Problems may arise if the patient has an individual intolerance to a certain type of medication.
Folk remedies
If the healthcare system cannot cope with the patient’s problem on its own, folk remedies are used.
The use of diuretics is considered effective. At the same time, both store-bought preparations and those made at home from natural ingredients are used equally successfully. Mix carrot, cucumber and beet juice and drink. It is recommended to use equal proportions.
Parsley is a means to improve the functioning of the heart and kidneys. If symptoms in the legs are associated with poor functioning of these internal organs, the use of parsley is completely justified. The recipe has been passed down from generation to generation and has proven itself well.
Finally, cabbage leaves serve as an effective treatment for illness. It is enough to wash them and apply them to the place where these symptoms are most severe. Never pre-dry cabbage leaves. The juice of the plant should interact with the diseased area of the skin.
The mechanism of operation of the traditional medicine described above has not been studied. This means that the patient acts at his own peril and risk. A positive effect may occur, but nothing like this may happen.
To ensure a guaranteed cure for a dangerous disease, it is necessary to visit a specialist doctor.
How does panaritium occur?
To start the pathological process, a tiny wound on the finger is enough - for example, from an injection or splinter.
Small wounds heal quickly, but the infection remains inside and continues to multiply. In this case, the human body recognizes the danger and begins to produce phagocytes (leukocytes). The structure of the connective tissue of the hands is specific - it forms vertical fascial partitions. They go from the periosteum to the skin, dividing into vertical cells. This keeps the infection from spreading to other areas, but creates ideal conditions for an abscess to form.
When swelling occurs in such partitions and pressure in the tissues increases, debilitating pain appears. If panaritium is not treated, the infection breaks into neighboring cells, spreading to the joints and tendons.
Risk factors for developing leg lymphedema
Risk factors for developing leg lymphedema include:
- weight gain or excess weight;
- infection of the affected leg;
- radiotherapy of the pelvic area;
- reappearance of cancer.
There are other factors that are thought to increase this risk. These include:
- Sedentary lifestyle.
- Flying on an airplane.
- Compression of the leg. It occurs when there is a tight ring of pressure in one area of the leg and is often caused by wearing certain clothing.
- Exposure to extreme temperatures.
to come back to the beginning
Prevention
It is not difficult to prevent the appearance of panaritium. To do this, it is important to follow the following rules:
- wear protective gloves when working;
- observe safety precautions at work and at home;
- immediately treat any skin damage with antiseptics, including splinter injections and hangnails;
- cover injured areas with a protective plaster.
- ensure that manicure tools are sterile;
- Avoid prolonged exposure to water - it weakens the protective qualities of the skin.