Causes
The tibial nerve is a continuation of the sciatic nerve. Its damage is possible in the following cases:
- Injuries of the lower extremities of various etiologies (fracture, dislocation or sprain of the ankle, tendon rupture, sprained foot ligaments). Traumatic factors and swelling caused by them lead to direct damage or compression of the tibial nerve, which leads to disruption of the transmission of nerve impulses.
- Deformation changes in the foot (flat feet, valgus).
- Compression of the feet or their uncomfortable position for a long time, for example, when squeezing the lower limbs with a heavy object.
- Diseases of the knee joint and ankle (arthritis, arthrosis).
- Disorders in the functioning of the endocrine system, thyroid diseases, diabetes mellitus.
- Tumor lesions of the tibial nerve of benign and malignant nature.
- Impaired blood flow to the legs and feet of the lower extremities (vasculitis).
- Poisoning of the body with toxic and chemical compounds, including alcohol-containing products.
- Inflammatory pathologies of infectious etiology of various localizations, including damage to multiple nerve fibers.
- Long-term therapy with drugs that negatively affect the functioning of the central nervous system.
- Reduced protective properties of the body.
- Harmful working conditions.
- Impaired nutrition of the tissues of the lower leg and foot.
- Prolonged exposure to low temperatures on the lower extremities.
- Improper nutrition, resulting in a decrease in the intake of B vitamins in the body.
- Pathological processes affecting the spinal column.
People at risk include:
- professionally involved in various sports;
- with working conditions that require constant standing, including walking;
- those who are prone to overweight or obesity - a large load on the lower limbs increases the risk of dysfunction of the tibial nerve;
- choosing the wrong shoes: high heels, thin soles.
Causes of shin pain
Traumatic injuries
A shin bruise usually occurs after a blow, less often it results from a fall.
It manifests itself as short-term severe acute pain, which quickly subsides, becomes dull, aching, weak or moderate. Swelling is detected in the area of the bruise, and bruising is possible. Support is preserved, movements are somewhat limited due to pain. Sometimes there is lameness. According to the mechanism of occurrence and clinical manifestations, a hematoma resembles a bruise, but the pain is of a pressing, bursting nature, which is caused by the accumulation of blood in the soft tissues. The difference from a bruise is a dense, limited swelling or area of fluctuation that does not disappear for a long time. Bruising is usually found on the skin.
Damage to the Achilles tendon is manifested by sharp pain, reminiscent of a blow or cut, on the back of the lower leg just above the ankle joint. Upon examination, swelling, pain on palpation, and retraction at the site of the Achilles are revealed. Plantar flexion of the foot is impossible with a complete rupture, but with a partial rupture it is limited. Support is significantly difficult.
Fractures of the lower leg bones are the result of a high-energy impact: a fall from a height, being hit by a car bumper, or an industrial accident. They manifest as explosive pain, which subsequently decreases somewhat, but remains very intense. At the time of injury, a crunching sound may be heard. The following types of damage are possible:
- Fracture of the tibia.
Develops as a result of impact, twisting, falling. Usually associated with a fracture of the fibula. Accompanied by unbearable pain, displacement of fragments, significant swelling, deformation of the limb, widespread bruising, crepitus, and pathological mobility. Support is impossible, movements are sharply painful. - Isolated fracture of the fibula.
Formed by direct impact. Local swelling and bruising at the site of injury are detected. The pain is moderate, sharply intensifies with palpation of the fracture zone. When the fracture line is located in an area not covered by muscles, a step is detected. The supporting function of the limb suffers slightly.
With a pathological fracture, the clinical manifestations are smoothed out, the pain syndrome is moderate. Bone fragments are often pressed into each other, so there is no crepitus or pathological mobility. Signs that allow one to suspect a violation of the integrity of the bone are the prolonged persistence of symptoms, previous disease of the bone structures, and periodic pain in the area of this segment of the limb.
Inflammatory diseases
Myositis of the lower leg muscles develops against the background of previous overloads: intense training, long walks. It manifests itself as aching pain that spreads throughout a muscle or group of muscles. The pain increases with tension and palpation of the muscle. Sometimes a slight diffuse thickening of muscle tissue, mild swelling, and hyperemia are detected.
Pain in the back of the leg above the ankle joint is caused by inflammation of the Achilles tendon. With tendinitis, the zone of maximum pain is located 3-6 cm above the Achilles insertion point, with peritendinitis it spreads throughout the tendon. At first, the pain syndrome appears only in the first minutes of exercise, then the pain intensifies, becomes prolonged, increases rather than decreases with continued movements, and occurs at rest, at night.
The tibia is often affected by osteitis deformans. The pain is deep, localized in the area of the affected bone, dull, aching, constant, and persists for many months. Intensifies at rest, after rest. They may be accompanied by curvature of the limb, pathological fractures, and when the lesion is located near the joint, the development of osteoarthritis is noted.
Shin pain
Bone infections
Aseptic periostitis usually develops along the anterior surface of the tibia, in an area with little soft tissue volume. It occurs after a bruise and is characterized by moderate pain, aggravated by palpation of the bone, and slight swelling. Sometimes serous inflammation is observed with the formation of a significant amount of fluid, manifested by bursting pain and the formation of a “bump” in the affected area.
Purulent periostitis becomes a consequence of infectious diseases of soft tissues and is formed in the projection of the inflammatory focus or in the area of swelling. The pain is rapidly increasing, twitching, pulsating, sharply intensifying when palpated. They appear against a background of increased temperature, chills, weakness, fatigue, and significant swelling of the limb. Within a few days they become unbearable and deprive you of night sleep.
Hematogenous osteomyelitis often affects the tibia. It develops in children, in half of the cases – after minor trauma or a general infectious disease. Manifests with severe hyperthermia, chills, fever, against which a pain syndrome appears after a few hours or 1-2 days. The pain is deep, extremely intense, pulsating, tearing. The slightest movement causes an explosion of pain, so patients try to lie still.
In some cases, a favorable course of hematogenous osteomyelitis is observed with a predominance of local symptoms and moderate pain. A hurricane development of the disease with delirium and severe impairment of general condition is also possible. In the case of postoperative and post-traumatic osteomyelitis, a clinical picture similar to the hematogenous type of the disease is observed, but the symptoms are not so pronounced, and the progression of the pathology is longer.
Soft tissue infections
In case of infectious lesions of soft tissues, the pain in the first hours is pressing, and when touched it is stabbing. They grow quickly, become twitching, pulsating, constant, and exhausting. They intensify when palpating, lowering the limb. The formation of an abscess usually occurs against the background of a sleepless night. In the affected area, swelling, hyperemia, purple-bluish coloration of the skin, and local hyperthermia are detected.
The degree of disturbance of the general condition depends on the prevalence of the purulent process, ranging from minor malaise to severe fever, severe intoxication syndrome. Local pain in the lower leg is observed with boils. Intense pain syndrome, spreading over a significant part of the segment, is observed with carbuncles, abscesses and phlegmon.
Arterial diseases
The cause of pain in the lower leg is sometimes arterial disease. With obliterating endarteritis, pain initially appears only when walking long distances (over 1 km). The pain is localized in the calf muscles, provokes intermittent claudication, and forces the patient to stop while moving. In the future, the distance to the onset of pain is reduced. In the later stages, pain is observed at rest, trophic ulcers form, and gangrene develops.
In terms of the nature and conditions of the onset of pain, obliterating atherosclerosis resembles obliterating endarteritis, but is detected in older men rather than in young men, and has a more favorable course. Only 14% experience rapid development of pathology, leading to pain at rest and severe trophic disorders; in other cases, pain remains at the same level for a long time or intensifies during periods of seasonal exacerbations. Similar symptoms are observed with Mönckeberg arteriosclerosis, which is diagnosed in the second half of life and occurs equally often in both sexes.
Diseases of veins and lymphatic vessels
A common vascular cause of pain is varicose veins. At first, the pain is minor, dull, local, short-term, appears in the evening, after a long stay in an upright position, and is combined with a feeling of heaviness. Subsequently, the pain syndrome becomes long-lasting, occurs after minor exertion, and is accompanied by noticeable pastiness of the limbs. At the final stage, the pain is prolonged, supplemented by night cramps, swelling, hyperpigmentation, and trophic disorders.
Acute phlebitis of the superficial veins of the leg often develops with varicose veins and is manifested by rapidly progressing pain, the appearance of a strip of hyperemia along the vein. The vein is compacted, its palpation is painful. With chronic phlebitis, the symptoms are smoothed out, the pain is recurrent. When deep veins are affected, there is no red stripe on the skin, the pain is localized deep in the tissues, combined with severe swelling and general hyperthermia.
With thrombophlebitis, as a rule, varicose veins of the upper third of the segment are affected. There is a nagging sharp pain in the projection of the vein, which intensifies when walking, the formation of a red stripe, a dense painful cord, and a disturbance in the general condition. With deep vein thrombosis, the pain is deep, bursting, aggravated by palpation, and can be combined with swelling, pallor of the limb, and swelling of the superficial veins.
With lymphedema, pain in the legs is constant, dull, bursting, complemented by heaviness in the legs and significant dense swelling of the limb. Primary lymphedema is characterized by a gradual spread of pain and swelling in the peripheral direction (from the thigh to the lower leg), while secondary lymphedema occurs in the central direction (from the foot to the lower leg). Palpation of the limb segment is painless.
Other skeletal diseases
In Schlatter's disease, local tenderness occurs in the area of the tibial tuberosity, just below the knee joint. The pain syndrome is associated with physical activity, appears when squatting, walking up stairs, and disappears with rest. At first the pain is mild, then it becomes significant, and attacks of acute cutting pain are possible. Palpation is painful; a prominence of bone density is detected in the area of the tuberosity.
Pain in the legs can occur with congenital anomalies of the lower extremities, Blount's disease, X-shaped legs, gonarthrosis and arthrosis of the ankle joint. Usually dull, aching, intermittent, associated with physical activity. Caused by disruption of the normal mechanisms of standing and walking, constant overload of the limb.
Oncological pathologies
Benign tumors of the tibia are characterized by slow growth, low-intensity, intermittent pain with unclear localization. The exceptions are osteoid osteoma and osteoblastoma, in which the pain is sharp, acute, and intense. Chondromas most often form on the tibia. Osteochondromas usually affect the fibula, the pain syndrome is localized in the upper third of the leg along the outer surface.
With malignant neoplasia, the pain is initially unclear and dull. They progress quickly, become permanent, extremely intense, painful. They can only be eliminated with narcotic analgesics. There is a deterioration in the general condition, swelling, deformation, and dilation of veins in the area of the neoplasm. With osteogenic sarcomas, pain occurs closer to the knee or ankle joint, with chondrosarcomas - in the upper part of the leg.
Neurological causes
Sometimes painful sensations are provoked by neurological pathologies. The pain is burning, shooting, piercing, spreading throughout the segment or the entire leg, combined with sensitivity disorders, weakening of the strength of the limb. The cause of pain is:
- Radicular syndrome.
Occurs after spinal injuries, in many degenerative diseases. The affected area depends on the root involved. Pain in the leg is combined with pain in the back, which is provoked by sudden movements, laughing, coughing, sneezing. - Femoral nerve neuropathy.
The pain is localized along the anterior inner surface of the lower leg and intensifies with extension of the knee joint. - Peroneal nerve neuropathy.
Pain occurs in the outer part of the lower leg (mainly in the lower third of the segment), and intensifies with squats. - Tibial nerve neuropathy.
With pathology of traumatic origin, patients complain of burning causal pain along the back, partially outer surfaces of the leg. With tarsal tunnel syndrome, there is pain in the foot, radiating to the calf muscle. - Sciatic nerve neuropathy.
The pain spreads along the buttock to the back of the thigh and lower leg to the foot. Very sharp, reminiscent of a lumbago, a dagger strike.
Symptoms
Neuropathy is accompanied by a clinical picture of severity, which depends on the degree of damage to the nerve fibers.
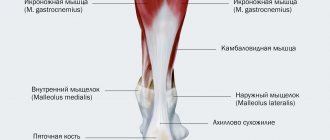
Nerve dysfunction can be recognized by impaired flexion of the foot and motor ability of the fingers. When walking, the foot is placed incorrectly - the emphasis is on the heel. The muscular system of the lower leg and foot shows signs of obvious atrophy and deformation.
In the case of traumatic origin of neuropathy, swelling forms in the ankle area, blood flow is disrupted, tissue sensitivity increases, and there is severe pain, which intensifies when the damaged areas are touched.
If the cause of nerve neuropathy is endocrine disorders or infectious lesions, the patient loses sensation in the lower extremity area of the leg and foot. The pain syndrome persists and can have a different nature and severity. The pain intensifies with walking and physical activity. The patient may experience involuntary contractions of individual muscles or a convulsive syndrome involving the lower limbs.
In addition, the patient is concerned about neurotrophic disorders, such as dryness of the epidermis in the lower legs and feet, keratinization of the upper layer of the dermis, brittle nails, pallor of the skin and a decrease in local temperature, increased sweating.
Symptoms of tibial nerve neuropathy
If the disease involves the popliteal region, the patient has problems with flexion of the foot, as well as an inability to control the fingers normally. There is an inability to stand on your toes. Complete dysfunction of the muscles in the area of the lower leg and foot occurs, the latter taking the form of a clawed paw.
In some cases, the problem begins to bother you as a result of long walking or jogging. There is severe pain in the sole, radiating to the calf muscle. Severe pain increases significantly in a standing position, as well as while walking.
The medial plantar nerve is mostly affected by elite runners. Pain occurs on the inside of the sole, as well as in the area of two or three toes.
Women who regularly wear heels or are obese suffer from this disease. Moreover, any movement or running significantly increases the pain.
Calcanodynia affects the heel area. As a rule, this disease occurs as a result of an unsuccessful jump on the heels, walking for a long time with bare feet, or using shoes with thin soles. A person cannot step on his heels due to burning and unbearable sensations.
Diagnostics
Tibial nerve neuropathy belongs to the group of mononeuropathy of the extremities. The clinical picture of the pathology is characteristic of dysfunctions of the musculoskeletal system and is of a traumatic nature, and therefore is subject to joint observation and control by specialists in the field of neurology and traumatology.
The first step in making a diagnosis is to question the patient about injuries to the lower extremities, working conditions, as well as the characteristics of the clinical picture and the presence of other diseases that may affect the normal functioning of the nervous system. After this, the patient is examined to identify atrophic and neurotrophic changes in the lower leg and foot.
Based on the data obtained, an initial diagnosis is made, which is confirmed by instrumental studies using one of the following methods:
- ultrasound diagnostics of the lower extremities;
- electromyography is a research method that allows you to determine the performance of the muscular system of the lower leg and foot;
- X-ray diagnostics if indicated, for example, for fractures;
- trigger point blockade is a therapeutic and prophylactic method that involves administering a medication to the affected areas of the lower extremities, which makes it possible to determine the degree of nerve damage;
- CT and MRI are used as additional diagnostic methods when using other methods there is insufficient data to make a diagnosis.
Therapy
The initial stage in treatment is therapy of the pathology that is the root cause of nerve fiber dysfunction. For example, for endocrine disorders of the system, hormonal drugs are prescribed, for diabetes mellitus, medications are prescribed to normalize blood sugar levels. If there is a deficiency of B vitamins, intravenous administration of drugs with vitamins B1, B6 and B12 is indicated, which will improve the nutritional capacity of the tissues of the nervous system.
To reduce the severity of pain and resume motor activity, the patient is prescribed special orthopedic shoes or insoles. The choice is made in accordance with the localization of the damage to the nerve fibers.
In case of severe pain, severe swelling as a result of pinched nerve endings, blockades are carried out with the introduction of analgesics (Analgin, Novocaine) and anti-inflammatory non-steroidal drugs (Ibuprofen, Dicroberyl). Less commonly used are steroids (hydrocortisone) or antidepressants (amitriptyline).
For trophic disorders of surface tissues, reperants (Solcoseryl, Actovegin) are recommended, the action of which is aimed at renewing cellular structures.
Anticholinesterase medications (Ipidacrine) are used to suppress nervous excitability.
To restore performance and strengthen the muscular system of the ankle, normalize blood flow, physiotherapeutic methods of therapy (electrophoresis, magnetic therapy, shock wave therapy), exercise therapy and massage sessions are indicated.
Surgical intervention is necessary in the absence of effectiveness of conservative therapy, nerve damage, the formation of adhesions, impaired sensitivity of the lower extremities and severe pain. The operation is performed by a neurosurgeon.