Hip dysplasia in newborns (infants)
Hip dysplasia is a congenital defect of the joint that can lead to joint damage. Dysplasia in newborns is the direct cause of congenital hip dislocation. This pathology, in turn, can lead to changes in gait, chronic pain syndrome and significantly limit mobility in the future.
The newborn itself (a newborn is a child in the first 28 days of life) is not bothered by dysplasia; Parents and doctors identify the disease based on external symptoms, and not on the basis of the baby’s crying or restlessness. If the pathology is not treated on time, it leads to deformation of the musculoskeletal system, disruption of the formation of the musculoskeletal system and disability. The disease can affect one leg (usually) or both. Boys suffer from hip dysplasia 7 times less often than girls.
What it is?
Today, hip dysplasia is considered the most common pathology of the musculoskeletal system in newborns and infants. “Dysplasia” translated means “improper growth,” in this case of one or both hip joints.
The development of the disease is associated with disruption of the formation of the main joint structures in the prenatal period:
- ligamentous apparatus;
- bone structures and cartilage;
- muscles;
- change in the innervation of the joint.
Most often, hip dysplasia in newborns and the treatment of this pathology is associated with a change in the location of the femoral head in relation to the bony pelvic ring. Therefore, in medicine this disease is called congenital hip dislocation.
Treatment must begin from the moment the pathology is diagnosed, the earlier the better, and before the baby begins to walk - from this moment irreversible complications appear. They are associated with an increasing load on the joint and the exit of the bone head completely from the acetabulum with an upward or sideways displacement.
The child develops changes when walking: a “duck” gait, significant shortening of the limb, compensatory curvature of the spine. These disorders can only be corrected through surgery. With pronounced changes in the joint, the baby may remain disabled for life.
Sources
- Yen W., Gartenberg A., Cho W. Pelvic obliquity associated with neuromuscular scoliosis in cerebral palsy: cause and treatment. // Spine Deform - 2021 - Vol - NNULL - p.; PMID:33861427
- Fatima M., Asghar MS., Abbas S., Iltaf S., Ali A. An Observational Study to Evaluate the Effectiveness of Rivaroxaban in the Management of Cerebral Venous Sinus Thrombosis. // Cureus - 2021 - Vol13 - N3 - p.e13663; PMID:33824814
- Gu M., Liu CC., Hsu CC., Lu CJ., Lee TS., Chen M., Ho CC. Associations of sleep duration with physical fitness performance and self-perception of health: a cross-sectional study of Taiwanese adults aged 23-45. // BMC Public Health - 2021 - Vol21 - N1 - p.594; PMID:33765974
- Weidekamm C., Teh J. . // Radiologe - 2021 - Vol61 - N4 - p.395-404; PMID:33765171
- Yousef MA., Ayers DC. Challenging Diagnosis of Stickler Syndrome in a Patient with Premature Osteoarthritis: A Case Report. // JBJS Case Connect - 2021 - Vol11 - N1 - p.; PMID:33755637
- Rozis M., Vlamis J., Pneumaticos S.G. Chronic Undiagnosed Brucellosis Presenting as Sciatica. // Cureus - 2021 - Vol13 - N2 - p.e13114; PMID:33728133
- Butscheidt S., Tsourdi E., Rolvien T., Delsmann A., Stürznickel J., Barvencik F., Jakob F., Hofbauer LC., Mundlos S., Kornak U., Seefried L., Oheim R. Relevant genetic variants are common in women with pregnancy and lactation-associated osteoporosis (PLO) and predispose to more severe clinical manifestations. // Bone - 2021 - Vol147 - NNULL - p.115911; PMID:33716164
Statistics
Hip dysplasia is common in all countries (2 - 3%), but there are racial and ethnic characteristics of its distribution. For example, the incidence of congenital underdevelopment of the hip joints in newborn children in Scandinavian countries reaches 4%, in Germany - 2%, in the USA it is higher among the white population than African Americans, and is 1 - 2%, among American Indians, hip dislocation occurs in 25- 50 per 1000, while congenital hip dislocation almost never occurs among South American Indians, southern Chinese and Africans.
A connection between morbidity and environmental problems has been noted. The incidence in the Russian Federation is approximately 2 - 3%, and in environmentally unfavorable regions up to 12%. Statistics on dysplasia are contradictory. Thus, in Ukraine (2004), congenital dysplasia, subluxation and dislocation of the hip occur in 50 to 200 cases per 1000 (5 - 20%) newborns, that is, significantly (5-10 times) higher than in the same territory during the Soviet period.
A direct connection has been noted between the increased incidence and the tradition of tightly swaddling the baby's straightened legs. Among peoples living in the tropics, newborns are not swaddled, their freedom of movement is not limited, they are carried on their backs (while the child’s legs are in a state of flexion and abduction), the incidence is lower. For example, in Japan, as part of a national project in 1975, the national tradition of tightly swaddling the straightened legs of infants was changed. The training program was aimed at grandmothers to prevent traditional swaddling of babies. As a result, there was a decrease in congenital hip dislocation from 1.1-3.5 to 0.2%.
This pathology occurs more often in girls (80% of identified cases); family cases of the disease make up about a third. Hip dysplasia is 10 times more common in children whose parents had signs of congenital hip dislocation. Congenital dislocation of the hip is detected 10 times more often in those born with a breech presentation of the fetus, more often during the first birth. Dysplasia is often detected during drug correction of pregnancy, or during pregnancy complicated by toxicosis. Most often the left hip joint is affected (60%), less often the right (20%) or both (20%).
Until the first half of the last century, only the severe form of dysplasia, congenital hip dislocation (3-4 cases per 1000 births) was taken into account. In those years, “mild forms” of dysplasia were not detected or treated. From the 70s - 90s. The term “hip dysplasia” is used, meaning not only dislocation, but also preluxation and subluxation of the hip joint. The incidence numbers have increased tenfold.
It should be noted that the lack of clear standards and the fear of missing severe orthopedic pathology is the reason for overdiagnosis (20-30% at the pre-dislocation stage). The dilemma of “immature hip joint and preluxation” is usually resolved in favor of dysplasia, which increases morbidity figures.
Classification
There are several types of hip dysplasia:
- Femoral dysplasia . The mechanism of development of TB dysplasia is a violation of the neck-diaphyseal angle, which determines the centralization of the femoral head in the acetabulum (the angle of articulation of the femoral neck with its body). Both a decrease in the angle of the hip joint - coxa vara, and an increase in it - coxa valga can be observed (Fig. below).
- Acetabular dysplasia . The pathology is caused by a violation of the development of the acetabulum, which is reduced in size, flatter, with an underdeveloped cartilaginous rim.
- Rotational dysplasia . The movement of all joints of the lower limb is caused by a mismatch of axes (excessive antetorsion angle of the femur), that is, a violation of the location of the femoral head relative to the acetabulum.
According to clinical and radiological criteria preluxation (unstable hip), subluxation (primary, residual and hip dislocation (anterolateral/lateral), supraacetabular and iliac high dislocation .
Causes of dysplasia
Underdevelopment and improper formation of the hip joint occur when the intrauterine development of a child is disrupted due to disturbances in the formation, development and differentiation of the baby’s musculoskeletal system (from 4-5 weeks of intrauterine development until the formation of full walking).
Reasons that negatively affect the fetus and disrupt organogenesis:
- gene mutations, as a result of which orthopedic deviations develop with disturbances of the primary anlage and the formation of defects in the hip joints of the embryo;
- exposure to negative physical and chemical agents directly on the fetus (ionizing radiation, pesticides, use of medications);
- a large fetus or breech presentation, causing displacement in the joints due to a violation of the anatomical norms of the location of the child in the uterus;
- disturbance of water-salt metabolism in the fetus due to kidney pathology and intrauterine infections.
Factors that negatively affect the development of the fetus and cause the formation of dysplasia on the mother’s side are:
- severe somatic diseases during pregnancy - cardiac dysfunction and vascular pathology, severe kidney and liver diseases, heart defects;
- vitamin deficiency, anemia;
- violation of metabolic processes;
- severe infectious and viral diseases suffered during pregnancy;
- unhealthy lifestyle, unhealthy diet and bad habits (smoking, drug addiction, drinking alcohol);
- early or late toxicosis.
In the risk group for the development of this pathology, contributing to the early diagnosis of dysplasia in infants. At the same time, even in the maternity hospital, the neonatologist and pediatrician at the site observe the baby more actively.
This group primarily includes premature babies, large children, with a breech presentation of the fetus, a pathological pregnancy and with a family history. It should be noted that this pathology occurs more often in girls than in boys.
Also, in addition to true dysplasia, infants (impaired development of the joint) may exhibit immaturity of the joint (slow development), which is considered a borderline state for the development of dislocation of the hip joint.
Treatment using the Nikonov method on muscles
Doctor Nikonov
Quote : My method of restoring mobility of the hip joint is based on restoring muscle mobility to its physiological norm. Using the Nikonov method on muscles with fixation of the problem muscle, I restore normal muscle stretching. With this effect, the hyaline layer completely covers the head of the femur at the hip joint. My method of treating dysplasia is the only effective one, since I know the real reason for the development of the disease.
Symptoms of dysplasia
When examining a baby, pay attention to the following signs (see photo):
- position and size of the lower extremities;
- position of skin folds in the thigh area (symmetrical or asymmetrical);
- muscle tone;
- volume of active and passive movements.
Hip dysplasia in infants manifests itself with characteristic symptoms.
- Limitation of hip abduction. Childhood hip dysplasia is manifested by limited abduction to 80 degrees or less. The symptom is most typical for unilateral lesions.
- Slipping symptom (synonym: clicking symptom). The child is placed on his back, bending his legs at both the knee and hip joints at an angle of 90 degrees (the examiner’s thumbs are placed on the inner surface of the thighs, the remaining fingers are on the outer surface). When the hips are abducted, pressure is applied to the greater trochanter, resulting in the reduction of the femoral head. The process is accompanied by a characteristic click.
- External rotation of the lower extremity is a sign characterized by outward rotation of the hip on the affected side. It can also occur in healthy children.
- Relative shortening of the limb. The symptom is rare in newborns and is observed with high dislocations.
- The asymmetrical position of the femoral and gluteal folds is revealed during an external examination.
Secondary (auxiliary) signs of hip dysplasia in a newborn:
- atrophy of soft tissues (muscles) on the affected side;
- pulsation of the femoral artery is reduced on the side of the dysplastic joint.
Asymptomatic cases of congenital hip dislocation are rare.
Patella tilting and subluxation, femoral condyle dysplasia
Usually this bone is called the kneecap, but in medicine they use another term - the patella.
The patella is a small but very important bone. It is located in front of the knee joint. In fact, the patella is the sesamoid bone. In medicine, this is the name for the bones that are located inside the tendons. Humans have several sesamoid bones, and the patella is the largest of them. The sesamoid bones, and the patella in particular, are needed to increase the efficiency of muscle traction and increase its strength, since these bones work like a block.
The patella (kneecap) is located in the thickness of the tendon that extends the tibia. This tendon is formed by the fusion of four muscles on the front of the thigh - the so-called quadriceps muscle. Below the patella begins the patellar ligament, which is attached to the front of the tibia (to the tibial tuberosity). Sometimes the patellar ligament is called the patellar ligament. When the leg is extended, the patella “floats” above the knee joint, located in front and above the joint space, but when the knee is bent, the patella fits into a special notch (groove) between the two condyles of the femur and begins to work like a block. This place in the knee joint is also called the patellofemoral joint (or patellofemoral joint, from the Latin terms patella - patella and femur - thigh).
The inside of the patella is covered with a thick layer of cartilage, which is needed to slide along the cartilage of the femoral condyles. The patellar cartilage is the thickest cartilage in humans - its thickness can exceed 5 millimeters! Naturally, it is thick for a reason, but because the patella experiences very strong loads. You can learn more about the anatomy of the knee joint and the patella in particular on our website.
On the left – the knee is in a flexed position. The patella fits into a groove on the femur, causing it to act as a pulley, increasing the traction efficiency of the quadriceps tendon.
In order for the patella to work as a block during extension in the knee joint to be as effective as possible, it must fit into the groove between the condyles of the femur correctly, i.e. centered. If the patella lies in the groove incorrectly, not in the center, then they talk about the inclination of the patella.
On the left - the patella is centered. The width of the inner and outer parts of the femoral-patellar joint is the same. On the right, the patella is displaced outward. The inside of the joint is much wider than the outside.
Almost always, when there are problems in the patellofemoral joint, the patella moves outward, and only in very rare cases does the patella move inward. If the tilt is slight, then we speak of lateral hyperprepression (i.e., increased pressure of the patella on the lateral condyle of the femur), or medial hyperpression if the patella is displaced medially. With greater displacement of the patella, subluxation appears, and finally, if the patella completely extends beyond the groove between the condyles of the femur, then they speak of a dislocated patella.
From left to right: normal joint (the width of the inner and outer parts of the joint is the same), patellar tilt or lateral hyperpression (the outer gap is narrower than the inner), subluxation of the patella (part of the patella has moved out beyond the condyle) and dislocation (the patella has completely moved outside the joint)
Tilt and subluxation of the patella are one of the variants of its instability, i.e. conditions where the patella may subluxate or completely dislocate.
Causes
Tilt and subluxation can be caused by various factors, most often several at the same time. Among the main reasons are the following:
- Excessive tension in the external patellar suspensory ligament or weakness in the internal patellar suspensory ligament (may develop due to a rupture of this ligament);
- weakness of the vastus medialis (internal) muscle;
- abnormal shape of the legs: X-shaped or valgus curvature of the legs (deviation of the legs outward);
- dysplasia of the femoral condyles;
- hyperextension in the knee joint;
- high position of the patella - patella alta;
- the outer position of the tibial tuberosity - the place to which the patellar ligament is attached
- internal rotation of the lower leg (can be a congenital feature - when a person rakes his feet inward when walking or can develop as a result of flat feet).
- other rare causes (femoral anteversion, patellar dysplasia, etc.)
The patella has two ligaments that hold it on the sides (sometimes they are not called ligaments, but retinaculum). The external ligament pulls the patella outward and does not allow it to dislocate inward, and the internal ligament, on the contrary, pulls the patella inward and does not allow it to dislocate outward. Excessive tension in the external patellar suspensory ligament or weakness in the internal patellar suspensory ligament (which can develop as a result of a rupture of this ligament) can cause the patella to lie in the groove between the femoral condyles not centered, but with a large displacement outward.
Normally, the patellar ligament (external and internal) is balanced and the patella is centered. If this balance is disturbed, for example, when the internal ligament is torn, the patella will tend to move outward due to uncompensated traction of the external ligament.
The stability of the patella is ensured not only by ligaments, but also by muscles. In particular, the vastus medialis (internal) muscle pulls the patella inward. This muscle is part of the quadriceps femoris muscle, which consists of four heads. If the vastus internus muscle is weak, it will not fully stabilize the patella and it will move outward.
Thigh muscles, front view. The quadriceps femoris consists of four muscles (heads): 1 - Rectus femoris, 2 - Vastus lateralis, 3 - Vastus medialis, 4 - Vastus intermedius. The vastus medialis (internal) muscle keeps the patella from moving outward (its pull is marked with black translucent arrows)
X-shaped or valgus curvature of the legs (deviation of the legs outward). If you look at the skeleton from the front, you can see how the femur connects to the shin at an angle called the quadriceps angle or Q-angle. The size of the angle Q is determined by the width of the pelvis. Women have a wider pelvis than men, so the Q-angle is larger in women than in men. In addition, congenital X-shaped deformity of the legs can lead to an increase in the Q-angle. A large Q angle causes the patella to move outward more easily. In addition, with a large Q-angle, the anterior cruciate ligament ruptures more easily.
Q-angle. The normal value is 20° for women and 15° for men. An abnormal Q-angle does not necessarily cause anterior knee pain or patellar subluxation, but it does contribute to patellar subluxation when the quadriceps muscle contracts.
Dysplasia of the femoral condyles. The groove between the femoral condyles must be deep enough to support the patella. With dysplasia of the condyles of the femur, i.e. a congenital feature of bone development, the groove is less deep and the patella moves outward more easily. Scientific studies have shown that in people with femoral condyle dysplasia, the groove depth is on average 7 millimeters less. There are several variants of dysplasia: dysplasia of both condyles, isolated dysplasia of the external or internal condyles, in addition, dysplasia can be of varying intensity. Dysplasia can be determined by axial radiographs or magnetic resonance imaging (MRI), and the accuracy of these two methods in determining dysplasia is approximately the same, but MRI, unlike radiographs, allows you to evaluate not only bones, but also soft tissues (cartilage, ligaments, etc.). d.).
Magnetic resonance imaging (MRI) of the knee joint. These images show a section of the knee joint at the level where the patella fits into the groove between the femoral condyles. On the left is a normal groove, on the right is a groove with condylar dysplasia. Please note that with dysplasia, the groove is less deep and the patella will move outward more easily. M - internal (medial) condyle, L - external (lateral) condyle
Hyperextension in the knee joint and high position of the patella (patella alta) lead to the fact that the patella will also slip out of the groove between the condyles and shift outward. When hyperextended, the patella is pushed out of the groove, and with a congenital high position of the patella, it lies in the groove higher, where the groove is smoothed out and is not so deep as to support the patella.
The outer position of the tibial tuberosity is the place where the patellar ligament is attached. In some people, the tibial tuberosity is located laterally (i.e., displaced outward), in which case the patella will also tend to move outward.
A similar problem occurs with internal rotation of the tibia - i.e. when the shin is twisted inward too much. This situation can occur due to a congenital feature - when a person rakes his feet inward when walking, or can develop as a result of flat feet.
Inward rotation (torsion) of the tibia promotes outward displacement of the patella
Symptoms of patellar tilt/subluxation
A typical manifestation of improper sliding of the patella in the intercondylar groove is pain in the anterior part of the knee joint and a feeling of instability. Sometimes patients with patellar tilt can accurately tell that the pain is located exactly under the patella (kneecap), but in many cases the pain is diffuse and affects the entire front surface of the knee. And finally, in the third case, the pain affects the entire knee joint.
A feeling of instability is an optional but common sign of patellar tilting/subluxation.
Often, in addition to pain, when bending and straightening the knee joint, a painful click or crunch may occur under the patella. These painful clicks and crunches in the knee joint under the kneecap occur due to improper sliding of the patella in the intercondylar groove.
When the leg is flexed, the patella usually slides along the intercondylar groove of the femur, but when it is almost fully extended, it moves outward. At this moment, patients usually feel a “failure” in the joint, although true dislocation of the patella rarely occurs in them.
Patellar tilting/subluxation is often preceded by trauma that damages the structure that prevents the patella from moving outward. For example, chronic patellar subluxation often develops after patellar luxation. In addition, patellar tilt/subluxation may develop as a complication after some knee surgeries.
Since when the patella tilts/subluxates, it slides in the intercondylar groove incorrectly, with greater pressure outward (more often, in rare cases, there is increased pressure from the inside—internal hyperpression), then with a long-term tilt/subluxation, the cartilage covering the patella and condyles, and patelofemoral arthrosis develops, which is part of the arthrosis of the knee joint.
With long-term tilting/subluxation of the patella, fluid may accumulate in the joint (synovitis), which will be manifested by swelling of the knee joint mainly above the patella.
In addition, when the patella dislocates, an injury to the patellar cartilage (osteochondral fracture) may occur, which will also contribute to the development of arthrosis of the knee joint.
Medical examination
As we have already noted, the most common complaint with tilting and subluxation of the patella is pain . During the examination, the doctor will first ask you about what movements this pain occurs with and where it is located. As a rule, pain appears when the knee joint is bent more than 30 degrees - because before this the patella does not come into contact with the intercondylar groove. The pain usually worsens when the quadriceps muscle is tense, such as when going up or down stairs.
During the examination, the doctor pays attention to the uneven development of the extensor muscles of the knee joint. When the patella is tilted and subluxated, atrophy and weakness of the vastus medialis muscle can often be seen.
In addition, during the examination, the doctor pays attention to all other factors that contribute to the development of patellar tilt/subluxation: posture and gait, high standing of the patella, abnormally large Q-angle, X-shaped curvature of the legs, femoral anteversion, dysplasia of the patella or femur, flat feet and joint hypermobility.
An approximate assessment of the trajectory of the patella can be made by slowly straightening the knee joint of a seated patient. Normally, the patella should move in a straight line. In some cases, you may notice a J sign, a pattern of motion that resembles an inverted J as the patella moves outward as the joint extends. With internal subluxation of the patella, a reverse J-sign can be seen due to the displacement of the patella in a position of full medial extension. If the J sign is noticeable when the legs hang freely while extending, this may indicate weakness of the vastus medialis muscle, which determines treatment tactics.
The path of movement of the patella when the knee is extended from point A to point B. When the patella is tilted/subluxated, it does not go in a straight line, and bends outward as the knee extends, which looks like an inverted letter J, which is why this symptom is called the J-sign
To determine the inclination and subluxation of the patella, the doctor conducts special tests: when pressing on the patella, when trying to move the patella outward with your fingers, pain may intensify and/or fear may appear, a premonition of patellar dislocation. In addition, increased patellar mobility revealed by this test will also indicate lateral tilt/patellar subluxation.
The lateral suspensory ligaments of the patella are also carefully examined. The pain of these ligaments upon palpation often accompanies their overload in patients with patellar subluxation. Tenderness in the area of the medial epicondyle - the so-called Bassett's sign - is characteristic of an injury to the medial femoral-patellar ligament.
The test to detect excess traction on the lateral suspensory ligament is to measure the inclination of the patella. The test is carried out with the knee joint relaxed and passively extended. When it is noticed that the outer edge of the patella has risen, the inner edge is fixed. Normally, the angle between the horizontal plane and the outer edge of the patella should be about 15°. At lower values, the cause of pain in the anterior knee joint may be excessive tension in the lateral suspensory ligament; according to indications, mobilization of the outer edge is carried out. When the patella is displaced outward, the patient sometimes tries to reduce the range of motion to avoid pain. This symptom most likely indicates hypermobility or instability of the patella.
The displacement of the patella along the articular surface from side to side makes it possible to judge the integrity of the structures that limit its mobility. Outward displacement is prevented by the external part of the joint capsule, the external suspensory ligament and the oblique part of the vastus medialis muscle. The patella is moved outward by hand and the resulting displacement relative to the neutral position is measured in quarters of the width of the patella. A shift of more than three quarters indicates hypermobility; less than one quarter with medial displacement indicates excessive tension of the medial suspensory ligament. The described test can provide valuable information about the condition of the ligamentous apparatus, but it is relatively subjective.
Palpation of the patella: the doctor presses on the patella and tries to move it to the sides, assessing the range of mobility and intensity of pain. The picture shows the Basset test
Fear, premonition of patellar dislocation. When the patella is displaced outward by the doctor's fingers, the patient may feel fear of dislocation and increased pain. Notice how the patient tries to stop the doctor. Illustration Hughston JC, Walsh WM, Puddu G: Patellar subluxation and dislocation. In: Saunders monographs in clinical orthopedics, vol 5, Philadelphia, 1984, Saunders with changes from the authors travmaorto.ru
When performing most tests, the patient lies on his back, but you can also examine the knee joint with the patient in the prone position. In this case, the immobility of the pelvis and the inability to flex the hip make it possible to more accurately assess the flexibility of the joint structures during extension. In addition, anterior femoral anteversion and tibial rotation can be easily identified. A decrease in the amplitude of internal rotation can be an early sign of arthrosis of the hip joint, which sometimes causes knee pain.
To clarify the diagnosis, additional research methods are carried out, the most important of which are radiography, computed tomography (CT) and magnetic resonance imaging (MRI). The initial examination of the femoral-patellar joint includes x-rays in frontal and lateral projections in a standing position. An AP X-ray may reveal significant subluxation, fracture, or deformation of the patella. Before judging the presence of subluxation, you need to make sure that this is not a placement error. Lateral radiographs can also provide valuable information. First of all, it allows you to get an idea of the depth and relief of the intercondylar groove. Its center corresponds to the most posterior line, and the articular surfaces of the lateral and medial condyles can be distinguished separately. Using these points, the depth of the furrow is measured and dysplasia is detected. Using a lateral radiograph, you can determine whether the patella is high or low and the ratio of the length of the patellar ligament to the diagonal of the patella is calculated. Normally, this ratio is 0.8-1.0; Large values indicate a high position of the patella, smaller values indicate a low position.
Additional information about the position of the patella is provided by radiography in the axial projection when the knee joints are flexed at an angle of 20° (according to Laurin) and at an angle of 45° (according to Merchant). To reduce radiation exposure, it is usually sufficient to take an image in one of these projections. Axial radiographs are very useful for identifying patellar tilt and subluxation. These radiographs determine two angles: the external femoral-patellar angle and the congruence angle. The first is formed by lines drawn through the femoral condyles and along the lateral facet of the patella. Typically these lines radiate outwards; if they are parallel or diverge inward, then this most likely indicates a tilt of the patella. The congruence angle is used to identify patellar subluxation. To construct the congruence angle, first draw a bisector of the angle formed by the slopes of the femoral condyles, and then measure the angle between this bisector and a line drawn from the lowest point of the slope to the middle part of the edge of the patella. Normal congruence in the knee joint bent at an angle of 45° is 6 ± 11°. At this angle of flexion, the patella should be located in the center of the articular surface, and a change in the degree of congruence indicates its possible subluxation.
Positioning the patient for AC Merchant radiographs
X-ray in the axial projection according to Merchant - the tilt of the patella is visible, the width of the joint space is uneven - it is smaller on the outside than on the inside
Computed tomography (CT) allows one to determine tilt and subluxation somewhat more accurately than radiographs in the axial projection, which is due to the absence of projection distortions and the overlapping of shadows of anatomical structures on each other. In addition, CT scans can be obtained at any knee flexion level. This is especially important for identifying tilt and subluxation of the patella with the knee practically extended, when the patella is deprived of fixation from the side of the lateral femoral condyle.
As we have already noted, an important factor in the development of patellar tilt/subluxation is the position of the tibial tuberosity, to which the patellar ligament is attached. An accurate assessment of the spatial relationship of the tuberosity, patella, and intercondylar groove can again be made on computed tomography (CT) scans. The most important indicator on them will be the TT-TG index (from the English terms tibial tuberosity and trochlear groove). To do this, measure the distance between the tuberosity and the intercondylar groove of the femur by superimposing two sections in the axial projection one on top of the other. A distance greater than 15 mm indicates patellar subluxation with a specificity of 95% and sensitivity of 85%.
Computer tomogram. In this figure, two sections are superimposed on each other: at the level of the intercondylar groove and at the level of the tibial tuberosity. Thanks to this overlay, the distance between the tuberosity and the sulcus can be measured. Normally, it varies from 10 to 15 mm. In this image it is 21 mm, indicating patellar subluxation.
Magnetic resonance imaging (MRI) can be used to confirm findings from CT scans and radiographs, but is more suitable for diagnosing soft tissue conditions and assessing cartilage damage. The method has proven itself to detect injuries associated with patellar dislocation: avulsion of the medial femoropatellar ligament from the femur or, less commonly, from the medial facet of the patella; joint effusion; areas of increased signal intensity and damage to the vastus medialis oblique muscle; hematomas in the area of the lateral femoral condyle and the medial facet of the patella.
Since pain in the knee joint can often be due to other reasons not related to the position of the patella, MRI is used quite often.
Treatment
Conservative treatment. Treatment of patellar tilt/subluxation is mainly conservative, i.e. non-surgical. The basis of treatment is physical exercise. Quadriceps strength and endurance are best trained with static, low-range extension exercises with the knee flexed between 0 and 30 degrees (i.e., with minimal contact between the patella and femur). The exercises are aimed at restoring the balance of the extensor muscles, special attention should be paid to the oblique part of the vastus medialis muscle.
Exercises for patellar flexion/subluxation
For additional stabilization of the patella, special orthopedic bandages, orthoses, and bandages can be used, but it is necessary that the patient understands the need to wear them. Orthoses also improve the architecture of the lower extremity, especially in patients with a tendency to have an X-shaped curvature of the legs, which aggravates patellar instability.
Taping is very effective, which allows you to compensate for the outward displacement of the patella and relieve pain in the knee joint against the background of hyperpresia of the outer parts of the femoral-patellar joint.
Thoughtful conservative treatment is effective in most cases, but in some cases it is not successful and then surgical intervention is often necessary.
Surgery. As with other diseases of the patellofemoral joint, accompanied by pain in the anterior part of the knee joint, arthroscopy is first performed: a video camera is inserted into the joint through a one-centimeter long puncture and the knee is examined from the inside. During arthroscopy, not only the femoral-patellar joint, the condition of the patellar cartilage, the correct insertion of the patella into the intercondylar groove are assessed, but also all other structures of the knee joint are assessed: cruciate ligaments, menisci, cartilage, etc.
If there is no subluxation of the patella, but only a tilt of the patella with lateral hyperpression, then arthroscopic mobilization of the outer edge of the patella is performed. To do this, the entire external suspensory ligament and the oblique part of the vastus externus muscle are dissected.
Scheme of the operation of arthroscopic mobilization of the outer edge of the patella (lateral release)
We have described the simplest and most common operation used to treat patellar tilting and subluxation. But, as we have already noted, there are many different reasons for the development of tilt and subluxation of the patella. And for some reasons, one operation is performed, and for another, another. In this article, we will not describe the algorithm for choosing the appropriate operation depending on certain reasons that led to the incorrect position of the patella in the intercondylar groove, since in fact this algorithm is relevant for a more severe option - chronic instability of the patella, manifested by complete dislocations of the patella. Usually, when the patella is tilted/subluxated, arthroscopic mobilization of the lateral edge of the patella is sufficient, but in some “advanced” cases, operations are used from the arsenal of methods for treating chronic patellar instability, which are described in detail in a separate article on our website.
Forecast
The prognosis in most cases of patellar tilting or subluxation is favorable. With both the correct conservative and surgical treatment tactics, a full recovery and even a return to sports activities is possible after restoration of mobility, stability and strength. The intensity of exercise and training should be increased gradually. The rehabilitation course is selected in accordance with the operation performed. Rest is required while soft tissue and bone heal.
Severity of traffic accidents
- I degree – pre-dislocation. A developmental deviation in which the muscles and ligaments are not changed, the head is located inside the beveled cavity of the joint.
- II degree – subluxation. Only part of the femoral head is located inside the articulation cavity, as it moves upward. The ligaments are stretched and lose tension.
- III degree – dislocation. The head of the femur comes completely out of the socket and is located higher. The ligaments are tense and stretched, and the cartilaginous rim fits inside the joint.
Consequences and complications
Delayed diagnosis and lack/ineffective treatment can lead to a number of complications:
- Impaired functions of the hip joint.
- Shortening of the injured limb.
- Deformations of the glenoid cavity.
- Development of pelvic asymmetry and curvature of the spinal column.
- Formation of flexion-adduction contracture.
- Avascular post-reposition necrosis of the femoral head .
- Multiplanar deformations.
- Development of hip arthrosis / dysplastic coxarthrosis .
Diagnostics
In a baby, signs of hip dysplasia in the form of a dislocation can be diagnosed in the maternity hospital. The neonatologist should carefully examine the child for the presence of such abnormalities in certain pregnancy complications.
The risk group includes children who belong to the category of large children, children with deformed feet and those with heredity burdened by this characteristic. In addition, attention is paid to toxicosis of pregnancy in the mother and the gender of the child. Newborn girls are subject to mandatory examination.
Examination methods:
- Ultrasound diagnostics is an effective method for identifying abnormalities in the structure of joints in children in the first three months of life. Ultrasound can be performed multiple times and is acceptable when examining newborns. The specialist pays attention to the condition of the cartilage, bones, joints, and calculates the angle of the hip joint.
- Arthroscopy and arthrography are performed in severe, advanced cases of dysplasia. These invasive techniques require general anesthesia to obtain detailed information about the joint.
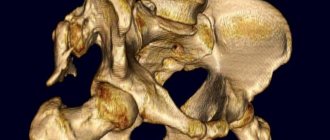
- CT and MRI provide a complete picture of pathological changes in the joints in various projections. The need for such an examination appears when planning surgical intervention.
- The X-ray image is not inferior in reliability to ultrasound diagnostics, but has a number of significant limitations. The hip joint in children under seven months of age is poorly visible due to the low level of ossification of these tissues. Radiation is not recommended for children in their first year of life. In addition, placing an active baby under the device while maintaining symmetry is problematic.
- External examination and palpation are carried out to identify characteristic symptoms of the disease. In infants, hip dysplasia has signs of both dislocation and subluxation, which are difficult to identify clinically. Any symptoms of abnormalities require a more detailed instrumental examination.
Main causes, symptoms and diagnosis of hip joint diseases
Pathological conditions in the hip most often develop against the background of:
- mechanical damage to joint elements;
- a tendency to diseases of the articular tissue of the hip area at the genetic level;
- functional impairment due to infection;
- systemic diseases in connective tissue;
- damage to the integrity of the joint due to degenerative-dystrophic transformations.
Any disease of the hip joint is characterized by the appearance of common symptoms:
- pain on the inner or outer thigh surface and in the groin area is of an acute, aching or pulling nature;
- motor activity is impaired, movements become limited;
- the skin becomes inflamed, the local temperature rises to subfebrile levels.
To correctly determine hip disease, a high-quality biochemical study is required. In addition, to accurately establish the diagnosis, instrumental diagnostic methods are shown:
- CT and MRI;
- Radiography;
- Ultrasound;
- Scintigraphy.
Let's consider the most common clinical diseases of the hip joint.
Hip dysplasia
This clinical disease is a congenital disorder or inferiority of the joint tissue, which increases the risk of subluxation or dislocation of the femoral head. The maximum number of cases of inadequate development of hip joints is observed in those areas where socio-economic policy is stable.
In the Scandinavian countries, the congenital anomaly is 4%, in Germany – 2%, and in the USA – 1-1.5%.
In the Russian Federation and post-Soviet countries, congenital dysplasia is diagnosed in 50-250 newborns out of 1000 (approximately 5%). According to medical experts, this is due to the unfavorable environmental situation in the states that were formerly part of the Soviet Union.
For the most part, the congenital disease is detected in female infants (in 80% of cases), as well as in families where one or both parents suffer from “congenital dysplasia.”
This congenital orthopedic anomaly can develop due to:
- breech presentation of the unborn baby;
- medical correction of pregnancy, which is complicated by toxicosis;
- large fruit.
A baby can develop dysplasia if he is swaddled too tightly to straighten his legs.
Since 1975, the Japanese have refused to tightly swaddle newborns. This has reduced the number of hip dislocations in infants.
Dysplasia in infants is manifested by the following clinical signs:
- asymmetrical skin folds on the legs;
- pronounced shortening of the thigh;
- restrictions in abduction and adduction of the hip joint.
A characteristic sign due to which one can suspect the presence of congenital dysplasia in a newborn is the Marx-Ortolani symptom. If you abduct the hip joint towards the surface where your baby is lying, you may hear a typical clicking sound in the joint area. This indicates that the femoral head is slipping into the acetabulum area.
The only effective therapy is to use a corrective orthopedic orthosis, thanks to which the baby’s legs can remain in a bent and abducted position at the required angle for a long time. Over time, the newborn is recommended to undergo massage, perform therapeutic exercises with constant supervision by an orthopedist. If treatment is started on time, the child can most often be cured.
Arthritis of the hip joint
Arthritis (coxitis) is a disease characterized by the development of an inflammatory process in the tissues of the hip joint. The disease occurs in acute (primary manifestations), protracted (2-12 months) or chronic form, which lasts more than a year.
Arthritic damage to the tissue system in the hip joint is divided into groups. It happens:
- infectious (septic coxitis) – inflammation that forms against the background of damage to the synovial fluid by an agent of a fungal, parasitic, infectious-allergic or viral nature;
- reactive arthritis - an immune-inflammatory pathology that manifests itself in the process or as a complication of infection of the joint tissue;
- rheumatoid arthritis is an autoimmune disease caused by the formation and spread of granulation tissue in the cavity of the synovial capsule. Because of this, articular cartilage and subchondral bone are destroyed;
- psoriatic arthritis is a rare autoimmune disease of the hip joint, manifested as a result of damage to joint tissue by psoriasis.
Symptoms, signs and treatment of hip coxitis
The causes, symptoms and therapeutic measures for arthritis of the hip joint depend on the nature of the disease.
The development of septic (infectious) arthritis is observed as a complication against the background of severe infection, which penetrates into the joint tissues through the bloodstream. This form of pathology is accompanied by joint pain, limitation of motor activity in the joint, redness and swelling in the problem area, hyperthermia within 39-40 degrees.
For therapeutic purposes, for infectious coxitis, anti-inflammatory drugs are prescribed for intramuscular, intravenous and intra-articular administration, as well as antiseptic and antipyretic drugs. In some cases, surgical treatment of the hip joints is required, which can be performed in Moscow in specialized centers. Failure to contact specialists in a timely manner is fraught with negative consequences; sometimes this disease causes the death of the patient.
The cause of reactive arthritis is an intestinal or urogenital infection. Pathology can also be caused by ureaplasma, streptococci and other microorganisms. This form of coxitis is characterized by the appearance of:
- pain in the hip joint;
- increased temperature;
- hyperemia and swelling of soft tissue in the damaged area;
- pain while walking or other activities.
Which medications will be prescribed for therapeutic purposes for reactive coxitis depends on the type of pathogen. The disease is easily treatable, the patient fully recovers after six months of drug therapy. In this case, the joint tissue is not destroyed.
The exact cause of the development of rheumatoid arthritis has not yet been determined. According to doctors, this is due to immunogenetic disorders in the body. This type of disease is accompanied by stiffness and pain in the joint in the morning, hyperthermia to low-grade levels (37-38 degrees). For rheumatoid arthritis, pharmacological agents of the antirheumatic, anti-inflammatory and hormonal group are indicated in the form of a course of treatment. It is not possible to completely cure coxitis of the rheumatoid form, but regular use of medications helps relieve the main pain syndromes of the pathology.
The psoriatic form of coxitis is a rather rare disease; it develops against the background of a skin pathology – psoriasis. With this disease, soft tissues become covered with dry red plaques, swelling forms, the temperature rises, and aches in the joints. Non-steroidal anti-inflammatory drugs are prescribed for therapeutic purposes. The outcome of the disease is determined by the severity of the condition.
Arthrosis (coxarthrosis)
Pain in the hip joint is often a sign of arthrosis of the hip joint. This is a chronic inflammatory disease, against the background of which dystrophic destruction is observed in the articular tissue of the hip joint.
Due to a lack of lubricating fluid, friction between the bones increases. This leads to the formation of growths on the head of the joint, which makes the functional activity of the joint tissue difficult.
If coxarthrosis of the hip joint is not treated in time, the patient will certainly lose the ability to move.
Consequences
If there is no treatment, then at an early age this can threaten the child with serious troubles. Children develop a limp when walking; it can be either barely noticeable or pronounced. Also, the baby will not be able to move his leg to the side, or will do it with great difficulty. The child will be bothered by constant pain in the knees and pelvis with possible bone distortion. Depending on the severity of the symptoms of dysplasia, children experience muscle atrophy of varying severity.
Gradually, as the child grows, the consequences of untreated dysplasia will worsen and be expressed in the development of the so-called “duck gait,” when the baby rolls from one leg to the other, protruding the pelvis back. The motor activity of such a child will be limited, which will entail underdevelopment not only of other joints, but will also affect the functioning of all organs and overall physical development. In the future, the leg muscles can completely atrophy, and the person will begin to be haunted by constant, incessant pain. In adult patients, hyperlordosis of the spine in the lumbar region is observed. All organs located in the pelvic area are also affected.
All this can be avoided if you start treatment on time and follow preventive measures.
Trochanteritis: signs, symptoms and treatment
In this disease, inflammation directly affects the hip part of the skeleton, the greater trochanter of the hip joint (trochanter). This pathology is otherwise called trochanteric bursitis. Painful symptoms with trochanteric bursitis are often similar to signs of hip coxarthrosis. With trochanteritis, the inflammatory process covers the tendons and muscle ligaments located on the surface of the greater trochanter of the femur.
Most often, only one hip trochanter is affected. Moreover, trochanteritis, in comparison with arthrosis of the hip joint, is not accompanied by restrictions in motor activity.
Depending on the location of the inflammatory process, trochanteritis can be:
- aseptic form - inflammation covers the synovial membrane, but pathogens are not involved in the process;
- septic flow - an infectious, bacterial, viral or fungal pathogen spreads throughout the entire pelvic area. The purulent-inflammatory process also affects other surfaces in the vital organs;
- The tuberculosis form is a fairly rare disease, mostly diagnosed in childhood. A distinctive feature is the spread of inflammation both to the greater trochanter and to the tissue adjacent to the bones of the thigh.
Possible factors in the formation of inflammation:
- excess body weight;
- the presence of anatomical disorders in the pelvis and legs;
- hypothermia;
- problems with the endocrine system;
- excessive physical activity.
Most often, trochanteritis is diagnosed in women 25-30 years of age or during menopause due to hormonal imbalances.
Regardless of the age category and gender of the patient, pain symptoms characteristic of trochanteritis can appear against the background of problems with calcium metabolism and after severe damage to bones and joints by osteoporosis.
The doctor selects the treatment, taking into account the origin of the inflammatory process occurring in the greater trochanter. If the cause of the development of the pathology lies in infection of the body, antibiotics are indicated. The aseptic form of the disease involves treatment with non-steroidal anti-inflammatory drugs. If tuberculous trochanteritis is detected, the doctor prescribes anti-tuberculosis medications.
Thanks to intensive treatment, literally after 2 weeks a person can be completely cured. The main condition is to contact a specialist in time.
Treatment of hip dysplasia in newborns
Modern conservative treatment of hip dysplasia in newborns is carried out according to the following basic principles:
- giving the limb an ideal position for reduction (flexion and abduction);
- start as early as possible;
- maintaining active movements;
- long-term continuous therapy;
- the use of additional methods of influence (therapeutic gymnastics, massage, physiotherapy).
It was noticed quite a long time ago that when the child’s legs are positioned in an abducted state, self-reduction of the dislocation and centering of the femoral head are observed. This feature forms the basis for all currently existing methods of conservative treatment (wide swaddling, Freik's pillow, Pavlik stirrups, etc.).
- Without adequate treatment, hip dysplasia in adolescents and adults leads to early disability, and the result of therapy directly depends on the timing of the start of treatment. Therefore, primary diagnosis is carried out in the maternity hospital in the first days of the baby’s life.
- Today, scientists and clinicians have come to the conclusion that it is inadmissible to use rigid fixing orthopedic structures that limit movement in abducted and flexed joints in infants under six months of age. Maintaining mobility helps center the femoral head and increases the chances of healing.
Conservative treatment involves long-term therapy under ultrasound and X-ray control.
Subluxation of the hip joint (grade 2 dysplasia)
In this condition, the head of the femur is displaced, but is located in the acetabulum. At this stage, the swelling in the hip adductor muscle is so severe that it cannot stretch. The hip adductor muscle does not move and pulls the femur in one direction constantly. As a result, the joint does not move. Movement is limited, therefore, less intra-articular fluid is required. The hyaline cartilage that covers the head of the femur has less self-reproduction. It is for these reasons that X-rays show areas of the femoral head without a hyaline layer. In fact, the hyaline layer is everywhere, but it is so thin that the resolution of the X-ray machine does not make it possible to detect it.
The image below shows the condition of the femoral adductor muscle in the stage of subluxation of the hip joint in an electron microscope:
Figure 5. Condition of the femoral adductor muscle in the stage of pre-dislocation of the hip joint
Explanation of the picture:
- Muscle cells are increased in size (swelled inside) - red color.
- Swelling is noticeable between the muscle fibers, which compresses the swollen muscle cells - light color.
- The nuclei are displaced from the center of the muscle cells - dark color.
These changes in the long adductor muscle of the thigh in children indicate a disruption in the structure of the membrane components of the fibers, a disruption of the intracellular homeostasis of the calcium pump, which is a consequence of hypoxia and ATP deficiency and the cause of its inactivity.
When a child has hip dysplasia, the socket is flatter and more sloping. The process of ossification of the head is disrupted, excessively stretched elastic ligaments do not hold the head of the femur in the articular cavity, it moves upward and laterally, the limbus moves upward and becomes deformed, losing the ability to hold the head of the femur. This is a subluxation of the hip joint.
Figure 6. Subluxation of the hip joint
Wide swaddling of baby
Wide swaddling can rather be attributed not to therapeutic, but to preventive measures for hip dysplasia.
Indications for wide swaddling:
- the child is at risk for hip dysplasia;
- During an ultrasound scan, immaturity of the hip joint was revealed in a newborn child;
- there is hip dysplasia, while other treatment methods are impossible for one reason or another.
Wide swaddling technique:
- the child is placed on his back;
- two diapers are placed between the legs, which will limit the bringing of the legs together;
- These two diapers are fixed on the child’s belt with the third one.
Loose swaddling allows you to keep the baby's legs apart at approximately 60 - 80°.
Ultrasound diagnostics
This research method makes it possible to evaluate the cartilaginous structures that predominantly comprise the joint of a child in the first months of life, as well as muscle and connective tissue components. Ultrasound diagnostics makes it possible to conduct functional tests in real time. Additionally, dynamic monitoring can be carried out during the child’s treatment. The optimal time for conducting a screening study is the age of 4-6 weeks of life. The fact is that the hip joint is already, for the most part, formed.
Massage and exercise therapy
Exercises and massage are performed before feeding: these procedures stimulate blood circulation and improve nutrition of the structures of the hip joint. As a result, the growth processes of cartilage and bone tissue are stimulated, nerve conduction is enhanced - and the joint is formed correctly.
Massage movements are performed smoothly and gently. Apply stroking, rubbing and kneading the muscles of the thighs, buttocks, and lower back. The newborn is laid out on both his back and stomach. The duration of the massage is about 5 minutes. After the procedure, you can leave him to lie on his stomach for some time so that his legs hang down to the sides. This hardens and further strengthens the body.
A set of exercises is selected by a physical therapy doctor or pediatrician according to the degree of development of the disease. Most often this is: abduction of bent legs to the sides (contraindicated in slip syndrome), flexion and extension in the hip and knee joints. The movements are performed very smoothly. At first, they are recommended to be done in water, while swimming. The duration of the gymnastics is also about 5 minutes.
To work with a newborn at home, parents need to attend massage and exercise therapy courses at the clinic.
Wearing various orthopedic devices
Freik's pillow, Pavlik's stirrups and others. All this also helps to keep the baby's legs spread and bent. It is this method of treating hip dysplasia in infants that seems blasphemous to many parents, since they have to constantly see their baby “shackled” in orthopedic spacers.
It is worth remembering that this measure is necessary, but temporary, and should be treated with patience and understanding. The child's initial discomfort goes away within about a week, then he gets used to it and no longer feels any discomfort from wearing the splint. The duration of use of such devices is determined by the doctor based on periodic examinations and ultrasound diagnostics.
Epidemiology/Etiology
Total hip replacement is a frequently performed operation. Although it is performed in selected cases, it is also used for hip fractures (most often displaced fractures of the neck) caused by trauma (for example, a fall) or other pathological processes. Osteoporosis and osteomalacia are often the causes of hip fractures in older people. Arthritis, in its most common form, osteoarthritis, is also a common degenerative process among this population group. Because of the great success achieved in restoring function and mobility to those suffering from osteoarthritis, the total hip replacement procedure has become a common treatment for hip injuries. It is also used to treat juvenile rheumatoid arthritis, but only if other methods are unsuccessful.
Physiotherapy
Many physiotherapeutic procedures are used that eliminate the inflammatory reaction, improve joint trophism and reduce joint pain. The most commonly used procedures are:
| Electrophoresis | Using this procedure, you can introduce anti-inflammatory and painkillers into the joint cavity. |
| Mud therapy | During this procedure, the blood vessels dilate, resulting in improved blood flow in the joints. |
| Ultrasound | This treatment also has an anti-inflammatory and resorption effect. |
Contraindications for surgery
Absolute contraindications
- Progressive infection in the joint unless repeated surgery is performed as an immediate replacement or interval procedure.
- Systemic infection or sepsis.
- Neurogenic arthropathy.
- Malignant tumors that prevent reliable fixation of components.
Relative contraindications
- Localized infections, particularly in the chest and bladder, skin infections.
- Absence or relative insufficiency of abductor muscles.
- Progressive neurological disorders.
- Any pathological processes that quickly destroy bone.
- Dental or urological procedures required by the patient, in particular transurethral resection, must be performed before complete replacement of the hip joint.
Features of caring for newborns with dysplasia
With the right approach to treatment and care, dysplasia in newborns can be overcome. If your baby has disorders in the development of the hip joints, then he needs daily care and constant observance of special rules when carrying, feeding, and putting to bed.
- Hip dysplasia in newborns eliminates vertical loads on the legs.
- If the child is in a lying position, then his feet should hang slightly, this way better relieves tension from the thigh muscles.
- Transportation by car in a special child seat that does not interfere with the wide spread of the legs.
- The correct position when carrying in your arms: hold the baby in front of you by the back, while his legs should tightly grasp you from behind.
- Make sure that when feeding and sitting down, the hips are separated as much as possible.
The hip joint is an important supporting element of the human skeleton. He is constantly exposed to heavy loads when carrying heavy loads, running, and long walks. It is necessary to monitor the correct full development of this joint from infancy, otherwise in adult life the disease will still make itself felt, but it will be much more difficult to cure than dysplasia in newborns.
Clinical picture
Hip fracture: The patient often cannot walk, complains of aching pain in the knee, hip, groin, back or buttock, and has difficulty carrying heavy objects. The damaged femur is shown in the x-ray below.
Femoral neck fracture
Osteoarthritis: Felt or audible crunching when moving, inability to assume an anatomically neutral position. Often accompanied by pain and/or limited movement. X-ray studies usually indicate a decrease in joint space, subchondral sclerosis, cyst formation and the appearance of osteophytes.
Osteoarthritis of the hip joint
Rheumatoid arthritis: Movement of the hip joint is difficult and associated with pain; after rest, stiffness in movements and pain reappear.
Avascular necrosis: Symptoms are similar to those of osteoarthritis, and knee pain is also felt.
Avascular necrosis
Reduction of congenital hip dislocation
Indications for reduction of congenital hip dislocation:
- The child is over 1 year old. Before this, the dislocation is relatively easily reduced using functional techniques (splints and orthoses, see above). But there is no single unambiguous algorithm. Sometimes a dislocation after 3 months of age cannot be corrected by any means other than surgery.
- The child's age is no more than 5 years. At an older age, it is usually necessary to resort to surgery.
- The presence of a mature hip dislocation, which is determined by radiography and/or ultrasound.
Contraindications to closed reduction of congenital hip dislocation:
- Severe underdevelopment of the acetabulum;
- Severe displacement of the head of the femur, inversion of the articular capsule into the joint cavity.
Closed reduction for congenital hip dislocation is performed under anesthesia. The doctor, guided by X-ray and ultrasound data, performs a reduction - returning the femoral head to the correct position. Then, for 6 months, a coxite (on the pelvis and lower limbs) plaster cast is applied, which fixes the child’s legs in an extended position. After removing the bandage, massage, therapeutic exercises, and physiotherapy are performed.
However, some children develop a relapse after closed reduction of congenital hip dislocation. The older the child, the more likely it is that surgery will eventually be necessary.
Congenital dislocation of the hip joint (grade 3 dysplasia)
In this condition, the entire head of the femur is located outside the acetabulum. The dislocation occurred due to the fact that a contracture formed in the adductor muscle of the thigh. Those. the muscle cannot stretch even one millimeter. She pulled the femur out of its socket. The head of the femur is displaced upward and laterally by the force of the adductor muscles of the thigh.
The acetabulum is filled with fatty tissue. The lip of the acetabulum flattens and blocks the reduction of the head. The round ligament of the femur lengthens, the muscles of the hip joint shorten, contract and block the reduction of the head.
In the absence of appropriate treatment, late symptoms of dysplasia appear after a year. These include:
- Late onset of child walking independently (after 2 years).
- Incorrect (like a duck) gait.
- Trendelenburg's sign.
Prevention of pathology
If you do not want dysplasia to appear in your baby, you must take certain precautions:
- Taking vitamins, proper nutrition, light physical activity during pregnancy.
- Constantly following your doctor's recommendations during pregnancy. In this case, an important element of the examination is ultrasound, which can show health problems at an early stage of fetal development.
- Postpartum examination by an orthopedist, as well as an ultrasound of the hip joint.
- It is necessary to eliminate the causes that can lead to the appearance of pathology and provoke dislocation.
- The use of therapeutic exercises and regular physical activity, which will help place and fix the bone in place.
- Carrying a baby in a sling, as well as using wide swaddling.
- If the diagnosis of “dysplasia” is nevertheless made, then the baby cannot be put on his feet until the doctor allows it.
Modern methods of diagnosing and treating hip dysplasia are still far from perfect. In outpatient settings (clinics), cases of underdiagnosis (the diagnosis is not made in time for existing pathology) and overdiagnosis (the diagnosis is made in healthy children) are still common.
Many orthopedic structures and surgical treatment options have been proposed. But none of them can be called completely perfect. There is always a certain risk of relapses and complications. Different clinics practice different approaches to the diagnosis and treatment of pathology. Currently, research continues to be actively conducted.