Recently, an article was published on our website on the peculiarities of measuring the acetabular angle in children with deformity of the acetabulum, intended for specialists. But not only specialists, but also parents, who are most often interested in this parameter when diagnosing hip dysplasia, began to take an interest in this article. Therefore, counting on parents, I decided to expand a little on this topic . Let's consider the most relevant age of children - up to 1 year.
Features of the disease
Hip dysplasia is a destructive process during which the ligamentous apparatus that holds the pelvic bone (the largest joint in the human body) develops incompletely or incorrectly.
The head of the femur attaches to the pelvic bone in a place called the acetabulum. If any of the elements of the joint is underdeveloped, it means there is no proper articulation, as a result of which the ligaments are stretched and the head falls out of the socket.
Most often, parents of children under one year old are faced with this pathology. This is due to the fact that the baby’s ligaments are very elastic. This allows it to pass through the mother's birth canal without consequences. Therefore, any newborn baby has immaturity of the hip joint. As soon as he is born, active articulation occurs, which lasts for one year (more active in the first month of life). If at this time the joint develops incorrectly, and the acetabular angle deviates more than normal, it is customary to talk about dysplasia.
In 9 out of 10 cases, dysplasia affects girls, although there is no exact cause of this pathology. Most often it is associated with the period of the baby in the womb. It is as a result of hormonal changes that most strongly affect a woman in her first pregnancy that the ligaments can be too elastic.
Degrees and types of disease
It is customary to talk about dysplasia depending on the degree of pathology:
- The first (pre-dislocation) is minor disorders that do not lead to displacement of the hip joint, that is, a deviation of the acetabular angle from the norm.
- The second (subluxation) - the femoral head partially comes out of the acetabulum.
- The third (congenital dislocation of the hip) - the femoral head completely protrudes from the acetabulum, and the space that is freed is filled with connective tissue (this pathology requires immediate treatment - reduction).
Ultrasound can detect minor abnormalities in the development of the joint.
Types of hip dysplasia:
- Acetabular is a pathology that is directly related to the acetabulum.
- Rotational – the bones are positioned incorrectly.
- Underdevelopment of the articulations is observed on the proximal part of the femur bone.
Adults do not suffer from this pathology. If in the first year of life there were disturbances in the development of the hip joint and appropriate therapeutic measures were not taken, this can affect the normal well-being of an adult, even to the point of disability.
Sources
1 — Marx V.O. Study of an orthopedic patient // Minsk, “Science and Technology”, 1978. - 512 p. 2 - Hefti F. Pediatric Orthopedics in Practice // Springer. 2007. - 793p. 3 — Hilgenreiner (1925) Zur Fruhdiagnose und Fruhbehandlung derangeborenen Huftgelenkverrenkung // Med Klin 21: 1385–8, 1425–9 4 — Laurenson RD. The acetabular index: a critical review // J Bone Joint Surg Br 1959;41:702-10 5 - Staheli, Lynn T. Practice of Pediatric Orthopedics. Second edition //Lippincott Williams & Wilkins. 2006. - 490p. 6 — Tonnis D, Brunken D. Differentiation of normal and pathological acetabular roof angle in the diagnosis of hip dysplasia. Evaluation of 2294 acetabular roof angles of hip joints in children // Arch Orthop Unfallchir. 1968;64:197–228.
* - It will probably not be a big secret for the reader that the existence of the “Iron Curtain” in certain years in the USSR. As a result, there was a partial “separation” of Soviet science, incl. medicine from the “rest of the world” (author’s note).
Congenital hip dislocation
If the joint is incompetent, congenital dislocation of the hip is diagnosed. It is the most difficult and requires immediate treatment. If left untreated, the child may develop lameness in the future. It is most effective to treat pathology at 3-4 months of a baby’s life. It is during this period that it is customary to talk about the normal acetabular angle at 3 months. Only a specialist can diagnose pathology or deviation from normal values.
If the pathology is diagnosed late or treatment is ineffective, surgery is performed. Lack of timely treatment can lead to the development of coxarthrosis and disability in the future.
According to statistics, congenital hip dislocation occurs in one child out of 7 thousand newborns. It most often affects girls and is unilateral 2 times more often. Since the hip joints are deep, pathology can be diagnosed by indirect signs. Most often this is a limitation of abduction. In a healthy baby, the acetabular angle of the hip joint is 25-29 degrees at birth, and the legs are abducted 80-90 degrees. If the indications are less, it is customary to talk about dysplasia.
General recommendations
Children with a high risk factor for dysplasia are recommended to visit an orthopedist once every six months or according to an individual schedule prescribed by a doctor. During this period, you should engage in physical therapy and make full use of the capabilities of the hip joints.
Other recommendations for the prevention of dysplasia in children:
- Use special backpacks, slings, car seats. In them, the child’s torso takes the correct position and is not deformed.
- For newborns, special wide swaddling techniques are used. They can be mastered at courses for expectant mothers or at a consultation with a pediatrician or orthopedist.
- Massage or lightly exercise your baby regularly. Knead all joints and bones by performing flexion, extension, rotation and abduction movements.
- To securely fix your baby’s legs, discuss with your doctor an orthopedic device, for example, Pavlik stirrups.
Swimming lessons, visiting a gymnastics group, breathing techniques, and children's yoga are also suitable for prevention.
Causes of pathology
Modern science cannot say for sure why hip dysplasia occurs. But there are factors that increase the risk of developing pathology:
- First birth. The hormone relaxin, which is produced in large quantities during the first pregnancy, makes the joints more elastic and soft, as if preparing the woman for childbirth, but this affects not only the mother, but also the baby.
- The weight of the fetus is more than 3.5 kg. Such a child is considered large. During passage through the birth canal, the pressure on the hip joints is greater (the left side is more often affected).
- Birth of a girl. Nature arranges it in such a way that the female body is more flexible and therefore more susceptible to dysplasia.
- Breech presentation of the fetus.
- Hereditary predisposition - most often transmitted through the maternal line.
How is ultrasound of the hip joints performed in infants?
The examination is painless and does not require special preparation.
A special transparent gel is applied to the skin of the hip joint area, which is necessary to ensure close contact between the skin and the ultrasound sensor of the device. Having installed the ultrasound sensor in a certain position (at different angles), the doctor examines the images (“scans”) on the monitor. During the examination, the child is turned on the right and left sides. Upon completion of the study, parents clean the skin with a napkin and dress the baby.
Usually the conclusion is issued immediately after the end of the study. The ultrasound doctor interprets the results, and he can also discuss the results with you, but the final word remains with the doctor who referred the child for the study.
Symptoms
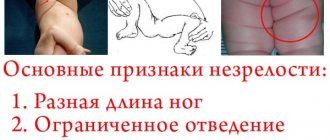
If a deviation from the norm of the acetabular angle can be noticed only with the help of ultrasound or x-ray, then dysplasia (depending on the degree) can be diagnosed by visual examination. Both a specialist and a mother can do this.
Signs that indicate hip dysplasia:
- The folds on the legs are asymmetrical. They can differ in shape, depth and be located at different levels, which becomes noticeable at the age of 2-3 months (deeper than the fold on the side where the dislocation or subluxation is observed). But asymmetry can also be observed in healthy children.
- Shortening the thigh. The head of the femur moves backward relative to the acetabulum. This is a severe form of dysplasia, which can be checked by placing the baby on his back and bending his knees. If they are at different levels, the diagnosis is confirmed.
- Marks-Orttolani slip sign. It is not a direct sign of dysplasia, since 60% of children with this symptom are absolutely healthy, but it is used as indirect evidence of pathology and only in the first month of life.
- Restriction in hip abduction. Dysplasia is diagnosed if the legs are separated at an angle of less than 80-90 degrees. For a seven-month-old baby, the norm is 60-70 degrees.
Additional diagnostic lines
In addition to angles, radiologists often use the concept of lines. These data help determine the relationship between the femoral head and the acetabulum and identify pathology.
Lines used in the diagnosis of the hip joint:
- Shenton line. It is carried out along the lower contour of the femur. It passes to the lower contour horizontally to the surface of the pubic bone. Forms a smooth arched line. With dysplasia, it has a broken shape.
- Calvet line. Crosses the outer contour of the ilium and goes to the upper contour of the femoral neck. With dysplasia it also has a broken structure.
- Ombredant-Perkins line. It follows vertically from the superior-outer point of the acetabular notch and continues with the longitudinal axis of the femoral diaphysis. With normal development of the musculoskeletal system, the proximal epiphysis is located inward from this line, in pathology - outward.
- Keller line. A horizontal line passing through both Y-shaped cartilages.
Lines are necessary for a schematic representation of the elements of the hip joint. A deviation from the norm will allow you to easily determine the presence of a displacement and its degree.
Diagnostics
An orthopedist can diagnose dysplasia. Ultrasound is performed, although this is not an accurate diagnostic method for pathology. With it you can control how the therapy process is progressing.
Most often, if a disease is suspected, an x-ray is prescribed, which can display the full picture of the pathology. Moreover, in newborn babies, the femur bone consists of cartilage, which may not be visible on an x-ray. Therefore, certain schemes and calculations are used.
It is with the help of X-ray examination that the acetabular angle is calculated, that is, the amount of inclination of the roof of the acetabulum and its deviation from the norm. But in the first months of a baby’s life such an examination is not carried out. As a preventative measure, therapeutic massages and swaddling are practiced.
Contraindications
Ultrasound examination of joints has no serious contraindications and is safe for all categories of patients - adults and children. Sometimes doctors find it difficult to diagnose patients who have scars in the scan area. For bumpy skin, the sensor of the device has poor contact with the surface, so the examination may not be informative. The presence of endoprostheses or metal in the body is not a contraindication to ultrasound. Therefore, it is sometimes used as an alternative for MRI of the hip joints of patients with metal structures in the body.
What is considered normal
If dysplasia or congenital dislocation of the hip is suspected, an x-ray examination is prescribed. This method determines the acetabular angle, that is, how much the acetabular cap is inclined to the Hilgenreiner line. In the first three to four months of life, its readings are maximum. The optimal angle dimensions can vary between 25-30 degrees. As the child grows and the body as a whole grows, this angle begins to gradually decrease.
By one year, the angle is already 20-25 degrees, and by 2-3 years – 18-23 degrees. At five years old, an angle of 15 degrees or less is considered normal.
Below are normal indicators and deviations, according to the Graph table:
- 3-4 months - normal - 25-30 degrees, 1st degree of dysplasia (subluxation) 30-35 degrees, dislocation - 35-40, with an angle of more than 40 degrees they speak of a high dislocation.
- 5 months – 2 years – normal – 20-25 degrees, subluxation – 25-30, dislocation – 30-35, severe dislocation – more than 35 degrees;
- 2-3 years – normal – 18-23 degrees, 1st degree – 23-28, 2nd degree – 28-33, 3rd degree – more than 33.
If a baby's acetabular angle exceeds the norm at 1 year of age, this may indicate congenital hip dysplasia or neuromuscular disorders. An indicator below normal is typical for children with Down syndrome and achondroplasia.
Normally, in an adult, the angle varies between 33-38 degrees. Intermediate values include indicators of 39 and 46 degrees; at 47 it is customary to talk about dysplasia.
Angles of the hip joint and their norms in children
Measuring the angles of the hip joint in children is carried out if congenital dysplasia is suspected. Timely medical care saves many from disability in adulthood, because dysplasia is a disorder in the formation of joints. Mostly girls suffer from it as a result of improper intrauterine development, frequent swaddling, and lack of vitamins and minerals. The exact reason has not yet been established.
Transverse scanning is carried out to determine the direction in which the femoral head is displaced in an unstable position (dislocation, subluxation). An X-ray sensor is placed in the area of the greater trochanter of the femur.
In the neutral position, the normal angle is 15-20 degrees. The rounded head of the femur is located in the acetabulum, the Y-shaped cartilage is in the central part. In front is the pubic bone, and in the back is the ischium.
To analyze a cross-section in a flexed hip position (about 90 degrees), the sensor is installed in the projection of the acetabulum and femoral head. Normally, the head should be completely immersed in the recess and not move during dynamic tests. In the picture, the joint looks like the Latin letter “U”. With subluxation, the image will more likely resemble the letter “V”, and with dislocation, it will resemble the letter “L”.
The angle of sagittal correspondence is formed at the intersection of the longitudinal neck of the femur and the tangent to the anterior and posterior edges of the roof of the acetabulum. The indicator is measured using an x-ray in the sacroacetabular projection. Additional factors that are taken into account when determining joint stability:
- centering of the head in the acetabulum;
- angle of inclination of the roof of the acetabulum.
If the x-ray was taken with the hips in an average position, then any changes in the direction of the longitudinal axis of the femoral neck or pathological angle values are a sign of dysplasia.
To eliminate errors in installation, it is enough to make corrections for abduction and adduction of the hips.
The Weisberg angle or central-border angle is formed by a vertical straight line and a line running from the center of the femoral head to the lateral side of the acetabulum.
In the medical system, the vertical-central angle is called the VCA angle. It is formed by a straight line (V) and a line running from the center of the femoral head through the anterior edge of the shadow of the femur behind the anterior edge of the glenoid cavity. X-rays are taken in the “false profile” position. The patient is in a standing position, and the cassette of the device is located behind the limb being examined. The angle between the pelvis and the cassette should be 65 degrees, and the distance to the bone should be 110 cm. To obtain an image, the beam of rays is directed to the center of the femoral head. The side view can be rotated 25 degrees.
The second name for Hilgenreiner's angle is cartilage angle. It is measured using a radiograph. The plane lies between the limbus and the transverse plane of the pelvis. The value allows you to determine the ossification of the hip bone. Delayed bone formation is another sign of congenital dysplasia.
The neck of the hip joint is one of the elements of the proximal articular end of the femur. In normal condition, the angle of rotation of the femoral neck around its axis is 20-25 degrees.
With the diaphysis, the femoral neck forms the neck-diaphyseal angle (CHA). Normally, in newborns it is 140-150 degrees, and with age it decreases to 120-130 degrees. Pathological forms are considered to be an obtuse angle, which is formed as a result of a varus or valgus pelvis, and individual, constitutional features.
The Sharpe angle (DCB) is the angle of inclination of the acetabulum in the vertical plane. It is formed by a horizontal line passing through the upper and lower edges of the acetabulum. To assess the indicator, a frontal radiograph is used. Using a photo you can measure:
- inclination of the depression in the vertical plane;
- depth of the glenoid cavity;
- length of the cavity entrance;
- glenoid coefficient.
The vertical correspondence angle is the part of the plane that is formed by crossing the tangent to the entrance to the acetabulum and the longitudinal axis of the femoral neck.
The reference point for the tangent (DA) is the lower pole of the teardrop and the outer edge of the roof of the acetabulum.
The normal angle for children over 6 years old is 85-90 degrees.
Acetabular angles at 3 months
When the baby turns 3 months old, the pediatrician refers him for a preventive examination to an orthopedist. It is not recommended to skip this examination, since this is where much attention is paid to the development of the hip joint. A specialist, after conducting a visual examination, may notice dysplasia. If it is detected in the maternity hospital, the baby is immediately sent to an orthopedist.
The femoral head, which is positioned incorrectly, can move relative to the acetabulum, thereby changing the structure of the joint. This is how preluxation, subluxation and dislocation appear, that is, three degrees of dysplasia. The greater the angle of inclination or acetabular index, the higher the risk of disruption of the correct structure of the hip joint in the future.
For example, if normal values at three months should be 25-30 degrees, then the normal acetabular angle at 6 months is slightly lower and varies from 20 to 25 degrees. At the same time, boys, as a rule, have a slope angle that is a couple of indicators lower than girls. That is why they are less flexible and plate-like. Often dysplasia in children is unilateral.
At an early age, the pathology may not manifest itself in any way, so not all mothers notice the deviation. If you identify the pathology in 3-4 months, you can achieve complete recovery using the least painful method in almost 100% of cases. Therefore, it is important not to skip a consultation with an orthopedist.
Animation of acetabular index measurement on a real image
And now we will analyze all this in practice. Above we looked at the scheme for measuring the acetabular index (the very first picture). In practice, measurements are usually more difficult because There are no clear lines like in the diagrams. I created an animation of the measurement on a real photo.
So, let's begin…
Patient 3 months old (from own archive).
- First we draw the Hilgenreiner line , it is determined relatively easily, along the top of the Y-cartilages.
- But next we must determine the upper-outer edge of the acetabulum . The younger the child, the more difficult it is. On the left acetabulum (picture above) it is better defined (don’t forget in the picture in front of you it is on the right), through it, perpendicular to the Hilgenreiner line, draw the Ombrédanne-Perkin line .
- This point is difficult to find on the right acetabulum. Therefore, Ombrédanne-Perkin at approximately the same distance from the point of contact of the ilium with the Hilgenreiner line.
- From the point of contact of the Hilgenreiner line with the ilium, draw a straight line to the intersection of the Ombrédanne-Perkin line and the edge of the acetabulum (both right and left).
- The angle between the last straight line we drew and the Hilgenreiner line is the acetabular index .
If you have questions and comments about the radiological indicator - the acetabular index "in general" - I will be glad to receive comments on this page.
Acetabular angles per year
If dysplasia was not detected in time (before the child reaches one year old), significant consequences are possible. But even at this age, it is quite difficult for parents to identify abnormalities in the structure of the hip joint. The following factors may indicate this:
- The child has turned one year old, but he still does not show the desire to walk or not stand on his feet at all.
- The baby is already walking, but at the same time he has a “duck” gait (rolls from one side to the other).
- The lumbar curve is significantly pronounced.
- Limitation of movements when spreading the legs, asymmetrical folds or lower limbs of different lengths.
The normal acetabular angle per year in children should be 20-25 degrees. Girls have a greater inclination (that is, angle) than boys, which depends on the anatomical features of the body. The higher the index, the more pronounced the signs of pathology and the higher the degree of dysplasia.
Treatment
If dysplasia is detected at an early age, for example, with slightly increased acetabular angles at 6 months, conservative therapy is carried out. It consists of using special orthopedic devices, with the help of which the child’s legs will be fixed in an extended position. This could be a Freik pillow, swaddling with two diapers between the legs, Pavlik stirrups, bandages, Becker pants, elastic splints.
It is also important to carry out therapeutic exercises and special massages, which will help not only strengthen muscles and joints, but also improve the health of the small organism as a whole. These methods are used at all stages of therapy and during the recovery period.
If a severe dislocation is diagnosed (grade 3 dysplasia), coxite bandages, Volkov or Vilensky splints are indicated for use. Corrective surgery is also performed if conservative therapy is ineffective.
How to warn
The absence of tight swaddling can reduce the risk of developing dysplasia significantly. Wide swaddling is possible when the baby's legs do not move together. If that doesn’t work, then you can put a soft toy or pillow between them.
Diapers are a good preventative method and a modern assistant for parents. They prevent the legs from closing (especially when filled), which is an excellent prevention of dysplasia. You can also take diapers several sizes larger.
Carrying backpacks and car seats are also an excellent preventative measure. It is worth undergoing an examination on time (no later than the baby’s six-month age). If the problem is not identified and corrected in a timely manner, in the future the child may develop an abnormal posture and gait, and he will experience serious difficulties with the musculoskeletal system.