Knee arthroplasty is a modern method of surgical treatment of the knee using high technology. In some cases, when a person suffers from pain in this area and is severely limited in mobility due to knee pathologies, knee replacement surgery becomes the only effective solution for improving the quality of life and getting rid of pain.
Indications
Knee replacement surgery is called arthroplasty. Like any other serious invasion, it is carried out only when indicated.
The latter include:
- severe limitations in knee mobility due to wear and tear or injury;
- severe pain in the knee area, felt even in a stationary position;
- irreversible changes in the joint caused by osteoarthritis;
- knee damage as a result of injury;
- deformations;
- diagnosed death of bone tissue as a complication of impaired blood supply;
- deformations or destruction resulting from a number of diseases (gout, rheumatoid arthritis, hemophilia);
- disorders that provoke abnormal bone growth of the lower limb.
Installation of a knee joint prosthesis is an operation of a fairly high level of complexity. This is a radical treatment method. Replacement is usually done if the disease progresses despite best efforts with therapy.
What to do if you have problems after surgery
Problems after endorothesis are quite rare, but they are one of the consequences that need to be eliminated as soon as possible. Most often, such problems include swelling. It may be due to fluid filling the inside of the knee or an abnormal position of the joint itself. After all, although joints are selected taking into account the anatomical characteristics of a particular patient, none of us is immune from mistakes. If problems arise, you should consult a doctor as soon as possible. In this case, you should completely stop doing physical exercise. It is quite possible that when selecting exercise therapy after knee replacement, the doctor made some mistake or the patient himself did not follow the recommendations correctly. In this case, after identifying the causes of the problem, the doctor edits the previously approved rehabilitation program and gives new recommendations.
Knee replacement surgeries
Knee replacement can be done entirely (total) or partially. In the first case, the endoprosthesis replaces both parts of the joint, in the second - only one of its sides (less time in the hospital, better results in terms of restoring mobility, surgery is sufficient for approximately 25% of patients with osteoarthritis).
There are alternatives to arthroplasty, but practice shows that in the long term their results are inferior to knee replacement . Alternative treatments include:
- Osteotomy is an operation to straighten the leg bone so that the load shifts from the damaged part of the knee to the healthy one.
- Mosaicplasty is the transfer of healthy hard cartilage tissue along with the underlying bone (partially) from another part of the knee to the affected area in order to restore it.
- Arthroscopy - washing and treating the affected area to remove pathological formations from pieces of bone and cartilage.
How to walk correctly after surgery
Not all patients know how to walk after knee replacement. To give the most general advice, it is based on the fact that the load on the operated knee should be as little as possible at first. The presence of pain indicates that the prosthesis is beginning to take root and the body must get used to it. To reduce pain, special strong painkillers and antibiotics are prescribed. While taking them, you should, if possible, completely avoid contact of your knee with water. Ideally, it is advisable to put a bandage on the knee and wear it until the stitches are removed after knee replacement (usually the duration of wearing the stitches is about 2 weeks). At the same time, the patient will need crutches after knee replacement - they should be used for the first time when moving. This need is explained by the fact that the load on the sore knee should be minimal. Accordingly, it is impossible to stand on a sore leg, but it is also impossible to remain motionless. After all, the patient is trying to return to normal life, and the more he sits in one place, the more the muscles in the area of the knee joint atrophy. And if you don’t move at all, then after a while one leg will become shorter than the other and the patient will limp for the rest of his life.
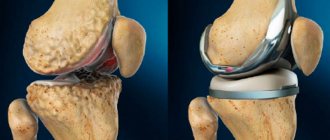
Knee endoprosthesis
What is a knee prosthesis? This is a complex design that follows the anatomy and dimensions of the joint being replaced. In other words, an endoprosthesis is the same knee joint, only artificial.
Today, many companies offer a wide range of knee and hip prostheses of various types and configurations. Their designs are constantly being improved to extend their service life after installation and increase the likelihood of normal healing in the knee.
The specific type of prosthesis is selected for each clinical case individually. Only a qualified specialist, after diagnosis and examination, can decide which knee joint prostheses are suitable for restoring the mobility of the patient’s lower limb.
Moreover, all modern endoprostheses (Diamond, Freedom, Lotus, Optimus, Oprtma, Titan) must meet a number of general requirements, including:
- biocompatibility (lack of rejection by the natural tissues of the knee and allergic reactions to the implanted knee joint endoprosthesis );
- load capacity (not lower than that of a real joint);
- the ability to maintain its original shape (during the entire service life, the prosthesis and its components should not be deformed);
- sufficient functionality (knee joint replacement is carried out, among other things, with the aim of restoring normal mobility; accordingly, the endoprosthesis must provide a good range of motion in the lower limb);
- anatomical shape (the knee joint prosthesis must repeat the structural features of the prototype, correspond to the natural dimensions and bends of the leg bone).
Endoprosthetics of the knee joint. Preparation, endoprosthetics, rehabilitation
In this article we will talk about knee replacement.
Knee replacement can be divided into three stages:
- Preparation for surgery;
- Performing knee replacement surgery;
- Rehabilitation after surgery.
There are several important points to consider when preparing for surgery. First, you need to come for a consultation with an orthopedic traumatologist so that he can look at your range of motion, your gait, and prescribe an examination in the form of x-rays.
If an orthopedic traumatologist sees indications for surgical intervention, he will give you a specific list of tests:
- Blood analysis;
- Urine tests, detailed forms;
- Gastroscopy;
- Ultrasound of the veins of the lower extremities;
- ECG;
- Fluorography of a pile of cells.
On the appointed day of hospitalization, you arrive early in the morning on an empty stomach to check all the tests you have taken. If the doctor does not see any contraindications, then you are hospitalized that day. Based on the ring examination and clinical conclusion, an endoprosthesis is individually selected for you based on the degree of connection.
A knee replacement typically consists of three components: a femoral component, a tibial component, and a polyethylene liner between them. Alloys can be cobalt-chromium alloy, titanium alloy.
You must have crutches with you, preferably axillary aluminum telescopic crutches and compression hosiery (first class compression) if there is no concomitant vascular pathology.
Documentation is completed, and you are hospitalized in a specialized trauma department. Next, consult an anesthesiologist. A suitable method of pain relief is selected for you - either spinal anesthesia or general anesthesia. Typically, these types of surgeries are performed under spinal anesthesia.
On the eve of the operation, in the evening, the medical staff prepares you. Cleansing enemas are performed and the hair at the surgical site is shaved. In standard cases, surgery occurs the next day after hospitalization.
On the day of the operation, you must hand over all valuables to relatives or medical staff. Early in the morning you are taken to the operating room. The anesthesiologist with whom you consulted meets you there. Performs spinal anesthesia. Spinal anesthesia involves the first injection of an anesthetic into the projection of the spinal column, then you no longer feel it and the anesthesia itself is performed. All this happens absolutely painlessly and under the control of an anesthesiologist.
Spinal anesthesia lasts for six hours from the moment it is performed. As a rule, the operation lasts from 1 to 2 hours.
In the first hours after surgery, you are monitored in the intensive care unit for no more than 12 hours. Next, you are transferred to the orthopedic traumatology ward, and the third stage begins - rehabilitation.
You are not allowed to stand up for 12 hours after surgery as spinal anesthesia may reduce sensation and movement in your lower extremities.
Your relatives can visit you the very next day after the operation.
Rehabilitation after endoprosthetics
So, the third stage is rehabilitation. It starts from the first days after surgery. On day 1, the attending physician explains to you how to perform movements in the lower extremities.
First, you need to perform flexion and extension in the ankle joints, in the knee joint, not operated and operated on, to a flexion angle of 45 degrees.
The attending doctor explains in detail how to lower your legs from the bed, how to take the first step with the help of additional support - this is in the form of a walker or crutches. Activation occurs within the ward. On the first day, this means walking to the toilet and back.
On the first day, a rehabilitation specialist will be assigned to you, who will monitor your movement and the load on the operated limb. On the second and third days you will be under the supervision of the attending rehabilitation doctor and postoperative dressings will be performed.
On the day of discharge, you are provided with documents: this is a passport of the implant that was installed for you, an extract with the full range of treatment, antibiotic therapy, the date of the operation and subsequent recommendations.
The recommendations state:
- Place of observation and rehabilitation;
- Duration of suture removal;
- Number of dressings.
The endoprosthesis passport will contain the date of the operation, the name of the operating doctor and all the stickers from the endoprosthesis components. You will need this for your follow-up at the clinic at your place of residence. You will need your implant passport at the airport when you go through the metal detector.
After inpatient treatment, you can undergo rehabilitation in a clinic in a physical therapy group under the supervision of a rehabilitation physician or in our sanatorium for two weeks under the supervision of our specialists.
It is especially worth noting that sutures are removed 14 days after surgery. Walking with the help of additional support (crutches or walkers) - 8 weeks after surgery. Compression hosiery (compression class 1) - 6-8 weeks and anticoagulation therapy for six weeks. You will take medications to prevent blood from thickening and blood clots from forming.
You will be fully socially adapted in the sixth month after the operation. It is advisable to consult your attending or operating doctor one month after surgery, three months, six months and a year. Further as possible.
Tibial insert FREEDOM
More details
All knee replacements
Classification of endoprostheses
Materials for the manufacture of a knee joint prosthesis to replace the latter: ceramics, metal alloys, polyethylene. Depending on the design features, endoprostheses are divided into models with a movable and fixed platform.
Prostheses with a movable platform have an insert that can rotate in the metal part. This gives additional amplitude when moving the knee after surgery in the medial, lateral direction. In endoprostheses with a fixed platform, the elements - part of the tibial element and the metal component - are firmly connected to each other.
Another classification divides knee replacements into 3 types.
- Unilateral or unicondylar endoprosthesis. It is used for partial replacement of the knee joint in its upper part (prosthetic replacement of an area on one of the femoral condyles).
- Total or bilateral knee replacement (usually metal). Used to replace both parts of the joint (both femoral condyles are covered). The design of such an endoprosthesis differs from the unicondylar one in that it has more powerful attachments to the bone and increased width.
- Total endoprosthesis with axial stabilization. It is also used in total knee replacement operations, when its parts (upper and lower) are fixed with long pins along the longitudinal axes of the femur and tibia. Pins for secure fixation are driven into the space filled with bone marrow (medullary cavity).
Another sign of the classification of knee prostheses is the method of their fixation. There are 2 options: structures installed with cement and cementless methods. In the first case, when replacing a knee joint, its artificial analogue is stabilized (fixed) with quick-curing medical cement. With the cementless method, fixation is carried out as bone tissue grows into the implant.
Cemented knee joint prostheses are more reliable and versatile (used in any type of replacement surgery). An endoprosthesis for cementless installation has a special surface - porous, textured (it provides the opportunity for bone to grow into the implant).
What not to do after surgery
As already noted, as a result of knee replacement, part of it is replaced with an artificial element. Therefore, no matter how the patient tries to restore the full functionality of the knee, the presence of a foreign body will leave a trace of this fact forever. Any artificial joint gradually wears out. Accordingly, the patient will need to lead a calm lifestyle. It is advisable to completely abandon active sports, as well as strength exercises. Any awkward movement can lead to a dislocation or fracture of the knee, and this will lead to another operation. Therefore, you always need to be as careful as possible in everything.
When leaving the hospital, it is recommended to obtain a certificate from the orthopedist stating that you have had an endoprosthesis inserted. The fact is that this prosthesis consists of metal parts. Therefore, when passing through various types of metal detectors, they will be triggered. To avoid problems with security guards, sellers and anyone who uses metal detectors in their work, it is better to have this certificate with you.
If during the rehabilitation process or after the end of its most intensive phase any unpleasant or painful sensations appear, do not hesitate. It is quite possible that the situation can be corrected relatively quickly, so you should consult a doctor as soon as possible - he will identify the cause of the pain and then, depending on it, will develop appropriate recommendations.
How is the operation performed?
Knee replacement surgery can be performed either under general anesthesia (more often) or under spinal/epidural anesthesia (less often). Takes 1–3 hours. Progress of the procedure:
- an incision is made in the front of the knee (the surgeon opens the kneecap and displaces it to gain access to the tissues of the joint located behind it);
- removal of damaged tissue (femoral head, tibia);
- measuring bones and preparing the prosthesis (the dimensions must be kept extremely accurately);
- cleaning the ends of the bone and installing an endoprosthesis;
- replacement of a section of femoral bone tissue with a curved metal element;
- the end of the tibia is replaced with a plate (also metal, but flat);
- installation of a plastic gasket between the elements of the knee prosthesis (it replaces the cartilage necessary to reduce friction during movements);
- replacing the back of the kneecap if necessary;
- applying sutures or clamps and a bandage (sometimes it is replaced with a splint to fix the limb in a stationary position).
Rehabilitation
After knee replacement, the patient remains under observation (in the hospital) for 3–5 days. During this time, he undergoes a special course of exercises (physiotherapy to strengthen the knee).
Features of the rehabilitation period:
- swelling of the feet and legs is likely;
- movement - with the help of special means (metal frame or crutches);
- classes can be carried out on a simulator for passive movement (the patient remains in bed, the leg is fixed in an elevated position, and a special support makes movements of the knee, which improves its blood supply and helps reduce swelling);
- There may be noticeable discomfort when walking and making leg movements (this is normal).
Complete rehabilitation after knee replacement can take up to 2 years, but the patient can often move independently without special aids after 6 weeks. And after 2 months, many are already driving vehicles.
Is sick leave required after surgery?
For the first couple of weeks, the patient will only be able to walk very carefully and with the help of crutches or handrails. Accordingly, there can be no talk of any full life. Therefore, sick leave after knee replacement is issued for 2 weeks. Moreover, a day and a week after discharge, the patient must undergo observation by an orthopedist. Therefore, there can be no talk of any work. In the future, you can no longer use crutches and the load on the knee should be gradually increased. In the first 2 weeks, you should not forget about performing special physical exercises aimed at improving knee mobility. By performing them, the patient develops ligaments and muscles, gradually returning them to full functionality. The essence of the exercises comes down to bending and straightening the knee, raising the leg, and subsequently walking up a low ladder and squats.
Paraprosthetic infection of the knee joint - diagnosis
Infection is one of the most common complications during endoprosthetics. With revision intervention, the number of victims of infection increases to 40%. And these numbers are increasing every year, as the number of people who have resorted to endoprosthetics is growing. Previously, these were elderly patients, but now young people are getting implants. Therefore, in the 21st century, endoprosthetics is literally on stream. The causes of paraprosthetic infection are different and not fully understood. Recently, publications have increasingly appeared on the connection between the pathogen and the material from which the prosthesis is made, as there is evidence of the ability of some microorganisms to adhere to certain types of implants.
The severity of symptoms of infection after endoprosthetics depends on the virulence of the pathogen, the source of infection, the condition of the patient and his age. In the first few days after implantation of a knee prosthesis, clinical data still do not clearly distinguish between postoperative tissue reaction and initial infection. Classic signs of inflammation (hyperthermia, redness, swelling, pain and dysfunction) may initially exist without the presence of infection, and their absence or severe delay during the first week should be a good reason for further monitoring.
Clinical data
Paraprosthetic inflammation manifests itself after installation of the endoprosthesis for several months; depending on the time of occurrence, it is distinguished:
- if symptoms appeared within 30 days after the intervention, they speak of an acute form;
- if signs of infection appear 30 days after placement of the implant or within a year after it, then we are talking about a chronic form;
- if complaints appear 12 months after surgery, then doctors talk about an acute hematogenous infection
Febrile body temperature, as an indication of infection, usually occurs three to six days after arthroplasty, more so in the case of a (super-)infected postoperative hematoma. However, the presence of persistent (sub-)febrile fever should, at the very least, be considered an alarm that requires enhanced monitoring. If systemic parameters of sepsis occur, postoperative wound infection should be excluded.
Sometimes the disease occurs latently without obvious signs. The presence of effusion without local or systemic signs of infection is usually nonspecific. It can be punctured under sterile conditions so that the punctate can be further examined microbiologically. The fistula form is characterized by the appearance of a fistula in the form of a pathological course from the prosthesis to the epidermis, through which pus is released.
The diagnosis is based on examination data, anamnesis, patient complaints and additional examination. Due to the vagueness of symptoms and the absence of specific examination results, making a diagnosis of parainfection is quite difficult and, first of all, depends on the experience and qualifications of the doctor.
Main complaints
People usually come to the doctor with complaints of swelling of the joint, limited functionality, low-grade fever (and sometimes fever), redness and swelling in the knee area.
But the classic signs of inflammation may be absent, and the main symptom of infection and the patient’s complaint will be constant pain in the knee, vaguely associated with movement and worsening at night. The pain can be aching or throbbing, local or radiating.
If the paraprosthetic process is deep, the muscles next to the implant are affected. Intoxication spreads throughout the body, the general condition worsens, the temperature remains high, the patient shudders, weakness is noted, and vomiting is possible.
The doctor clarifies with the patient the nature of the pain, its onset, the dynamics of the process, and finds out whether treatment was carried out (if complaints appeared outside the clinic)
If the infection is latent, there may be no pronounced complaints; the patient notes fatigue, aching pain, and slight swelling in the joint area.
Any complaint of pain in the area of the endoprosthesis, especially during the first three years after surgery, should be considered as an infectious complication. In addition to complaints, the doctor collects a thorough medical history, finding out:
- Do you have any joint diseases?
- whether the patient suffers from rheumatism;
- whether you took a long course of medications;
- were there any injuries or falls after the operation;
- what condition are the vessels in?
- do you have diabetes?
- do you have osteoporosis?
- what type of prosthesis and whether there were problems with the postoperative wound;
- whether there is cardiovascular insufficiency;
- Is there any pain in the area of the prosthesis, and when did it appear?
Patient examination
During a clinical examination, attention is drawn to an enlarged knee or limited swelling, a change in the color of the skin around the joint. The doctor determines whether there is a restriction of movement. Unambiguous confirmation of paraprosthetic infection are fistulous tracts. The edges of the wound may diverge, discharge appears from it, and sometimes areas of necrosis form.
On palpation - enlargement of the inguinal lymph nodes, increased local temperature, pain in the area of the projection of the joint space. Tachycardia (rapid heart rate) and rapid breathing are noted.
Laboratory research
Usually, blood is taken for clinical and biochemical analysis, and blood is donated for culture. Laboratory tests include, in particular, the determination of serum CRP [C-reactive protein], which currently represents the most important control parameter in addition to the white blood cell count in the blood picture. However, here the absolute values of the corresponding indicators are of less importance compared to the course of the disease. Immediately after surgery, CRP (C-reactive protein) values almost always increase and then begin to fall in the following days. The absence of a decrease in CRP or its continued increase, combined with clinical signs of infection, indicate the presence of infection until proven otherwise. In this context, erythrocyte sedimentation rate (ESR) is unlikely to play a role in the current clinical picture, except to provide indirect monitoring of the long-term course of the disease and the determination of chronic infection.
Regarding laboratory parameters, it should be noted that, for example, an infection such as Staphylococcus epidermidis usually does not cause a significant increase in CRP and clinical parameters are often very nonspecific.
For example, a change in the number of leukocytes may be observed, but the information content of this parameter of paraendoprosthetic infection is not significant. If the cultures of the synovium are sterile, this does not mean the absence of parainfection; it is necessary to repeat the examination of tissues for culture from different areas of the knee joint.
Instrumental studies
There is absolutely no doubt in the case of large soft tissue defects with visually distinguishable prosthetic components identified during instrumental examination.
- Sonography
Sonographic examination plays an important role when early infection is suspected, as it can be used to visualize periprosthetic effusion or hematoma and, if necessary, to perform sonographically guided puncture. The basis for diagnosis may be detected areas of hypoechogenicity.
- X-ray
A conventional x-ray image is unlikely to convey the target information in early parainfection, since there are very few specific x-ray signs. In contrast, with the late form there is a different situation: in this case, periprosthetic signs of weakening on the x-ray can be observed at two levels. The presence of infectious inflammation can be suggested by the periosteal reaction and signs of osteolysis revealed in the image. Regular x-ray monitoring is mandatory to see the dynamics of the process. If a fistula exists, then X-ray fistulography can provide evidence of the involvement of the prosthesis in the pathological process. An X-ray image of a fistula clarifies its localization, the branching of its passages, connection with organs and tissues, and finds purulent accumulations (leakage). In addition, if a fistula is present, a smear is taken for bacteriological examination, including a resistogram.
- CT and MRI
Due to the layering of the prosthesis when implanting, in most cases, steel components, computed tomography (CT) and magnetic resonance imaging (MRI) play virtually no role here (with the exception of titanium prostheses).
- Scintigraphy
In case of a long course of the disease, (three-stage) scintigraphy can also be used, with which the pathological metabolic activity of soft tissues and/or bone in the periprosthetic area can be proven.
- Biopsy
Tissue puncture in the area of the knee joint to obtain puncture is carried out under ultrasound control. The resulting contents are studied in the laboratory, where culture is carried out to identify the pathogen.
Only after interpreting the data obtained can the doctor develop the optimal treatment strategy.
Conclusion
Correct diagnosis will help answer many medical questions, find out the involvement of surrounding tissues and the design of the endoprosthesis in the inflammatory process, find out its prevalence, understand at what stage the blood circulation is impaired and, most importantly, develop optimal and effective treatment tactics. Treatment of paraprosthetic infection is lengthy, using expensive drugs and materials. Debate continues about the choice of optimal technologies that can restore joint function with minimal risk of re-infection, so it is very important to find a doctor with extensive experience in arthroplasty and a specialized clinic with modern equipment.