What is Achilles tendinitis?
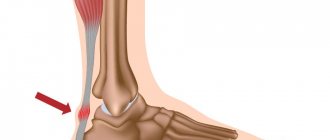
The Achilles tendon is considered one of the densest formations in our body. With the participation of this ligament, the heel is raised and pushed off the surface with the fingers.
When using unsuitable shoes, while moving on an inclined surface, or jogging, significant loads are placed on the heel tendon, which causes frequent injury.
In addition, a load of identical force can reduce the strength of this ligament and provoke the appearance of dystrophic disorders. All kinds of changes in conductivity can also lead to tissue dehydration, slowdown of metabolic processes and salt deposition.
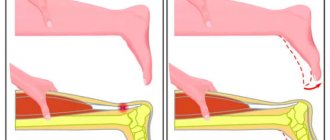
As a result of the above processes, the tendon's resistance to micro-tears that occur during sudden changes in body position and stretching is significantly reduced.
People in the middle age group (over 35 years old) are susceptible to similar degenerative processes. However, in people who daily engage in strenuous physical work and athletes, such manifestations can occur much more often, which is due to regular overload and premature aging of tissue in the tendon area.
According to experts, it is precisely those who engage in active sports training and do not pay enough attention and time to the recovery period that develop Achilles tendinitis. A similar situation can manifest itself when carrying out excessive loads without going through the preparatory stage.
As a result, the muscle stretches weakly, inflammatory processes appear, and damage appears in the ligament area. This is accompanied by acute pain during physical activity.
If a person does not visit a specialist in a timely manner and does not begin treatment procedures, this may provoke a tendon rupture in the future.
In some situations, damage may be mechanical. But the most common is tendinitis of the Achilles tendon, which is accompanied by the appearance of inflammatory foci.
If Achilles tendonitis is of a similar nature, then treatment is carried out with the use of anti-inflammatory drugs. In case of mechanical damage, long-term therapy and special exercises are required until the ligament tissue is fully restored.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Types and forms of Achilles tendonitis
Taking into account the factors that caused the onset of the disease and the nature of the disease, there are 4 types of Achilles tendinitis:
- Aseptic acute. When connective tissue fibers are damaged, the body responds, but the infection does not penetrate the affected area;
- Fibrous. It is chronic. In this case, the functional tissue is gradually replaced by pathological formations (scars);
- Ossifying. It is chronic in nature. Tissues lose elasticity, calcium formations appear;
- Acute purulent. The infection penetrates from nearby inflammatory foci or from the outside.
There are also three forms of pathology:
- Enthesopathy. The inflammatory focus is located in the area where the ligament attaches to the heel bone;
- Peritendinitis. Inflammation spreads to nearby tissues;
- Tendinitis of the heel or Achilles tendon. The lesion is located at the location of the heel connective tissue cord.
Calf stretch
Standing facing the wall, arms resting at chest level. The heel of the developed (back) leg touches the floor, the toes point straight ahead. Bend your back knee and gently lean toward the wall until you feel a stretch in your shin. Hold the stretch for 15-30 seconds. Return to the starting position. Repeat 3 times
Causes of Achilles tendonitis
Factors that cause disturbances in this area can be of a different nature.
Age factors
As you know, the tendon is represented by two types of fibers: collagen and elastin. The former are responsible for the strength of the ligament, the latter provide the ability to stretch.
Typically, the extensibility of the Achilles tendon is 5% of the original length. Due to this, the lower limb is able to perform springy movements, which also indicates the shock-absorbing ability of the tendon.
However, as the body matures, the ligament's ability to stretch decreases, and increased loads can cause micro-tears and damage to the fibers.
This explains why experts do not advise people over the age of 35 to start sports training. In such situations, a mandatory warm-up and warming up of the muscles is required.
Excessive loads
Lesions may occur in persons with professional physical training. The reason for this lies in the presence of significant and regular tension in the ligament area. As a result, if there is no sufficient rest period, the tissues are deprived of the ability to relax and regenerate.
As a rule, athletes do not attach due importance to the initial signs of the disease. This can provoke further intensification of degenerative processes, lead to the appearance of a chronic disease, and can also cause complete rupture of the ligament.
To prevent such complications, even mild pain should be taken as a signal to action, because they can indicate the appearance of microtears in tissues and indicate the need to stop (temporarily or completely) sports training. Therefore, if you notice the first signs of the disease, or you are diagnosed with Achilles tendonitis, treatment should begin as early as possible. And only an experienced doctor will tell you when you can resume exercises, or inform you about the need to stop them completely.
A few words about overpronation
The physiological rolling of the foot inward is called hyperpronation. This position of the ligament during walking and other active movements often leads to injury or excessive stretching.
. . . .
Using inappropriate shoes
Achilles tendinitis and, as a consequence, the need for treatment of such a pathology can also provoke:
- Using inappropriate shoes when performing physical exercises. This contributes to irrational load distribution and can negatively affect the function of the tendon;
- Using high heel shoes. Women who prefer such shoes also risk damaging ligaments in this area. However, they may experience discomfort in this area the next time they wear flat shoes.
Haglund's deformity
It is a bony formation that looks like a bubble and is located in close proximity to the area adjacent to the tendon. Such growth causes the need for additional stretching of the ligament under significant loads.
Depending on the presence of inflammatory foci, the degree of hardness of the formation is determined.
Infectious processes
In this situation, the appearance of inflammatory foci is associated with the penetration of infection.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Symptoms of Achilles tendonitis
When considering calcaneal or Achilles tendonitis, symptoms and the need for treatment, the form of the pathology should be taken into account. It can manifest itself either acutely or develop into a chronic process.
The acute form is characterized by a gradual development of the pathology: initially, a person begins to experience pain when engaging in sports exercises, which disappears during a break. Recurrence of discomfort is possible with new physical activity. The subsidence of the pain syndrome can be explained by the healing of micro-tears during a long break after training. However, if you have signs of Achilles tendinitis at the initial stage, but do not want to undergo treatment, the disease may gradually become chronic.
In such a situation, increased pain occurs over some time. In addition, discomfort may be of the following nature:
- It becomes more pronounced during physical exercise, and can occur even after the preparatory stage (warming up the muscles);
- The length of the recovery period does not affect the possibility of eliminating discomfort. It can occur even in the morning;
- When moving on an uneven surface, the pain intensifies.
In this case, the following characteristic manifestations may be observed: the density of the ligaments increases; tension in this area increases; redness of the skin may be observed; mobility is lost at the location of the ankle; localization of pain can be observed on an impressive surface; there is a possibility of swelling; difficulties arise when trying to rise on your toes; In some situations, a peculiar creaking sensation occurs in the ankle joint.
Signs of the disease
If the pathology is preceded by trauma, as happens in most situations, then the signs of exacerbation quickly increase and cannot go unnoticed. If the disease occurs against the background of rheumatic pathology, then the symptoms will appear gradually and resemble a chronic course. If bursitis occurs against the background of Achilles overload, then the patient will feel a subacute process, which will be felt by chronic and sluggish pain during periods of rest. The main complaint that the patient presents is pain in the supraheel region, which intensifies with movement and against the background of shoe pressure.
Upon external examination, you can notice a slight swelling and local redness, and local discomfort is present. At first, the swelling looks small, and then acquires a larger area as the inflammatory process in the tendon progresses. If a patient develops anterior Achilles bursitis, a spindle-shaped swelling with a characteristic protrusion on both sides of the tendon is detected. If the posterior bursa is affected, a round or oblong soft formation is observed above the tendon.
Signs of Achilles bursitis
If you palpate the posterior Achilles bursitis, the pain will be felt under the tendon. In case of inflammation of the anterior part, discomfort occurs in the superficial tissues. Local redness, increased body temperature, weakness and general malaise are also observed. If the pain is acute, it negatively affects the patient's quality of life. He suffers from insomnia, as he cannot sleep due to severe pain.
Diagnosis of Achilles tendinitis
Before making a diagnosis, the specialist examines the patient and studies the complaints received from him.
The following methods are used to confirm tendinitis:
- MRI. The information value of this method is noted in advanced stages of the disease (it is possible to find out whether fluid has accumulated in the affected area) and in the presence of scar changes;
- Radiography. The presence of Achilles tendonitis can be determined by x-ray. It becomes possible to detect pathological manifestations caused by the presence of calcium deposits;
- Testing for the presence of breaks. The ability to flex the joint while lying on the stomach is assessed. In this case, it becomes possible to determine the etiology and localization of the pain syndrome;
- Research in laboratory conditions.
Treatment of Achilles tendonitis
Before the appearance of serious degenerative changes in tissues, the disease can be treated without any further complications.
However, if a patient is diagnosed with chronic Achilles tendonitis, it is much more difficult to cope with this disease, since it often leads to a decrease in the motor activity of the ankle joint and tendon ruptures. Next, we will consider the main measures that, in the presence of this pathology, must be carried out without fail:
- In the first time after injury, compresses or lotions with ice are used, which are applied to the affected area every 3 hours;
- If heel tendonitis occurs due to infection, it is not recommended to use the above method;
- Decreased motor activity of the joint. This is one of the main measures that involves the use of plaster to fix the ankle joint.
After injury to the lower limb, it must be kept motionless for 48 hours. This will eliminate swelling, shorten the recovery period and prevent the appearance of a hematoma.
Treatment with shock wave therapy for achillotendinitis
The most effective and modern way to eliminate inflammatory processes characterized by the appearance of calcium deposits in the tendon area is shock wave therapy.
The positive effects of this new technique are based on the following mechanisms:
- Calcium formations in the tendons are destroyed;
- The pain syndrome is not only relieved, but also completely disappears;
- It is possible to completely normalize blood circulation;
- Metabolism improves;
- Inflammatory processes are eliminated;
- Tissue regeneration occurs;
- Motor activity in the lower extremities is normalized.
It is possible to obtain a sustainable healing effect and ensure positive dynamics from the first sessions. The frequency and intensity of procedures is determined individually. In addition, a timely visit to a specialist allows you to get the desired result when exposed to shock waves.
Experienced physiotherapists who are able to conduct a thorough diagnosis, accurately diagnose and select the most effective treatment procedures will work with you at the medical center. At the same time, the priority direction of our activity is the implementation of UVT procedures using innovative Swiss equipment and with impressive discounts.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Drug treatment for Achilles tendinitis
First of all, you should ensure the immobility of the foot in order to minimize the load on it. This is achieved by the following methods:
- Plaster or splint application;
- Use of crutches;
- Application of a fixing bandage;
- Applying a cotton plaster;
- Use of special orthopedic devices.
It is also recommended to use the following medications:
- Drugs included in the group of non-steroidal anti-inflammatory drugs, which include Diclofenac, Nurofen, etc.;
- Antibacterial therapy drugs;
- Use of external agents: Nise gel, Voltaren, etc.;
- Compresses using Analgin and Acetylsalicylic acid - for pain relief.
After eliminating pain, massage and general strengthening gymnastic exercises should begin.
Physiotherapeutic treatment of achilles tendinitis
When it comes to how best to treat Achilles tendinitis, physical therapy is paramount. It helps restore blood flow, improves metabolism and speeds up the recovery period.
In this case, the following activities are carried out:
- Stimulation with light waves of a fixed length (laser exposure);
- Exposure to low frequency electromagnetic field;
- A method based on the influence of galvanic current and an active anti-inflammatory substance introduced through it;
- Use of high-frequency sound pulses;
- Shock wave therapy: destruction of calcium formations using low-frequency shock waves;
- Warming up;
- Massotherapy;
- Special exercises.
Surgery
The need for surgical intervention arises in situations where conservative therapy has not given the desired effect. In this case, the following sequential steps are implemented:
- The skin is cut to gain access to the ligament;
- Excision of dense calcium formations and other pathologically altered tissues is performed;
- After 50% of the affected tissue has been removed, a procedure is performed to restore collagen fibers using tendon from the plantaris muscle.
The duration of the recovery period reaches 12 weeks. The patient wears a cast for 30 days after the intervention.
The start of rehabilitation procedures is determined depending on the rate of tissue healing. As a rule, the duration of this period reaches 2 months.
Make an appointment Online booking
- Clinic on Krasnopresnenskaya +7 (499) 252-41-35 Volkov lane, 21
- Clinic on Varshavskaya +7 (499) 610-02-09 Varshavskoe highway, 75, building 1
- Clinic in Annino +7 (495) 388-08-08 Varshavskoe highway, 154, building 1
Folk remedies
Many patients are interested in how to treat Achilles tendonitis using traditional methods. First of all, you should check with your doctor about the possibility of such a treatment method. In this case, the following means can be used:
- Seasoning curcumin. This is an antibacterial agent of natural origin, which also has an anti-inflammatory effect and eliminates the inflammatory process in the tendon area. However, you should consume this substance at least 500 g per day;
- Infusion of walnut partitions. For this purpose, use 0.5 liters of vodka and 1 glass of partitions. The infusion period reaches 3 weeks. You need to use the product 1 teaspoon twice a day;
- Solution with mumiyo resin. The mixture is applied to the affected area, and also consumed orally in the form of a solution in milk;
- Pine-salt baths;
- Ice massage. Has an analgesic effect.
General information about the disease
Achilles tendon bursitis is one of the most common pathologies in modern traumatology.
The Achilles attachment often becomes inflamed and is no less common than elbow, knee, and shoulder bursitis. In most cases, the disease develops under aseptic conditions and is preceded by trauma resulting from a blow or fall. In rare cases, purulent inflammation occurs. The pathology is more common in young men and women who lead an active lifestyle. Men are more likely to develop the disease because, due to many habits, they are forced to run or walk more. The disease in the acute stage is easier to treat than the advanced, chronic form. In rare cases, a complication occurs in the form of ligament rupture.
At the point where the Achilles attaches to the heel bone there are two mucous bursae that facilitate movement. The anterior bursa is located between the ligament and the bone, and the posterior bursa is under the skin. Normally, the bursae contain a small amount of fluid, which allows the ligamentous apparatus to glide during movements. If aseptic inflammation develops, the amount of fluid increases due to serous inflammation. The walls of the bag are saturated with serous fluid.
Achilles tendon - where is it located?
If a closed type injury occurs, then excess fluid occurs against the background of a rupture of the vascular bed and is hemorrhagic in nature. If there is an open lesion, then without the proper level of sanitation it becomes purulent due to the entry of pathogenic microflora inside. If the acute course of the disease is not cured, it turns into chronic inflammation due to the growth of fibrin in the wall of the bursae and the formation of scar adhesions.
Preventive actions
To prevent the development of calcific tendinitis of the Achilles tendon, the following principles should be adhered to:
- If you are advised to exercise for Achilles tendonitis, the load should be increased gradually;
- Warming up the tendons and muscles is a must before performing any physical exercise;
- For daily use and sports activities, you should choose the right shoes;
- If pain occurs, you must stop training.
Achilles tendonitis, as evidenced by reviews, is easily treatable, but only if it is carried out at the initial stage of the disease. In advanced forms, severe consequences such as chronic Achilles tendinitis or tendon rupture can occur. To achieve a positive result, it is necessary to use a set of procedures aimed at ensuring immobility of the affected area, as well as achieving the necessary analgesic and anti-inflammatory effect.
Prognosis for recovery
Considering Achilles tendinitis and reviews of the treatment of this disease, we can conclude that the recovery period primarily depends on the degree of damage. With a timely visit to a specialist, more than 80% of patients can count on positive treatment results. In this case, the rehabilitation period can reach 3 months.
The resumption of usual physical activity must be carried out gradually, which will prevent deterioration of the heel tendon.
Treatment of achillodynia (achillobursitis)
The remedies commonly used for bursitis—rest, heat, ointments, diathermy—rarely lead to improvement. High heels, by relaxing the Achilles tendon, usually make walking easier.
But the most reliable and fastest method of treating late bursitis, which has become chronic, must be the surgical removal of the diseased mucous bursa with an incision on the side of the Achilles tendon. Complete restoration of walking with this treatment of achillodynia (achillobursitis) is achieved in three to four weeks.
Physiotherapy is used in the treatment of Achilles bursitis.