One of the most common ailments of the musculoskeletal system (MSD) is gonarthrosis. A serious degenerative disease affects the tissues of the knee joint and can lead to irreversible consequences, including knee deformation and loss of limb mobility.
The knee is an important part of the human musculoskeletal system, responsible for the ability to move freely. Due to increased loads, the pathogenesis of the structure occurs quite rapidly, which significantly affects a person’s quality of life and can become the reason for obtaining the status of “disabled person”, as well as the accompanying restrictions.
According to statistics, it is this form of arthrosis that is most often diagnosed when patients complain of the presence of corresponding symptoms.
What is gonarthrosis?
Gonarthrosis is a type of arthrosis of the deforming type, the destructive processes of which are localized in the hyaline cartilage of the knee.
According to medical data, degenerative-dystrophic processes are exclusively non-inflammatory in nature and can occur against various backgrounds, which indicates the presence of a large number of probable causes of gonarthrosis.
The disease can be traced through the emergence of a complex of signs from which the symptomatic picture is formed. These include: a feeling of stiffness, tightening under the knee, as well as the appearance of aching pain during prolonged walking.
What are the differences between gonathrosis and arthrosis?
From the point of view of the interpretation of medical terminology, it can be noted that there is no particular fundamental difference in the concepts. Degenerative-dystrophic processes can also be called osteoarthritis, because the essence, manifestations, prevention and even treatment methods are the same.
It is important to note that the concept of “gonarthrosis” is applicable only in a situation where the destruction is localized specifically in the knee, since in translation from Greek. the concept is translated as “knee + arthrosis,” while “arthrosis” and “osteoarthrosis” are applicable to any type of this type of disorder in the human musculoskeletal system.
Causes and mechanism of development of arthrosis
The reasons for the development of the articular degenerative-dystrophic process are diverse. Arthrosis is a disease that begins gradually against the background of congenital structural features of connective tissue, as well as prolonged microtrauma, acute joint injuries and diseases. Almost all chronic inflammatory processes (arthritis) eventually turn into degenerative-dystrophic ones with periodic relapses of inflammation. Finally, the largest group of arthrosis is age-related.
Factors predisposing to the development and progression of this pathological process are:
- sedentary lifestyle;
- heavy professional or sports physical activity;
- professions that involve standing for long periods of time without moving;
- excess weight;
- endocrine diseases and hormonal disorders leading to circulatory and metabolic disorders: diabetes mellitus, atherosclerosis, thyroid disease, obesity;
- venous insufficiency;
- poor irregular diet, bad habits (smoking, alcohol abuse) - increase metabolic disorders;
- hereditary predisposition to diseases of the musculoskeletal system.
Under the influence of all these reasons, the cartilage cells covering the articular surfaces of the bones begin to gradually deteriorate. The cartilage first thins, loses its elasticity, and then cracks. The subchondral bone tissue begins to rub against the same dilapidated bone surface on the other side of the joint and collapse. The reaction of bone tissue to this process is its growth, especially at the edges of the joint, which leads to limited mobility and joint deformation.
Joint deformity due to arthrosis
A feature of articular tissue cells is the ability to respond to any, even minor, injuries. Destroyed cells produce pro-inflammatory (causing and supporting the inflammatory process) cytokines. Therefore, the destruction of cartilage and bones is accompanied by an aseptic inflammatory process in the synovium (synovitis) and the effusion of inflammatory fluid into the joint cavity. Periodically developing inflammation contributes to even more active death of hard tissue cells and progression of the disease.
The process is long, at first it does not manifest itself in any way, since the cartilage tissue does not contain nerve endings, so patients do not experience pain in the early stages. They appear when the periosteum located under the cartilage is injured and during exacerbation of inflammatory processes (the periosteum and synovial membrane are very well innervated).
Arthrosis that develops against the background of chronic inflammatory processes is more severe. Complete destruction of articular tissues occurs with the formation of ankylosis (immobility) and disability. Age-related disorders are not so aggressive and rarely lead to severe disorders.
At risk are women over 50 years of age, men over 40 years of age, persons suffering from endocrine pathology and chronic arthritis, as well as persons engaged in heavy physical labor, professions involving prolonged standing, athletes (weightlifters and those involved in traumatic sports) . For these individuals, prevention of arthrosis is of particular importance.
Pathogenesis of gonarthrosis of the knee joint
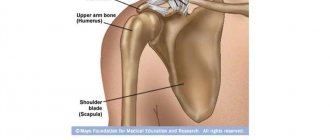
The knee is a joint, a complex bone joint, protected in front by the patella, which normally moves freely in physiological directions when moving, absorbing movement.
The contacting bone surfaces are covered with smooth cartilage, which in normal condition reaches a thickness of 6 mm. With its help, friction arising from knee movements is significantly reduced and shock absorption is provided when performing jumps and other types of impact loads.
The pathogenesis of gonarthrosis involves the gradual destruction of cartilage, which is caused by impaired circulation, leading to the loss of the smoothness it needs. As the disease progresses, it provokes the occurrence of compensatory changes, which is expressed in the growth of bone tissue and deforms the joint.
The progression of pathology with the lack of treatment certainly leads to the fact that the bones are severely deformed and create conditions for loss of mobility due to a significant lack of cartilage.
Are surgeries performed for uncoarthrosis?
Surgical intervention for uncoarthrosis is practiced extremely rarely, only if the disease threatens the patient’s life. Another indication is that the disease progresses too quickly, which leads to serious problems in the body. As a rule, if treatment is started on time, complications can be avoided using conservative methods.
Traditional methods bring temporary relief: the disease can progress dramatically
What is the danger?
Gonarthrosis of the knee joint can be classified as a disease that can be described as a “time bomb”. The disease is characterized by insidiousness, which sooner or later leads to serious health problems.
The gradual development of the pathology makes its timely diagnosis difficult. In the initial stages, a person suffers exclusively from dull pain, which can be confused with severe fatigue. Only after a certain period of time does the pain intensify, which indicates the progression of the disease.
An advanced form can cause not only constant pain, but also a change in gait and visually noticeable deformity.
The main danger of developing the disease is the likelihood of being deprived of the ability to move independently.
What restrictions may be imposed?
If there is deforming gonarthrosis (regardless of the degree of the disease), the young man is subject to lifelong exemption from conscription. If a conscript only has a thinning meniscus, he may be given a temporary deferment from the army for 6 months. In this case, it is necessary that the width of the gap be no more than 0.44 cm. After completing the rehabilitation period, the young man must again undergo the appropriate commission.
If a young man subject to conscription has coxarthrosis, deformation of the hip joint is observed. When such a disease occurs, the following symptoms may occur:
- change in gait;
- the occurrence of sharp pain.
In case of severe deformation of the joint, in which the size of the gap is less than 0.2 cm, the young person has the right to be assigned category “D”.
Important! A young man suffering from uncovertebral arthrosis is also exempt from the army with the assignment of category “D”.
With flat feet of 3 and 4 degrees, degeneration of the corresponding foot joint is observed. In this case, the conscript is assigned category “B”. With a more advanced form of the disease, the young man can count on receiving category “D”.
If you experience pain when walking or exercising, it is recommended to undergo a thorough examination. If necessary, an x-ray examination should be done. With the resulting image, it is recommended to go for a consultation with an orthopedist or surgeon.
Gonarthrosis in the international classification of diseases (ICD-10)
ICD-10 defines codes from M17.0 to M17.9. What does this mean? Let's try to figure it out.
ICD-10 is the most important document of global significance, which is being developed by specialists from the World Health Organization (WHO), which allows us to form an excellent basis for solving global medical aspects.
The code M17.0-M17.9 is a kind of cipher:
- letter – disease class;
- numbers – the disease (the first two) and its type, with clarification of the features (the last one).
The ordered classification allows doctors around the world to be guided by existing standards when making a diagnosis and to maintain more accurate morbidity statistics.
Decoding the M17.0-M17.9 code is quite simple:
M
– disease of the musculoskeletal system and connective tissues;
17
– gonarthrosis or arthrosis of the knee joint;
0-9
– type of disease, its location and nature of origin.
Do people with gonarthrosis join the army?
Often, patients of military age have a completely logical question: are they called up for service with a pathology of this type?
To clarify such a complex situation, it is important to understand that pathology is taken into account when passing a medical commission, however, the verdict on the “suitability” of a conscript is formed taking into account such criteria as:
- the severity of existing symptoms;
- degree of deformation;
- presence of concomitant diseases.
Suitability for service is determined by a military medical commission exclusively on an individual basis, based on instrumental and laboratory tests.
Suitability categories
During the military medical commission, the conscript is assigned one of the fitness categories:
- A – fit;
- B – suitable with minor restrictions;
- B – limited availability (not called up in peacetime);
- G – temporarily fit (assigned until the end of the recovery period for conscripts who have undergone surgery);
- D – not subject to conscription.
Read more about how categories of military fitness are determined here.
Causes of gonarthrosis
Everyone knows that any disease occurs in accordance with certain reasons that give rise to its progression.
A large number of diseases of the musculoskeletal system are characterized by a combination of unfavorable factors, which simultaneously act as causes of gonarthrosis, conditionally divided into groups:
- caused by a violation of tissue integrity (trauma, surgery, etc.);
- caused by constant trauma (excess weight, specific activity, characteristic diseases, etc.);
- associated with structural features (dysplasia, autoimmune disorders, etc.);
- based on metabolic disorders (diabetes mellitus, pregnancy, menopause, etc.).
It is important to note that there is also a hereditary factor. If one of the parents or close relatives had a history of a similar illness, then the chance of its development is much higher.
How to detect uncoarthrosis
Very often, the first manifestations of the disease are attributed to fatigue or hypothermia. Meanwhile, you should pay attention to short-term piercing pains that occur when you turn your head. If left unattended, other symptoms will appear in the near future:
- headache;
- dizziness;
- pressure surges;
- constant fatigue;
- vision problems;
- nausea.
Do you experience discomfort when turning your head? See a specialist
Key symptoms of gonarthrosis
When making movements with your knee, do you hear uncharacteristic sounds? After walking or waking up, does your leg begin to bother you with aching pain or stiffness? It's time to sound the alarm, because all this may indicate the development of a serious illness.
If you close your eyes to existing difficulties and do not pay attention to the existing problem, the source of all unpleasant sensations can develop into a real problem.
Symptoms of gonarthrosis appear gradually as the disease progresses. In the initial stages, the patient may complain exclusively of discomfort and pain, which intensifies after a long walk or climbing stairs. All manifestations disappear after a short rest. Additionally, weakness in the lower extremities may occur.
With increasing deformation, the symptoms become much brighter and become persistent.
In addition to discomfort and pain, symptoms include:
- feeling of stiffness, inability to fully move a limb;
- the presence of slight swelling, synovitis (inflammation);
- crunching sound when performing movements;
- gradual, but noticeable deformation, the severity of which increases with the progression of the disease.
It is worth noting that symptoms may appear with varying intensity, which may indicate the degree of development of the disease.
Arthrosis of the talonavicular joint
The pathology is mainly recorded in young men with flat feet. Other causes of the disease include foot injuries, congenital anomalies and inflammatory processes. The affected area becomes inflamed and swollen, pain appears, the pain intensifies when bending the leg or while walking.
The examination of the disease is carried out according to Article 68 of the Schedule of Diseases. Young people with post-traumatic deformation of the calcaneus, accompanied by a decrease in the Beler protrusion to 10 degrees and arthrosis of the joints, are exempt from conscription. If such an anatomical disorder is detected, the conscript is assigned category G (temporary exemption from military service). The diagnosis of arthrosis of the talocaleonavicular joint is confirmed by CT scanning and radiography.
Provocateurs of the development of gonarthrosis of the knee joint
If a person leads a healthy lifestyle, tries to maintain an optimal level of activity and has good general health status, problems with the functioning of the joints may not overtake him even in old age. If the situation is the opposite, then difficulties with ODA can arise even in youth.
The onset of degenerative changes that rapidly destroy the most important joint components can appear at absolutely any age, for which there are a number of negative factors, the most common of which are:
- joint abnormalities;
- consequences of previous injuries;
- HMS (joint hypermobility);
- diseases of the musculoskeletal system;
- metabolic disorders;
- local inflammation;
- obesity;
- lack of physical activity;
- increased loads;
- pathologies of the cardiovascular system.
Natural physiological changes are not usually considered a paradox, because normally they develop quite slowly.
Classification of gonarthrosis
Gonarthrosis is usually classified according to two factors:
- by etiology;
- by localization.
Depending on the origin of the disease, it is customary to distinguish:
- primary – occurs mainly in older people, especially in those who are overweight;
- secondary – progresses against the background of a previous injury, and can manifest itself as a complication of an infectious disease.
Taking into account localization, three types are determined:
- right-sided - located in the right limb, the risk of development is higher in people who expose the lower limbs to excessive loads of varying intensity;
- left-sided - the lesion is concentrated on the left leg and occurs mainly in middle age with excess weight;
- bilateral - occurs on both legs at once, mainly in severe form and most often causes disability. Most common in older people.
Other types
Simply saying, for example, “rheumatoid arthrosis of the ankle” is not enough. The diagnosis must fully characterize the clinical picture, therefore other types of arthrosis are also used for a medical conclusion.
Localized and generalized arthrosis
When the disease affects only one joint, the disease will be localized. If arthrosis affects several joints (for example, fingers, hip joints, spine), it is polyarthrosis (otherwise, generalized arthrosis).
Primary and secondary arthrosis
Osteoarthritis can be primary (otherwise idiopathic) and secondary. The cause of primary deforming arthrosis is genetic factors. The most significant causes of secondary osteoarthritis are:
- Biomechanical:
- pathologies of development of the musculoskeletal system;
- highly intense loads, especially shock and torsion;
- joint injuries;
- disruption of the structure and nutrition of bone tissue with subsequent necrosis;
- obesity (weight creates additional stress on the joints);
- kyphosis, lordosis, scoliotic posture.
- Inflammatory:
- hemophilia (bleeding into the joint leads to inflammation and further development of the disease);
- arthritis.
- Metabolic:
- deposition of calcium salts in chondrocalcinosis;
- iron deposition in joints with hemochromatosis;
- deposition of uric acid salts in gout.
- Endocrine:
- hormonal imbalance;
- increased production of growth hormone (acromegaly);
- diabetes;
- insufficient or excessive production of PTH hormones produced by the parathyroid glands (hypo- and hyperparathyroidism).
- Ischemic:
- vascular atherosclerosis and obliterating endarteritis of the lower extremities;
- varicose veins
If you have at least one of the listed reasons and feel pain in the joints of your arms or legs, it is better to consult an orthopedic traumatologist in advance.
Degrees of gonarthrosis
According to current data, it is customary to distinguish 4 degrees of the pathological condition, each of which is characterized by a specific clinical picture. Let's consider the issue in more detail.
Initial degree of gonarthrosis (I)
The symptoms are mild, the disease can be detected exclusively using instrumental diagnostic techniques, thanks to the identification of single osteophytes (bone growths).
There is discomfort when performing movements.
Second degree of gonarthrosis (II)
The severity of symptoms increases, the results of instrumental research methods indicate a narrowing of the joint space. Foci of cartilage destruction become noticeable.
When making movements, the symptoms intensify.
Third degree gonarthrosis (III)
The symptoms are pronounced, the joint is visually deformed. A large number of osteophytes are clearly visible among the tissues, which is caused by a compensatory effect.
Mobility is limited.
Final degree of gonarthrosis (IV)
The manifestation of symptoms is permanent, the cartilage is completely destroyed. The bones have grown greatly, the joint is deformed. There are cases when the bones are fused to each other.
Complete loss of mobility.
Stages of arthrosis
The pathology develops gradually in 4 stages. At stage 1, the disease is not accompanied by a pronounced clinical picture - the patient can sometimes hear a crunching sound in the joint while moving. Pain may occur and resolve on its own.
Arthrosis of the 2nd degree starts the process of deformation - the band of clearing between the joints is reduced and mobility is limited. The pain becomes more pronounced and rarely goes away on its own.
Stage 3 is accompanied by a thinning of the joint tissue by 80% and the disappearance of the joint space. The bone becomes covered with osteophytes. The pain syndrome is relieved with the help of medications.
At stage 4, the cartilage is completely destroyed. Drug therapy is ineffective; surgery is required to replace the joint.
Diagnosis of gonarthrosis
The diagnosis and treatment of the vast majority of diseases localized in the joints is carried out by a rheumatologist or orthopedic traumatologist.
The diagnosis is made taking into account the patient’s existing complaints, data from an objective visual examination and analysis of the results of various types of studies.
Instrumental diagnosis of gonarthrosis
To identify pathology localized in the knee, a professional examination, as well as radiographs in frontal and lateral projections, are often sufficient. Available clinical data in combination with x-ray images make it possible to assess the current picture and determine the disease, in particular, the degree of its progression.
The early stage, characterized by minor tissue changes, is ineffective with instrumental X-ray examination. The best diagnostic solution in this situation is arthroscopy.
Ultrasound examination, due to the impossibility of obtaining a clear image, does not allow the assessment of changes. With an accuracy of up to 85%, detection of changes is possible using magnetic resonance imaging (MRI).
Laboratory diagnosis of gonarthrosis
An excellent addition that makes it possible to clarify the characteristics of the existing pathology is laboratory diagnostics.
Synovial fluid is used for research. Attention is paid to such indicators as the level of phosphorus and calcium (the increased content of microelements confirms diagnostic assumptions).
Objective and subjective symptoms of uncoarthrosis
Pain due to lesions of the bone and cartilage tissue of the cervical spine can be very different, so it is impossible to make a diagnosis based only on the patient’s complaints.
- The pain can be aching, stabbing, throbbing - moderate, weak or strong.
- It may appear in the neck, head or shoulder area.
- The pain syndrome can be short or long, periodic or constant, and can intensify when turning or tilting the head.
Objective symptoms include:
- change in skin color;
- increased dryness or sweating;
- changes in tendon reflexes;
- decreased surface sensitivity, etc.
Upon palpation, the doctor detects spasms of the muscles of the cervical spine. When pressing on the exit points of nerves and areas of arthrosis changes, the patient feels pain, and sometimes a soft crunching sound is heard.
Treatment of gonarthrosis of the knee joint
Treatment of musculoskeletal pathologies is always a labor-intensive and quite lengthy process that requires strict adherence to recommendations and instructions. Specialists such as a traumatologist, rheumatologist, orthopedist, and surgeon can participate in the development of the strategy.
The forecasts are simple, logical and understandable: the earlier therapy is started, the better results can be achieved.
Conservative measures aimed at treating gonarthrosis
Conservative treatment is complex and involves taking medications, as well as a combination of physiotherapeutic and other methods.
Essential Principles
In a situation where the patient’s articular tissue can still be saved, the preferred method of treating gonarthrosis is conservative therapy, based on principles such as:
- conducting active physical activity, in particular, engaging in therapeutic physical education, which helps improve metabolism;
- reduction and control of body weight, relieving the joint from excessive stress;
- control of physical activity, preventing the possibility of the need for the joint to work in an increased impact mode;
- the use of a complex of medications aimed at relieving pain and stimulating the production of joint fluid;
- use of orthopedic structures, shoes;
- prescription of physiotherapy.
Treatment of acute pain
Acute pain requires prompt elimination, regardless of the cause of its occurrence. Excellent helpers in this are medications, including:
- non-steroidal anti-inflammatory drugs (NSAIDs);
- corticosteroids;
- antispasmodics.
One of the most effective drugs in the NSAID group is Artradol, which has proven itself in the treatment of patients of varying severity.
IMPORTANT! The exact list of medications, their dosage and other features of administration are determined by the attending physician on an individual basis.
Maintenance therapy
After relieving acute pain, it is important to quickly begin to stop the destructive processes, while simultaneously stimulating regeneration.
The following groups of drugs are prescribed as maintenance therapy:
- chondroprotectors;
- drugs to improve microcirculation.
In addition to drug therapy, physiotherapeutic options are actively used, for example, exposure to ultrasound or laser, etc.
Massage and, of course, therapeutic physical training will also be an excellent addition to treatment.
Surgical treatment of gonarthrosis
The use of drugs and physiotherapeutic techniques can be effective only in the early stages of the disease. In a situation where knee arthrosis is advanced, surgery is the only option for salvation.
Severe pain, a pronounced impairment of functionality, as well as complete or partial loss of performance and self-care are direct indications for surgery.
In total, several types of surgical intervention are practiced:
- endoprosthesis replacement is the most popular and effective solution, involving complete or partial replacement of the affected joint;
- arthrodesis - the connection of bone tissues with each other in order to eliminate pain and create the possibility of independent movement for the patient;
- corrective osteotomy – artificial redistribution of the load.
It is worth noting that arthrodesis and osteotomy are performed quite rarely, only in cases where endoprosthesis replacement becomes impossible for some reason.
Regardless of the type of operation, based on its results, a set of rehabilitation measures is carried out with the patient. Full recovery can take from several months to six months.
Types of arthrosis by location
Types of arthrosis according to the location of the disease:
- Arthrosis of the hip joint.
- Arthrosis of the knee joint.
- Arthrosis of the temporomandibular joint
- Arthrosis of the clavicle.
- Arthrosis of the shoulder joint.
- Arthrosis of the ankle.
- Arthrosis of the talonavicular joint.
- Arthrosis of the foot joints.
- Arthrosis of the elbow joint.
- Arthrosis of fingers and hands.
- Patellofemoral arthrosis.
- Arthrosis of the wrist joint
- Etc.
Let's take a closer look at each of them.
Osteoarthritis of the hip joint
Arthrosis of the hip joint, otherwise coxarthrosis, develops after 40 in both men and women. Its peculiarity: first one joint gets sick, if the disease is not treated, the second one “tightens up”. The main symptom of arthrosis of the hip joint: pain in the groin, descending along the front and side surfaces to the middle of the thigh. The pain rarely reaches the knee and mid-calf, never to the toes (which often happens with a herniated disc).
The disease progresses quickly:
- At the first stage, the intensity of the pain is low, it quickly goes away during rest. If the walk is long (over 2 km), lameness appears. When climbing stairs, patients experience difficulty due to a decrease in range of motion.
- At the second stage, pain occurs with any stress (starting to walk, sudden change in body position, getting up from a chair), and can be from moderate to significant. It intensifies from tension in the surrounding muscles, often projects to the area of the inguinal fold and radiates (radiates) to the knee. The muscles can no longer relax, they are constantly in good shape. It is difficult to swing to the side and rotate the leg. Habitual actions: putting on socks, tying shoelaces, sitting on an exercise machine with your legs spread wide are difficult. Night pain in the joint does not go away. Patients limp, walk with a cane, and are forced to stop often because the pain intensifies after 500-800 m. The limitation of mobility is reduced by a third, and a crunching sound appears. Patients become disabled group 3.
- The third stage – 1st and 2nd disability groups. The pain in the hip joint is constant, sharply intensifies with movement, which cannot be done without crutches. The leg shortens (flexion contracture). It is interesting that in 1 and 10 patients the leg lengthens. Only rocking movement is possible in the joint; adduction, flexion, and external rotation are impossible. The affected leg turns outward, and when walking the person seems to fall on it. In addition to the pain in the groin, pain in the lower back is added. The muscles atrophy, pain appears near the knee, in the area where the tendons attach, which can be worse than the groin. However, the disease does not spread to the knee, this is not arthrosis of the knee joint, the cause is in the muscles.
If a diagnosis of “arthrosis of the knee joint” is made, but no one has checked the functional functioning of the entire limb, there is a high probability of a medical error and the problem is in the hip joint.
This type of arthrosis is the most severe disease in terms of course and consequences. If left untreated, it will lead to long-term disability and disability.
Osteoarthritis of the knee joint
Osteoarthritis of the knee joint
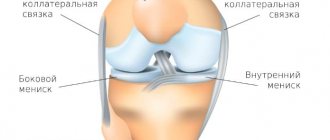
Gonarthrosis, according to statistics, is diagnosed in 8%-20% of patients with arthrosis, develops after 40 years, women are affected more often than men. The disease is more severe with excess body weight and varicose veins.
The main symptom: pain in the knee, which occurs after physical activity, when going up and down stairs, worsens in cold and damp weather. Moreover, the pain does not arise suddenly, in one day, the onset of the disease is a period of many months of mild pain. The knee practically does not change shape, it may be slightly swollen.
Symptoms at stage 2:
- crunching sound when moving;
- inflammation of the inner lining of the joint (synovitis), when there is a lot of pathological fluid formed during inflammation, it may spread to the back surface of the knee and form a Baker cyst;
- decreased range of motion;
- painful palpation in the projection of the joint space and when the patella is displaced;
- increasing deformity of the lower limb.
Attention: gonarthrosis is often confused with damage to the menisci (meniscopathy, develops very quickly), blockade of the knee joint, “referred” pain of coxarthrosis, inflammation of the knee tendons, vascular pain, etc. Contact a specialist to make the correct diagnosis.
If this type of arthrosis is not treated, knee instability, impaired flexion-extension movements in the knee, and varus or valgus deformity appear. The knee hurts all the time, not only when walking.
Crunching in joints - when to worry
Intra-articular injections of hyaluronic acid
Patellofemoral arthrosis
Arthrosis that damages the cartilage tissue, and then the bone of the kneecap and femur, is called patellofemoral (“patella” means “kneecap”). A rare type of arthrosis, but it occurs even in adolescents, because The disease is caused by bruises and injuries to the knee (typical for athletes), compression (prolonged work on the knees of repair workers, tilers). Women, due to weaker muscles and ligaments, get sick more often than men.
The main symptom: pain in the front of the knee, not in the entire joint, which occurs during physical activity, going up and down stairs. A slight crunch and numbness are also noted. If the disease does not affect the remaining parts of the joint, varus (O-shaped) curvature of the tibia and valgus (inward) displacement of the patella are possible in the future. If we compare both limbs, the patient’s kneecap looks inward rather than forward, and the lower leg is more curved in the middle part.
Arthrosis of the ankle
Arthrosis of the ankle joint occurs in obese people and due to problems with the ligamentous apparatus:
- after dislocations and fractures of the foot and ankle;
- fractures of the talus;
- gunshot wounds;
- due to professional chronic injuries (dancers, ballet dancers, athletes);
- with severe deformation of the proximal segments of the limbs.
With a single injury, the ankle recovers in a couple of months, but with repeated injuries, arthrosis begins. Stages of arthrosis of the foot joints:
- The first stage is characterized by swelling and pain in the ankle after normal walking activities and at the end of a working day. Location of pain: anterior surface of the joint, along the line of the joint with transition to the lateral surfaces under the ankles. Sometimes there is a feeling of a “twisted leg.”
- The second stage, there is constant pain, synovitis, crunching when moving, limited mobility.
- The third stage, the joint is deformed, severely swollen along with the distal (lower) part of the leg. Only rocking movements are possible in the ankle.
Arthrosis is accompanied by swelling of the joint, so a frequent misdiagnosis is diseases of the internal organs (diabetes, heart failure, kidney disease). Yes, these diseases can exist, but swelling rises higher: not only to the joint, but also to the lower leg, and often lower, to the foot and toes. And this does not exclude problems with the ankle. Therefore, you need to contact specialists who will examine the ankle using X-rays, conduct a blood test, and perform rheovasography to examine the vessels, and prescribe treatment.
Arthrosis of the talonavicular joint
The talonavicular joint (more precisely, the talocaleonavicular joint) is responsible for the flexion and extension of the foot. Arthrosis in this localization can develop:
- after an injury, severe bruise (martial arts fans: don’t madly hit your foot on a concrete surface);
- foot fracture;
- gunshot wound;
- autoimmune diseases (rheumatoid arthritis);
- necrosis of the bones forming the joint, etc.
The main symptom: pain in the foot followed by limitation of movement. The pain is worse in cold and damp weather. If the disease is not treated, the foot will constantly swell in the upper part, and at stages 2-3 the disease will become deformed.
Arthrosis of the foot joints
Arthrosis of the foot joint
Arthrosis affects not only large joints; small joints of the foot are also affected. Most often, the thumb suffers (“healers” call this gout, explaining the pain as salt deposition). The most common cause is not impacts or injuries, but wearing tight shoes. Along with flat feet, improper shoes lead to illness.
Tight shoes with a narrow toe squeeze the toes, causing the big toe to bend inward and press against the second toe. It's a slow torture for the legs. The finger bone protrudes, rubs against the shoe, and becomes injured. The joint becomes thicker, movement in it is limited. Next, the thumb pushes out the second and third fingers, and bursitis (inflammation of the periarticular bursa) may occur in the joints.
In the initial stage, hallux valgus (and flat feet) can be corrected by giving up tight shoes and performing special physical exercises, regularly using braces, and doing massage. If treatment is neglected, the disease will progress and only surgery can alleviate the condition.
Arthrosis of the clavicle
Arthrosis of the clavicle means:
- arthrosis of the sternoclavicular joint;
- arthrosis of the acromioclavicular joint.
The disease affects the same bone, the collarbone, and the symptoms are similar. This is pain when moving, and then at rest, limited mobility, clicking when moving. Athletes who work with heavy weights and military personnel are at risk (gunshot wounds and injuries can also lead to illness).
In the early stages of arthrosis, injections that reduce pain are widely used - blockade with long-acting glucocorticoids and injections of platelet-rich plasma. Surgical treatment of this type of arthrosis is indicated for severe pain, confirmed by MRI and radiographs.
Arthrosis of the shoulder joint
Arthrosis of the shoulder joint is caused by a severe bruise, dislocation or intra-articular fracture. The disease develops gradually, since the shoulder joint does not experience strong loads compared to the same knee joint. The pain is sharp, it is difficult to bend, abduct or rotate the arm.
Night pain syndrome is noted by all patients, and it is necessary to distinguish between arthrosis in the joint and pain radiating to the upper part of the arm (shoulder) due to heart disease, damage to the periosteal muscle, or osteochondrosis. Arthrosis pain syndrome is aching, pressing, dull, with intensity ranging from weak to very strong, with irradiation to the lower part of the arm.
If you ignore the symptoms and do not consult a doctor, the disease leads to loss of ability to work for a year or more, since during treatment in the final stages the arm is fixed on an abductor splint.
Arthrosis of the elbow joint
Arthrosis affecting the elbow joint develops as a post-traumatic disease. Feature of the disease: in the initial stage, pain is felt not in the joint, but in the lower part of the humerus above the elbow joint (the place of attachment of the tendons to the epicondyles of the humerus), and in extreme positions of flexion-extension of the arm, also in the projection of the ulnar nerve. If the disease is not treated, over time the arm loses mobility at the elbow (flexion contracture develops), first under the influence of muscle pain, then arthrosis.
Arthrosis of the wrist joint
Severe bruises, wounds, fractures of articulating bones are the main causes of arthrosis of the wrist joint. The disease can also be caused by:
- dislocations and subluxations of the hand;
- tunnel syndromes with pinched nerves and poor circulation in the hand;
- Dupuytren's contracture (shortening of the palmar tendons, due to which the palm and fingers do not straighten and bend completely).
If left untreated, pain in the wrist joint due to arthrosis begins to be accompanied by impaired mobility of the fingers and hand.
Arthrosis of the joints of the hand and fingers
Arthrosis of the finger joint
Arthrosis that affects small joints is multiple; if it affects, it is not just one joint, but both hands at the same time. It appears against the background of hormonal imbalance; it often occurs during menopause, and women are much more likely than men. First, nodules appear on the fingers:
- Heberden, located on the joint of the middle and upper phalanges;
- Bushera, located on the joint of the middle and lower phalanges.
The appearance of thickenings in the joints is usually painless, sometimes patients feel a burning sensation in Herberden's nodes and tingling. Next, the joints swell and turn red. After the fluid flows out through the burst skin, the pain subsides. The acute period lasts several months, then the joints become dense, the pain is practically not felt. Over time, deformation and stiffness in the joints increases.
Busher's nodes develop gradually and painlessly, thickening the finger on the sides so that they become spindle-shaped. The joints hurt less throughout all stages, but in the last stage the deformity is clearly severe, the fingers on the hand are knotty.
Another joint susceptible to arthrosis is at the base of the big toe. The disease is called rhizarthrosis (the joint that articulates the metacarpal bone of the thumb and the wrist joint is destroyed) and progresses in those whose profession involves active work with this finger. Main symptoms: stiffness, crunching and moderate pain
The symptoms of this arthrosis are similar to psoriatic arthritis and gout. If you notice swelling or feel severe pain, consult a doctor immediately.
Arthrosis of the temporomandibular joint
Problems in the temporomandibular joint are closely related to psychology. We grind our teeth, clench our jaws, doing unpleasant things through force. Tension in the muscles does not go away, the vessels carrying nutrition to the joint are pinched. Enough chronic stress (along with elevated cortisol levels) and the disease will begin to progress. Other reasons:
- autoimmune diseases;
- endocrine disorders;
- jaw injuries;
- errors in dental decisions.
In addition to pain and crunching in the joint, swelling affects the ear (can lead to hearing loss), the symmetry of the face is disrupted, and dental problems on the part of the joint increase. If arthrosis is not treated, dizziness, insomnia, and headache appear.
Chondroprotectors: what are they, how to choose, how effective are they?
Joint pain at rest
Consequences of lack of treatment for gonarthrosis
Do you think that gonarthrosis is just a periodic crunch in the knee and intermittent pain? “It will go away on its own” won’t work here.
The lack of timely diagnosis, as well as proper treatment, can bring not only emotional decline, torment and loss of the previous level of quality of life, but also:
- visually noticeable deformation of the knee, which not only causes pain, but also belongs to the category of cosmetic defects;
- inability to perform simple actions (flexion/extension of the leg at the knee);
- spread of destructive processes to other parts of the musculoskeletal system (hip, ankle, etc.);
- inability to move independently.
If nothing is done to stop the process, chronic pain syndrome may develop, as well as significant limitation of mobility. With uncontrolled progression, complications such as loss of the ability to walk may occur.
How to prevent all of the above? It's simple: do not ignore the obvious and seek medical help in a timely manner, following all instructions and recommendations.
Approach to treating the disease in our clinic
The Paramita Clinic is an example of a unique approach to the treatment of arthrosis. We use an approach that combines modern European and time-tested Eastern principles of treatment. Taking the best medications for arthrosis is not always a guarantee of results, since the body gets used to the medications. In addition, this approach does not restore energy integrity; problems of interaction between individual systems will remain.
In the clinic, based on the tests, an individual treatment plan is drawn up, physiopuncture and other oriental methods of physiotherapy are prescribed, and traditional drug therapy is also used.
As a result, not only the symptoms of arthrosis are eliminated, the joint restores its functionality, but also a “reboot” occurs:
- general well-being improves;
- metabolism is restored;
- Further destruction of the body due to chronic stress is prevented.
Arthrosis of the joints is a disease that leads to disability. Don't waste time!
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating arthrosis
Literature
- Traumatology and orthopedics. Textbook. Ed. Corresponding member of the Russian Academy of Medical Sciences, prof. N.V. Kornilov
- Traumatology and orthopedics. Textbook for university students. Ed. G.M. Kavalersky
- Evdokimenko P.V. Arthrosis
Themes
Arthrosis, Joints, Pain, Treatment without surgery Date of publication: 10/07/2021 Date of update: 10/08/2021
Reader rating
Rating: 5 / 5 (1)
Prevention of the development of gonarthrosis of the knee joint
Prevention of pathologies is a set of simple recommendations that are incredibly simple to implement.
To maintain healthy joints, you need to follow simple tips such as:
- Systematicity of motor activity. There is no need to strive for records, just walking and simple but well-done exercises in the morning are enough.
- Minimizing stress and getting proper rest. Sleep is the key to health, and controlling emotions and limiting experiences is the basis of quality sleep.
- Balanced nutrition. The daily diet should be optimally rich and healthy.
- Optimal weight. By keeping your weight within normal limits, you can control your load.
- Refusal of uncomfortable clothes and shoes. It is best to give preference to physiological, orthopedic models.
- Attending preventive examinations. It is not superfluous to check the functioning of all body systems, even if you are feeling well.