Pus in a postoperative wound indicates the development of infectious complications. In orthopedics and traumatology, they are difficult to treat and lead to disability of patients. Paraprosthetic infections cause an increase in hospital stay and require costs to combat them.
Discharges from the TBS.
Infections after endoprosthetics can be superficial or deep, acute or chronic, and develop in the early or late postoperative period. The inflammatory process can affect only the soft tissues of the lower limb or spread to the operated joint.
If after endoprosthetics you have pus in your scar, your temperature has risen and you have pain in your leg, go to the doctor immediately. He will examine you, order the necessary tests and find out how serious your condition is. You will have to go to the hospital and undergo a course of treatment.
Relevance of the problem
According to various data, the incidence of early paraprosthetic infection after primary replacement of large joints is 0.3-0.5%, after revision - 9%. Inflammatory processes are detected during the first three weeks after surgery.
An example of a “quiet” seam.
If we talk about the incidence of late infectious complications, they most often occur in the first two years after endoprosthetics (1.63% of patients). Less commonly (in 0.59% of those operated on), deep paraprosthetic infections develop in the next 8 years after surgery.
The frequency of infectious complications has remained unchanged for several decades. However, the total number of arthroplasties has noticeably increased, and the total number of complications has also increased. Therefore, their prevention, early diagnosis and treatment are becoming increasingly important.
Fact! As scientific studies have shown, the risk of developing infectious complications depends on the type of endoprosthesis. It turned out that in total, implantation of domestic models leads to inflammation more often (3-10% of cases) than installation of imported ones (0.3-4.8%).
Symptoms
Manifestations of paraprosthetic infection are in many ways reminiscent of the clinical picture of a classic infectious process, regardless of the place of its origin. In general, symptoms depend on factors such as:
- period of infection:
- the depth of the process.
The superficial type of infection occurs during the recovery period after surgery. In this case, an inflammatory process is observed from the soft tissues without the implanted joint being drawn into it. The manifestations are:
- hyperemia (redness) of the skin in the joint area;
- local (local) swelling;
- increase in local temperature;
- pain;
- disturbances from the wound.
Characteristics of pain:
by localization - in the area of the endoprosthesis;- by distribution - irradiation is limited to neighboring tissues;
- by nature - aching, with the addition of a purulent process - twitching;
- in terms of severity - medium intensity, intensifies with suppuration;
- by occurrence - observed almost immediately from the moment of development of the infectious process.
Wound characteristics:
- may heal slowly;
- the edges often diverge;
- with abscess formation (suppuration), purulent discharge appears;
- in some cases, the formation of areas of superficial necrosis (death) is observed.
A deep form of paraprosthetic infection can develop in the early postoperative period and quite a long time after surgery. It affects the muscles and fascia in the area of the implanted joint. In addition to local signs, which overlap with the signs of the superficial form of the pathology, dysfunction of the limb is observed. There is also a deterioration in the general condition due to intoxication syndrome, which develops due to the involvement of a fairly large array of tissues in the process. Its signs are:
- hyperthermia (increased body temperature). It often reaches 38 degrees Celsius, sometimes higher;
- chills. Its combination with an increase in body temperature is called fever;
- general weakness;
- feeling overwhelmed;
- deterioration in performance.
Deep and superficial processes can develop simultaneously.
note
Paraprosthetic infection can occur with smoothed symptoms.
What is a surgical site infection?
An SSI is an acute or chronic inflammation that develops at the site of an incision or in an area that has been iatrogenic during surgery. In 67% of cases, the infection affects only the surgical incision area, and in 33% it spreads to the implanted joint.
Factors for the development of SSI:
- the duration of the operation is more than 3 hours;
- technical difficulties during surgery;
- intraoperative blood loss more than 1 liter;
- instability of the installed endoprosthesis;
- the use of additional synthetic and biological materials during the operation;
- the presence of severe chronic diseases.
Inflammatory processes that do not spread to the operated joint can be overcome without revision arthroplasty. If the infection affects bone tissue, components of the endoprosthesis, remnants of the joint capsule or other parts of the knee or hip joint, it will be extremely difficult to treat. In this case, the patient will most likely require repeat arthroplasty.
There are a number of factors that aggravate the patient’s condition, slow down recovery and worsen the prognosis: decreased immunity, previous surgeries, frequent treatment with antibiotics. The resistance of the detected microflora to antibacterial agents, poor blood circulation in the joint area, and massive purulent lesions also complicate therapy.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Causes
The immediate cause of the described pathology is pathogenic microorganisms (usually bacteria). Most often, this pathology reveals:
- staphylococci (including Staphylococcus aureus);
- streptococci;
- coli
and some others.
It was revealed that there is a connection between the type of pathogen and the type of prosthesis. This is explained by the biological tendency of pathogenic (and not only) microorganisms to adhesion (stick) to foreign materials that are located in the patient’s tissues. Here are some examples:
- in the area of metal implants or their individual parts, an infectious process most often develops, provoked by Staphylococcus aureus;
- epidermal staphylococcus is activated in the area of polymer implants
and so on.
In addition, factors that contribute to the occurrence of paraprosthetic infection have been identified:
- general features of surgical intervention;
particular features of endoprosthesis implantation;- elderly age;
- a number of severe somatic diseases;
- microcirculation disturbance;
- immunodeficiencies;
- features of drug therapy before surgery;
- human factor.
The most significant factors in the occurrence of paraprosthetic infection are the following general features of surgical intervention:
- the duration of the operation is more than 3 hours - due to the increase in the time of contact of tissues with the infected external environment, the likelihood of their infection increases;
- the body's general reaction to stress, which is any surgical intervention;
- intraoperative complications - for example, bleeding from damaged vessels;
- technical difficulties due to the characteristics of a particular organism.
Particular features of implantation of an endoprosthesis that contribute to the development of paraprosthetic infection include the following:
- the body reacts to a foreign element, which is a joint prosthesis;
- the implant can injure soft tissues, and this facilitates the penetration of pathogenic microflora into them.
note
The older the patient, the higher the risk of paraprosthetic infection. This is due not only to age-related deterioration of immunity, but also to involutive processes in tissues, due to which they gradually lose the ability to recover.
Any severe somatic pathology (current or recently suffered) contributes to the weakening of the body's defenses and the development of paraprosthetic infection. These are serious diseases of any of the body systems:
- cardiovascular – hypertension, atherosclerosis, myocarditis;
- respiratory – pneumonia, pleurisy, bronchial asthma;
- gastrointestinal – peptic ulcer of the stomach and duodenum, cholecystitis, pancreatitis;
- genitourinary – pyelonephritis, glomerulonephritis
and so on.
Impaired microcirculation leads to deterioration in the restoration of tissues affected by microorganisms. It is often observed in vascular and endocrine disorders - as a rule, these are:
- vasculitis - inflammatory damage to the walls of blood vessels with their subsequent disruption;
- diabetes mellitus – carbohydrate metabolism disorders due to insulin deficiency
and so on.
Immunodeficiencies play a direct role in the occurrence of a paraprosthetic reaction - it can develop with the least disruption of the body’s defenses. These are immunodeficiency states:
- congenital;
- acquired.
The deterioration of immunity can also be caused by medical prescriptions in the pre- and postoperative stages - these are:
- blood transfusion;
- drug therapy.
As for the role of specific drug therapy before surgery, long-term use of antibiotics before endoprosthetics can play a pronounced negative role. In this case, the microflora becomes resistant to antibacterial drugs, and their use in the postoperative period to prevent infections is little or completely ineffective.
Important
The human factor that contributes to the development of paraprosthetic infection includes conscious or unconscious violation of doctor’s instructions regarding the regimen of physical activity and rehabilitation measures in the postoperative period.
Types of paraprosthetic infection
In orthopedics and traumatology, several classifications of SSI are used. Systematization and assignment of infection to a specific type helps doctors assess the severity of the patient’s condition. The Coventry-Fitzgerald-Tsukayama classification is the most common.
Table 1. Types of deep paraprosthetic infection according to Coventry-Fitzgerald-Tsukayama.
| Type | Development time | Treatment tactics | |
| I | Acute postoperative | 1st month | Revision of the postoperative wound, removal of necrotic tissue, and, if necessary, replacement of some parts of the endoprosthesis while maintaining its main components. |
| II | Late chronic | From 1 month to 1 year | Mandatory revision endoprosthetics. |
| III | Acute hematogenous | After 1 year | It is entirely justified to try to preserve the installed prosthesis. |
| IV | Positive intraoperative cultures | Asymptomatic bacterial colonization of the implant surface | Conservative treatment consisting of parenteral antibiotic therapy for 6 weeks. |
In the classification created by the Novosibirsk Research Institute of Traumatology and Orthopedics, SSIs are divided into early acute, late acute and chronic. The first develop within three months after endoprosthetics, the second - at 3-12 months, the third - after 1 year. Infectious complications can occur in a latent, fistulous, phlegmon-like or atypical form.
According to the prevalence, infections are epifascial (superficial) and subfascial (deep). May be accompanied by total, femoral or tibial instability.
Prevention
The following actions can prevent the development of paraprosthetic infection:
taking into account indications and contraindications when placing a joint implant;- strict adherence to the principles of asepsis and antisepsis when performing endoprosthetics;
- rational approach to antibiotic therapy;
- elimination of foci of chronic infection in the body;
- the patient’s compliance with all doctor’s instructions regarding activity and rehabilitation measures.
Superficial and deep infections
Occurs in the first month after endoprosthetics. Characterized by the development of inflammation in the soft tissues of the lower limb. The hip or knee joint itself remains intact, that is, it is not involved in the pathological process. The cause of the complication is most often the introduction of pathogenic microorganisms into the wound during surgery or in the postoperative period.
Superficial SSI:
- necrosis of the skin;
- ligature fistulas;
- divergence of wound edges;
- subcutaneous hematoma.
Deep infections:
- necrosis of paraprosthetic tissues;
- deep fistulas;
- infected subfascial hematoma.
Fact! Mild tenderness, local swelling, redness and hyperthermia of the skin in the scar area usually indicate a superficial infection, which can be treated. The appearance of fever, spontaneous dehiscence of sutures and severe pain in the leg suggest inflammation of deep tissues. In this case, the prognosis is less favorable.
Prosthetic joint infections
In pathology, inflammation spreads to the cavities and membranes of the operated joint, remnants of the synovial membrane, bones at the site of fixation of the endoprosthesis and adjacent soft tissues. The cause of the complication is the colonization of joint surfaces by pathogenic microflora. Bacteria can come from the external environment or be introduced hematogenously.
This is what an infection looks like on an x-ray.
Prosthetic joint infections are the most serious complication among all SSIs. They do not respond to conservative therapy, so they have to be treated surgically. Doctors replace the endoprosthesis, but sometimes they still manage to save it.
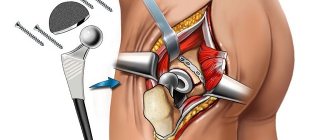
There are three methods for treating infections of a prosthetic joint: wound revision without removing the implant, one-stage revision and two-stage endoprosthetics. The choice of technique depends on the patient’s condition, the time of manifestation of the infection, the stability of the prosthetic components and the nature of the pathogenic microflora.
X-ray studies
X-ray fistulography plays an important role in the differential diagnosis of fistulous forms of infection. With its help, you can determine the size, shape and location of fistulas, identify purulent leaks and their connection with foci of bone destruction. This makes it possible to distinguish superficial from deep SSIs.
Photo: X-ray fistulography, fistula in the lower third of the thigh.
X-rays are most often used to diagnose prosthetic joint infection. The method does not give 100% correct results, but it allows one to suspect pathology. The presence of a paraprosthetic infection is indicated by the sudden appearance of a periosteal reaction and osteolysis. If these signs appear suddenly, soon after a successful operation, there is reason to suspect something is wrong.
Curious! MRI, ultrasound and radioisotope scanning are rarely used for diagnostic purposes due to their low information content. For example, an installed endoprosthesis interferes with magnetic resonance imaging, which makes the image blurry and unclear.
Lab tests
Taking tests helps identify acute and chronic inflammatory processes in the body. An increase in indicators is not a reliable sign of SSI. To make a diagnosis, it is necessary to take into account the presence of certain clinical symptoms, radiographic data and other research methods.
Clinically significant laboratory parameters:
- Leukocyte count. It is important in the diagnosis of acute paraprosthetic infection. A clear sign of inflammation is an increase in the total number of leukocytes and neutrophils, a shift in the leukocyte formula to the left.
- ESR. It is a non-specific indicator. A normal erythrocyte sedimentation rate indicates the absence of inflammatory processes, an increased rate indicates their presence.
- C-reactive protein. CRP is an acute phase protein and a highly sensitive marker of SSI in people who have undergone arthroplasty. When diagnosing paraprosthetic infections, you need to pay attention to this indicator.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Medical Internet conferences
Given the increase in total joint arthroplasty performed annually, the number
complications requiring revision surgery are increasing.
The incidence of PJI varies from 0.6 - 0.9% to 2.0 - 2.4% with general arthroplasty
hip and knee joints [1]. Despite the relatively low
incidence of PJI, the financial burden remains enormous.
Pathogenesis
The attachment of bacteria to the implant is the first step in the pathogenesis of PJI [2]. In
With the increase in total joint arthroplasty performed annually, the number of complications requiring revision surgery is increasing. The incidence of PJI varies from 0.6 - 0.9% to 2.0 - 2.4% in total arthroplasty of the hip and knee joints [1]. Despite the relatively low incidence of PJI, the financial burden remains enormous. Pathogenesis The attachment of bacteria to the implant is the first step in the pathogenesis of PJI [2]. During bacterial adhesion to the implant surface, two distinct phases occur: reversible (nonspecific) and irreversible (specific) attachment. Reversible attachment works based on nonspecific physical and chemical characteristics of bacteria [2]. The biomaterial and surrounding joint fluid also play a role in the reversible adhesion of bacteria to the implant[3]. In contrast, irreversible adhesion depends on more specific structures and receptors. Biofilms play an important role in the pathogenesis of PJI. Attachment of bacteria to a surface involves intercellular adhesion between microorganisms and the artificial surface [3]. Evidence suggests that intracellular entry of staphylococci is a mechanism contributing to the pathogenesis of PJI and treatment resistance. According to this concept, staphylococci can invade and live in host cells, promoting long-term persistence of the microorganism in bone through antibiotic evasion and immune system responses[4]. Most PJIs are caused by gram-positive cocci (Staphylococcus aureus and coagulase-negative Staphylococcus)[5]. In some cases, gram-negative bacteria and fungi can also lead to infection. A significant portion of PJI may be polymicrobial (about 19%). Definition and Manifestations of Periprosthetic Joint Infection According to the proposed criteria, PJI exists when: 1. The pathogen is isolated by culture from at least two separate samples of tissue or fluid obtained from the affected prosthetic joint 2. Four of the following five criteria exist. Increased serum erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) concentration, Increased number of synovial leukocytes, Increased percentage of synovial neutrophils, Presence of pus in the affected joint, Isolation of an organism in one culture of periprosthetic tissue or fluid. PJI may also be present if fewer than four of these criteria are met and clinical suspicion is high [6]. Early PJI (occurring within the first 3 months after initial surgery) typically presents with acute joint pain, wound inflammation (local hyperthermia and flushing), joint effusion, and loss of function [7]. Chronic PJI typically presents with chronic joint pain and prosthetic loosening. Risk factors for PJI: age > 50 years, BMI > 30, type II diabetes mellitus, history of alcoholism and drug addiction. Diagnosis Work on diagnosing PJI begins with systematization with the determination of ESR and CRP due to their high sensitivity and specificity [8]. If these tests are normal, infection is unlikely. Elevated levels of any of these indicators should prompt further investigation in the form of joint aspiration. The combination of serology and aspiration can help the clinician confirm or refute the diagnosis. The combination of serology and joint aspiration is sufficient to diagnose PJI in most cases [8]. Culture of aspirated joint fluid and samples taken during surgery play an important role in the diagnosis of PJI. It is recommended to collect three to five samples from different locations around the prosthesis to increase the likelihood of obtaining a positive culture [9]. Pre-use of antibiotics, slow-growing organisms and the presence of biofilms are some of the factors that negatively affect the sensitivity of culture results [10]. One-stage revision arthroplasty While two-stage exchange arthroplasty is the preferred treatment for PJI, many European centers have long advocated the use of a one-stage procedure, citing reduced morbidity, reduced costs, and comparable results [11]. For a patient to be a candidate for single-stage treatment, the patient must have healthy soft tissue, minimal bone loss, and the causative agent of PJI must be sensitive to antibiotics. Two-stage exchange arthroplasty Treatment of PJI with two-stage exchange arthroplasty has been used for more than four decades [12]. The first stage involves complete resection of all foreign material, clearance of surrounding infected soft tissue, and placement of an antibiotic-impregnated cement spacer. The second stage involves removing the spacer and any additional necrotic tissue, thoroughly irrigating the surgical site, and installing new prosthetic implants. Previously, chronic PJI was mainly treated with a two-stage exchange arthroplasty with a 4-8 week course of intravenous antibiotics between the two stages [13,14]. However, this surgical strategy is currently described as the initial treatment of some acute postoperative or acute hematogenous infections. Specifically, acute infection in immunocompromised patients with highly resistant strains of organisms such as Staphylococcus aureus (MRSA) is best treated with an initial two-step exchange. Additionally, in cases of acute PJI where an initial attempt at more conservative surgical treatment such as irrigation and debridement or one-stage exchange has failed, the use of subsequent two-stage procedures has been indicated [15]. The two-step method is advantageous for several reasons. Spacers not only provide increased joint stability, but also prevent soft tissue contraction and facilitate reimplantation procedures. In addition, cement with an antibiotic provides high bactericidal activity directly at the site of infection, increasing the intra-articular concentration of antibiotics, minimizing the systemic toxic effects of parenteral therapy [14]. An important factor when using cement spacers is the inclusion of specific antibiotics in the cement [16]. The most commonly used combination of antibiotic spacers is powdered tobramycin and vancomycin in polymethyl methacrylate cement. Internationally, a wide variety of antibiotic concentration ratios are used, but as a general rule, no more than 8 g per 40 g of cement should be used to minimize systemic side effects. [15,16]. One of the most controversial aspects of the two-stage exchange procedure today is the decision between the use of static and hinged spacers [17]. Although in certain situations, such as extensive bone loss, the use of hinge spacers is prohibited. Hand-cast static spacers have been shown to limit knee range of motion and functionality between the two stages and may lead to poorer functional outcomes after re-implantation. In some immunocompromised patients who cannot tolerate the reimplantation procedure, definitive treatment ends after resection of the infected prosthesis or even after amputation of the affected limb [15]. For everyone else, a decision must be made when new prostheses should be re-implanted. Unfortunately, to date, no reliable method has been developed to ensure adequate clearance of infection before re-implantation surgery. A study by Kusuma SK, 2011 [18] showed that even the inflammatory markers ESR and CRP, as well as the number and difference of synovial leukocytes, were unreliable in identifying persistent and treated infection. Therefore, the current accepted practice is to administer antibiotics for 4–8 weeks followed by joint aspiration, then stop antibiotics for at least two weeks. The aspirated fluid is then cultured to assess the presence of microorganisms. Long-term oral antibiotic therapy Patients for whom surgery was contraindicated due to various somatic diseases can be prescribed long-term antibiotic therapy without removing the prosthesis. In one study [19], among 18 patients who received only long-term oral therapy without prosthesis removal, 15 were able to maintain functional prosthesis. Conclusion Currently, ESR and CRP are the best available screening tests for PJI. An increase in ESR and CRP in a particular patient requires further research to diagnose PJI. Currently, two-stage exchange arthroplasty is the standard treatment for chronic infection. Under certain conditions (healthy soft tissue, minimal bone loss), one-stage revision arthroplasty is possible.
Microbiological studies
Bacterioscopic and bacteriological studies make it possible to identify and identify the causative agent of infection, as well as determine its sensitivity to antibiotics. Quantitative studies make it possible to determine the number of microbial bodies in purulent discharge.
The following materials can be used for research:
- discharge from a wound;
- fabric samples;
- fluid from the joint cavity;
- prosthetic material.
In case of implant-associated infection, it is almost impossible to detect bacteria in biological fluids and tissues. Pathogenic microorganisms are found on the surfaces of endoprostheses themselves. They cover the implants in the form of an adhesive film.
Fact! In addition to bacteriological examination, PCR (polymerase chain reaction) can be used for diagnosis. The method has high sensitivity but low specificity. Because of this, it often gives false positive results.
Treatment
Before deciding how to deal with the infection, doctors carefully examine the patient. Only after establishing a diagnosis and determining the sensitivity of pathogenic microflora to antibiotics do they make a final decision.
Table 2. Treatment methods for paraprosthetic infections:
| Method | Indications | results |
| Wound sanitation while preserving the endoprosthesis | It is carried out in cases where an SSI occurs in the first 3 months after surgery. It is possible to save the endoprosthesis only in the absence of purulent leaks and severe concomitant diseases. In this case, the implant must be stable, and the microflora must be highly sensitive to antibiotics. | It is the least traumatic treatment method. According to various sources, the effectiveness of surgical debridement is 18-83%. |
| Revision (repeated) endoprosthetics | One-stage or two-stage implant replacement is performed in cases where it is not possible to save the joint. A similar situation is observed with instability of endoprosthesis components, late development of infection, low sensitivity of microflora to antibiotics, and the presence of severe somatic diseases. | Allows you to completely cope with the problem in 73-94% of cases. Unfortunately, during treatment the patient has to completely change the installed endoprosthesis. |
| Arthrodesis with transosseous osteosynthesis | Deep recurrent paraprosthetic infection, microflora insensitive to antibiotics, the presence of severe concomitant pathology. | In 85% of cases, it eliminates the inflammatory process and restores the support ability of the lower limb. |
| Disarticulation in the hip joint | Chronic recurrent inflammation that threatens the patient's life, or complete loss of function of the lower limb. | A man permanently loses his leg. It is cut off at the level of the hip joint. |
Forecast
The prognosis for paraprosthetic infection is generally favorable, but in some cases, regarding the preservation of limb function, it is questionable. Recovery comes:
- during revision of the endoprosthesis - in 18-83% of patients;
- with repeated prosthetics – in 73-94%;
- when performing arthrodesis – in 85%.
Revision of the artificial joint and its reinstallation help preserve the functions of the joint (flexion, extension, etc.); after arthrodesis, such functions are completely lost, but the supporting capabilities are preserved.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
6, total, today
( 52 votes, average: 4.10 out of 5)
Bone panaritium of the thumb
Sacralization of the spine - what is it, consequences and treatment
Related Posts
Implant-sparing tactics
Its main goal is to eliminate the infectious process while preserving the endoprosthesis. The patient undergoes surgical treatment of the wound, during which pus and necrotic tissue are removed. If the joint itself is involved in the pathological process, arthroscopic debridement is performed. The patient is prescribed massive antibacterial therapy.
Curious! Scientific studies have proven the effectiveness of non-surgical treatment of early deep infections. As it turned out, a combination of antibiotics and enzyme preparations helps eliminate inflammation in 5-7 days.