Author
: Grachev Ilya Illarionovich
Editor
: Efremov Mikhail Mikhailovich
Date of publication: 05.13.2014 Date of update: 12.11.2020
There is no universal definition for such a phenomenon as dorsalgia. This term refers to any back pain of nonspecific origin, regardless of the nature and accompanying symptoms. The disease involves benign changes.
Like any ailment associated with the spine, dorsalgia can appear at almost any age. People who have jobs that involve constant physical activity or athletes may be especially susceptible to this phenomenon. The disease can also occur as a result of a back injury.
Any type of dorsalgia has serious complications, so you should not delay treatment.
See how easy it is to cure a disease in 10 sessions
Causes of dorsalgia
All currently known causes of dorsalgia are quite numerous. They can be associated both with direct problems with the spine and signal the presence of other ailments, for example, internal organs. The main factors for the occurrence of the disease are:
- Staying in an uncomfortable position for a long time,
- Muscle strain, physical overload,
- Depression, severe stress,
- Injuries, diseases of internal organs,
- Pathological changes in the spine (with vertebrogenic form),
- Hypothermia and drafts can also cause dorsalgia.
Dorsalgia
Dorsalgia - back pain - is a clinical syndrome caused by many causes. The most common cause of dorsalgia is dystrophic lesions of the spine: osteochondrosis with damage to the intervertebral discs and adjacent surfaces of the vertebral bodies; spondylosis, manifested by arthrosis of the facet and/or facet joints; spondylitis
Along with vertebrogenic causes of back pain, there may be other causes not directly related to the spine.
Vertebrogenic pain in the back and limbs is caused by the following reasons.
- Disc herniation.
- Spondylosis.
- Osteophytes.
- Sacralization or lumbalization.
- Arthrosis of the intervertebral (facet) joints.
- Ankylosing spondylitis.
- Spinal stenosis.
- Instability of the spinal segment with spondylolisthesis.
- Vertebral fractures.
- Osteoporosis.
- Vertebral tumors.
- Ankylosing spondylitis.
- Functional disorders of the spine.
Nonvertebrogenic back pain occurs due to the following reasons.
- Myofascial pain syndrome.
- Psychogenic pain.
- Referred pain in diseases of internal organs.
- Intra- and extramedullary tumors.
- Metastatic lesions.
- Syringomyelia.
- Retroperitoneal tumors.
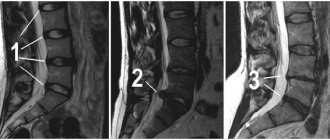
Osteochondrosis of the spine is one of the causes of vertebrogenic dorsalgia. The process is primarily localized in the nucleus pulposus of the intervertebral disc, which becomes less elastic due to loss of moisture. Under the influence of mechanical stress, the nucleus pulposus can sequester and protrude towards the annulus fibrosus of the disc. Over time, cracks form in the annulus fibrosus. A disc with an altered nucleus and fibrous ring can prolapse into the lumen of the spinal canal (disc prolapse), and masses of the nucleus pulposus penetrate through the cracks of the fibrous ring, forming disc herniations. The described processes in one spinal segment lead to reactive changes in adjacent vertebrae and intervertebral joints, resulting in disruption of the kinematics of the entire spinal column. In addition, the process may involve the ligamentum flavum, which becomes denser over time and puts pressure on the root or membranes of the spinal cord. Over the years, stabilization is possible due to disc fibrosis, but a reverse change is never observed.
The development of spinal osteochondrosis and its progression are caused by congenital bone anomalies, excessive physical activity and other reasons that contribute to the wear and tear of cartilage tissue.
Three main pathophysiological mechanisms for the development of dorsalgia have been studied.
- Peripheral sensitization of pain receptors associated with their injury or other pathological effects. In osteochondrosis, these receptors are located in the fibrous ring of the intervertebral disc, the posterior longitudinal ligament, facet and facet joints, spinal roots and paravertebral muscles. Sensitization of these receptors occurs due to trauma to the musculoskeletal tissues of the back, causing the release of pro-inflammatory and algogenic substances (prostaglandins, bradykinin), including mechanisms of peripheral sensitization.
- Damage to nerve structures (nerve, root, intervertebral ganglion) due to various pathological processes (trauma, inflammation, vascular insufficiency). As a result, neuropathic pain develops.
- Central sensitization, which in the first stages is a protective mechanism, and with long-term pain contributes to its intensification.
The processes described above are shown schematically in the figure.
| Drawing. Pathogenetic mechanism of pain chronization |
Depending on which structures of the spinal column are involved in the process in each specific case, either compression or reflex syndromes predominate in the clinical picture.
Compression syndromes develop if altered structures of the spine deform or compress the roots, blood vessels or spinal cord. Reflex vertebrogenic syndromes arise as a result of irritation of various structures of the spine, which has powerful sensory innervation. It is believed that only the bone tissue of the vertebral bodies and the epidural vessels do not contain nociceptive receptors.
Based on localization, vertebrogenic syndromes are distinguished at the cervical, thoracic and lumbosacral levels.
Cervical syndromes. Clinical syndromes of cervical localization are largely determined by the structural features of the cervical spine: there is no disc between CI and CII, CII has a tooth, which in pathological conditions can cause compression of spinal structures. The vertebral artery passes through the transverse processes of the cervical vertebrae. Below the CIII vertebrae are connected using uncovertebral joints, the structures of which can be deformed and serve as a source of compression.
Compression syndromes of the cervical localization. At the cervical level, not only roots and vessels, but also the spinal cord can be subjected to compression. Compression of blood vessels and/or the spinal cord is manifested by a clinical syndrome of complete or, more often, partial transverse lesion of the spinal cord with mixed paresis of the arms and lower spastic paraparesis. Root compression can be clinically divided into:
- root C3 - pain in the corresponding half of the neck;
- root C4 - pain in the area of the shoulder girdle, collarbone. Atrophy of the trapezius, splenius and longissimus muscles of the head and neck; possible cardialgia;
- root C5 - pain in the neck, shoulder girdle, lateral surface of the shoulder, weakness and atrophy of the deltoid muscle;
- root C6 - pain in the neck, scapula, shoulder girdle, radiating along the radial edge of the arm to the thumb, weakness and hypotrophy of the biceps brachii muscle, decreased reflex from the tendon of this muscle;
- root C7 - pain in the neck and scapula, spreading along the outer surface of the forearm to the II and III fingers, weakness and atrophy of the triceps brachii muscle, decreased reflex from its tendon;
- root C8 - pain from the neck spreads along the inner edge of the forearm to the fifth finger of the hand, decreased carporadial reflex.
Cervical reflex syndromes. Clinically manifested by lumbago or chronic pain in the neck area with irradiation to the back of the head and shoulder girdle. On palpation, pain is detected in the area of the facet joints on the affected side. Sensitivity disorders, as a rule, do not occur. It should be noted that the cause of pain in the neck, shoulder girdle, and scapula can be a combination of several factors, for example, reflex pain syndrome due to spinal osteochondrosis in combination with microtraumas of the tissues of the joints, tendons and other structures of the musculoskeletal system. Thus, with glenohumeral periarthrosis, many researchers note in such patients damage to the C5-C6 discs, as well as injury to the shoulder joint, or myocardial infarction, or other diseases that play the role of triggers. Clinically, with glenohumeral periarthritis, pain in the periarticular tissues of the shoulder joint and limitation of movements in it are noted. Only pendulum-like movements of the shoulder in the sagittal plane are possible (frozen shoulder syndrome). The adductor muscles of the shoulder and periarticular tissues are painful on palpation, especially in the area of the coracoid process and the subacromial zone. “Sensory” disorders are not determined, tendon reflexes are preserved, sometimes somewhat animated.
Reflex cervical syndromes include the syndrome of the anterior scalene muscle, which connects the transverse processes of the middle and lower cervical vertebrae with the first rib. When this muscle is involved in the process, pain occurs along the anterior outer surface of the neck, radiating along the ulnar edge of the forearm and hand. When palpating the anterior scalene muscle (at the level of the middle of the sternocleidomastoid muscle, somewhat laterally), its tension is determined, and in the presence of muscle trigger points, pain distribution zones are reproduced in it - shoulder, chest, scapula, hand.
Vertebrogenic neurological complications in the thoracic spine with osteochondrosis are rare, since the bone frame of the chest limits displacement and compression. Pain in the thoracic region more often occurs in inflammatory (including specific) and inflammatory-degenerative diseases (ankylosing spondylitis, spondylitis, etc.).
In medical practice, the first place in terms of treatment is taken by lesions of the lumbar and lumbosacral spine.
Lumbar compression syndromes. Upper lumbar compression syndromes are relatively rare. Compression of the LII root (LI-LII disc) is manifested by pain and loss of sensitivity along the inner and anterior surfaces of the thigh, and decreased knee reflexes. Compression of the LIV root (LII-LIV disc) is manifested by pain along the anterior inner surface of the thigh, decreased strength, followed by atrophy of the quadriceps femoris muscle, and loss of the knee reflex. Compression of the LV root (LIV-LV disc) is a common location. It manifests itself as pain in the lower back with irradiation along the outer surface of the thigh, the anterior surface of the leg, the inner surface of the foot and big toe. Hypotonia and wasting of the tibialis muscle and decreased strength of the dorsal flexors of the thumb are noted. Compression of the SI root (LV-SI disc) is the most common location. It manifests itself as pain in the buttock, radiating along the outer edge of the thigh, lower leg and foot. The strength of the triceps surae muscle decreases, sensitivity in the areas of pain irradiation is impaired, and the Achilles reflex fades.
Lumbar reflex syndromes. Lumbago - acute pain in the lower back (lumbago). Develops after physical activity. Manifests itself with sharp pain in the lumbar region. The antalgic posture and tension of the lumbar muscles are objectively determined. Neurological symptoms of loss of function of the roots or nerves of the lumbosacral region, as a rule, are not detected. Lumbodynia is chronic lower back pain. It manifests itself as dull aching pain in the lower back. Palpation determines the pain of the spinous processes and interspinous ligaments and facet joints (at a distance of 2-2.5 cm from the midline) in the lumbar region, in which movements are limited. Sensory disorders are not defined.
Piriformis syndrome. The piriformis muscle begins at the anterior edge of the upper sacrum and attaches to the inner surface of the greater trochanter of the femur. Its main function is hip abduction. The sciatic nerve passes between the piriformis muscle and the sacrospinous ligament. Therefore, when the piriformis muscle is tense, compression of the nerve is possible, which occurs in some cases with lumbar osteochondrosis. The clinical picture of piriformis muscle syndrome is characterized by sharp pain in the subgluteal region radiating along the posterior surface of the lower limb. Adduction of the hip causes pain (Bonnet test), the Achilles reflex is reduced. The pain syndrome is accompanied by regional autonomic and vasomotor disorders, the severity of which depends on the position of the body - pain and autonomic disorders decrease in the supine position and intensify when walking.
Differential diagnosis of compression and reflex vertebrogenic syndromes. Vertebrogenic compression syndromes are characterized by the following features.
- The pain is localized in the spine, radiating to the limb, right up to the fingers or toes.
- The pain intensifies with movement in the spine, coughing, sneezing, and straining.
- Regional autonomic-vascular disorders, often dependent on body position.
- Symptoms of loss of function of compressed roots are determined: impaired sensitivity, muscle wasting, decreased tendon reflexes.
The following are characteristic of reflex vertebrogenic syndromes:
- The pain is local, dull, deep, without radiating.
- The pain intensifies with load on the spasmed muscle, its deep palpation or stretching.
- There are no symptoms of loss.
Regional autonomic-vascular disorders are not typical.
Treatment of vertebrogenic pain syndromes. In the acute period of the disease, when the pain syndrome is severe, the main task of the doctor is to relieve pain. To successfully complete this task, certain conditions must be met.
- The spine should be kept at rest. To do this, place a shield under the mattress or place the patient on a special orthopedic mattress. For 5-7 days, the motor mode is limited, and the patient is allowed to stand only in an immobilizing belt or corset and only for physiological necessity. The rest of the time, bed rest is indicated. The expansion of the motor regime is carried out carefully; the recommended movements should not cause pain.
- Drug treatment should be structured taking into account all links in the pathogenesis of pain. The source of pain in compression syndromes is pathologically altered structures of the spinal column, which either irritate tissue nociceptors or compress the spinal roots. In reflex syndromes, the source of pain can be both the spine itself and reflexively spasmed muscles that form tunnel syndromes. In addition, with chronic (lasting more than 3 months) or recurrent pain, depressive, anxiety, hypochondriacal and other affective disorders develop. The presence of such disorders must be actively identified and treated, since they have an extremely negative impact on the course of the disease.
- Non-drug treatment is recommended. Physiotherapy, manual therapy, kinesitherapy, etc. are widely used in the treatment of vertebrogenic pain syndromes.
- Surgical intervention is used when conservative treatment is ineffective within 4 months or there are signs of spinal cord compression with dysfunction of the pelvic organs, sensory conduction disorders or damage to the central motor neuron (in the presence of pyramidal signs).
Drug treatment
Analgesics, anti-inflammatory non-steroidal drugs, anesthetics. To relieve pain, the use of analgesics metamizole sodium (Analgin), paracetamol, tramadol (Tramal) and nonsteroidal anti-inflammatory drugs (NSAIDs) enterally and parenterally is indicated. The use of NSAIDs is pathogenetically justified because, in addition to the analgesic effect, they have an anti-inflammatory effect (due to their effect on cyclooxygenase (COX-1 and COX-2), they inhibit the synthesis of prostaglandins, which prevents the sensitization of peripheral nociceptors and the development of neurogenic inflammation).
Among the well-proven drugs in this group, we note diclofenac, which is available in the form of tablets of 50 and 100 mg, rectal suppositories and solutions for parenteral administration. The drug ketorolac (Ketolac) has a powerful analgesic effect, which is recommended to be administered for severe pain syndromes at 30 mg IM for 3-5 days, and then switch to tablet forms, prescribing 10 mg 3 times a day after meals for more than 5 days. In addition to those listed above, you can use other drugs in this group: meloxicam (Movalis), lornoxicam (Xefocam), ketoprofen (Ketonal), etc. But it should be remembered that most NSAIDs are contraindicated for peptic ulcers of the stomach and duodenum, with a tendency to bleeding. If the patient is diagnosed with the above diseases, even in remission, the listed NSAIDs are contraindicated. In such cases, the drugs of choice are selective COX-2 inhibitors, which do not have such a significant effect on the gastrointestinal tract, in particular celecoxib (Celebrex), a selective COX-2 inhibitor. It should be prescribed at a dose of 200 mg 3 times a day after meals for 7-10 days.
To reduce pain, paravertebral blockades can be performed with an anesthetic (Procaine, Lidocaine, etc.) in combination with corticosteroids (50 mg Hydrocortisone, 4 mg Dexamethasone, etc.). Blockades using anesthetics and corticosteroids are recommended to be carried out once every 3 days. In most cases, 3-4 blockades are sufficient for a course of treatment (elimination of acute pain).
Vascular agents. Considering the mandatory participation of the vasomotor component in the pathogenesis of vertebrogenic syndromes, especially those of a compression nature, it is necessary to introduce vasoactive drugs into the treatment complex. The choice of drug depends on the presence of concomitant vascular disease and the severity of vasomotor disorders. In mild cases, oral administration of vasodilators (nicotinic acid preparations or their analogues) is sufficient. If the patient is diagnosed with severe compression radiculopathy, parenteral administration of drugs (Trental) that normalizes both arterial inflow and venous outflow is necessary.
Psychotropic drugs. Patients with chronic pain need correction of affective disorders. To carry out adequate correction of psychoaffective disorders, their diagnosis is necessary (consultation with a psychotherapist or psychodiagnostic testing). In case of predominance of anxiety-depressive and depressive disorders, the prescription of antidepressants is indicated. Preference is given to drugs that have, along with an antidepressant, anxiolytic effect: amitriptyline - from 25 to 75 mg / day for 2-3 months, tianeptine (Coaxil), mianserin (Lerivon), etc. If the patient has predominant hypochondriacal disorders, tricyclic antidepressants should be combined with antipsychotics that do not cause extrapyramidal disorders - tifidazine (Sonapax) - 25-50 mg/day, sulpiride (Eglonil) - 25-50 mg/day.
Non-drug treatment of vertebrogenic pain syndromes. Physiotherapy plays an important role in the treatment of pain syndromes. In the acute period of the disease, preference is given to the use of physical factors that reduce pain, improve regional hemodynamics, especially the outflow of blood from the area of compression, and relieve muscle spasm. At the first stage, diadynamic currents, microwave fields, magnetic therapy, UV irradiation, and acupuncture are used. As the pain subsides, physiotherapy is prescribed to improve tissue trophism and increase range of motion (laser magnetic therapy, massage, phototherapy, kinesitherapy). During the recovery period, it is recommended to actively involve the patient in the treatment process: expand the motor mode, strengthen the muscle corset, etc.
It should be remembered that complete comprehensive treatment of patients with vertebrogenic lesions of the nervous system allows one to achieve complete and long-term remission. During the period of absence of pain, it is necessary to recommend an active lifestyle, physical exercise (without significant vertical and “twisting” loads on the spine), and recreational swimming.
Literature
- Belova A. N., Shepetova O. N. Guidelines for the rehabilitation of patients with movement disorders. M., 1998. P. 221.
- Kukushkin M. L. Pathophysiological mechanisms of pain syndromes. Pain. 2003. No. 1. P. 5-13.
- Podchufarova E.V., Yakhno N.N., Alekseev V.V. et al. Chronic pain syndromes of lumbosacral localization: the significance of structural musculoskeletal disorders and psychological factors // Pain. 2003. No. 1. P. 34-38.
- Shmyrev V.I. Treatment and rehabilitation program for patients with dorsalgia: method. recommendations. M., 1999. 28 p.
- Yakhno N. N., Shtulman D. R. Diseases of the nervous system. T. 1. 2001.
L. G. Turbina , Doctor of Medical Sciences, Professor of MONIKI, Moscow
Types of dorsalgia
At the moment, it is customary to distinguish 2 classic types of the disease, based on the reason for its development:
|
Chronic vertebrogenic dorsalgia
Like any other chronic pain, pain with chronic dorsalgia goes through several stages in its development:
- arising from the primary focus - the site of injury (acute pain), if the cause of acute pain is not treated, the pain receptors continue to be irritated and send continuous impulses to the central nervous system (spinal cord and brain);
- over time, from continuous incoming information, the cells responsible for conducting and analyzing these impulses in the brain become hyperexcitable and undergo restructuring (central sensitization), a secondary focus of pathological impulses is formed and a change in the psycho-emotional perception of pain (subacute and chronic pain).
Chronic pain is considered after 12 weeks (3 months).
Symptoms of dorsalgia
All existing symptoms of dorsalgia are associated with painful sensations in the back, which last for 2-3 weeks and may periodically intensify. Classic symptoms in this case include:
- Feeling of painful discomfort in the spine area.
- Mild pain that worsens during movement or with deep breathing, coughing, sneezing.
- Often, a painful sensation appears after a sudden movement or after physical activity, and then suddenly goes away.
What is POSSIBLE for diseases of the spine
What NOT to do for spinal diseases
Symptoms
Back pain that lasts more than 3 weeks with the presence of functional impairment requires special attention, since it is necessary to identify serious causes of such pain, for example, malignant formations (metastases to bone tissue), inflammatory processes (for example, spondylodiscitis), instability of segments ( e.g. spondylolisthesis) or local compression (spinal or foraminal compression). Typically, serious causes of back pain occur in 5% of cases. The greatest alertness in case of pain for three weeks should be in relation to non-mechanical causes of pain - malignant diseases and infections. Typically, intense back pain at rest is most often a sign of a serious illness (cancer or infection). The presence of serious causes of pain (specific pain) in the back may include the following symptoms (red flags):
- Paroxysmal pain or pain associated with visceral disorders.
- A history of cancer, chronic fatigue, weight loss.
- Fever or immunodeficiency.
- Old age and the presence of osteoporosis.
- Progressive neurological deficit or dysfunction of the pelvic organs.
- Severe stiffness in the morning as the main complaint.
- For nonspecific mechanical back pain, the following red flag symptoms are significant:
- Dissociation between verbal and nonverbal expressions of pain
- Affective description of pain.
- Low pain modulation with prolonged intensity.
- Presence of previous trauma.
- Signs of depression (difficulty falling asleep, waking up earlier, decreased interest in life) and anxiety.
- The need for the use of psychoactive substances
- A history of unsuccessful surgical or conservative treatment.
Treatment methods
Before starting treatment for dorsalgia, it is necessary to find out the exact causes of the disease. For this purpose, the oriental medicine clinic uses muscle and meridian pulse diagnostics, as well as palpation. Then a course of treatment is prescribed, consisting of practice-tested methods of oriental therapy, which are the most effective and truly effective:
- Acupuncture helps eliminate pain and inflammation, eliminate muscle spasms, and relieve swelling.
- Acupressure stimulates complete relaxation of muscle tissue, improved blood circulation, and tissue nutrition. Massage also activates the body's recovery process.
- Manual therapy, in which the disease is treated by stretching the spine, reduces pressure on the intervertebral discs, improves the outflow and flow of blood to the spine. Manual therapy helps release pinched nerves and blood vessels.
- Pharmacopuncture, thanks to microinjections of homeopathic remedies, affects biologically active points on the body, promoting accelerated recovery of the patient.
- Hirudotherapy practices the treatment of sore muscles using leeches.
- PRP therapy is the newest way to stimulate recovery processes. It is used to restore the functions of various organs after diseases and injuries, including to restore the function of the musculoskeletal system during dorsalgia.
We combine proven techniques of the East and innovative methods of Western medicine.
Read more about our unique method of treating dorsalgia
Treatment of dorsalgia at the Paramita clinic
The specialists of our clinic will very quickly help eliminate all painful sensations and provide comprehensive treatment for dorsalgia based on traditional and modern methods of oriental therapy. Procedures are selected individually after a thorough examination of the patient, taking into account the specifics of his disease.
We try not to use surgery or medications. Unique methods of oriental therapy, as well as many years of experience and high qualifications of our doctors will help you forget about diseases such as dorsalgia, as well as general problems with the spine, for a long time.
Sign up for a free initial appointment
Treatment
Bed rest is necessary only for acute radiating pain (for example, sciatica) and should not last more than 1-3 days, as this avoids the progression of a decrease in physical activity and the appearance of pathological behavioral dominants. With all nonspecific myofascial pain, lack of physical activity will have a devastating physiological effect, leading to muscle and other soft tissue wasting, joint hypomobility, decreased muscle strength, and bone demineralization. Therefore, bed rest is generally not recommended. Patients are advised to maintain normal physical activity as much as possible. Bed rest leads to the patient developing a fear of movement and the formation of a pathological behavioral cycle.
Drug treatment is often prescribed for dorsalgia and, moreover, long-term unreasonable prescription of NSAIDs is carried out, which not only do not have a pathogenetic effect, but also cause a lot of side effects. The use of NSAIDs is justified for acute pain and for a short period of time. For dorsalgia (nonspecific pain), central muscle relaxants are also prescribed to relieve muscle spasm. If we are talking about chronic pain syndrome, the prescription of antidepressants is justified, since in chronic pain syndrome the central link of pain sensations is in the foreground. Strong analgesics such as opioids are indicated for pain caused by spinal cancer or serious degenerative changes.
Blockades with the introduction of local anesthetics and steroids are quite effective if there are clear indications for their use (for example, blockades in the area of trigger points or paravertebral blockades).
For dorsalgia, non-drug treatment methods, such as physiotherapy, massage, manual therapy and exercise therapy, have become widely used. The use of a complex of these treatment methods often allows one to achieve good results (stable remission).
Proper nutrition for dorsalgia
Nutrition is a very important factor in the prevention of dorsalgia, since it is the lack of substances necessary for bone and muscle tissue that can become the impetus for the development of negative processes in the body. Basic rules of dietary nutrition:
- Limit salt intake into the body.
- Introduce restrictions on the consumption of smoked and fatty foods.
- Eat meat no more than 2 times a week, if possible replace it with seafood and fish.
- It is recommended to eat jellied meat, jelly, and broths.
- The basis of the diet consists of vegetables and herbs.
- Be sure to include dairy products and eggs in your dishes.
What is chronic dorsalgia?
Dorsalgia (literally translated from Latin dorsum - back, algos from Greek - pain) is a collective concept of back pain of various origins. This diagnosis occurs quite often. According to statistics, up to 80% of people have experienced back pain at least once in their lives; Most people experience back pain occasionally, while for some it is chronic. Chronic nonspecific back pain (chronic dorsalgia) is most often localized in the lumbosacral region and in the back of the neck.
Therapeutic exercises for dorsalgia
To consolidate the effect of treatment, it is necessary to perform a set of simple exercises daily to maintain and strengthen the muscle corset:
- Spread your arms to the sides. Loosen them a little at the elbows for complete relaxation. Slowly move your arms forward, while tilting the entire shoulder area (about 10 times).
- Lying on your back, bend your knees, then straighten them. Slowly move your legs to the sides, perform circular movements.
- Perform circular movements with your head, first clockwise and then counterclockwise.
Dorsalgia of the cervical region
With cervical dorsalgia, compression of the roots, compression of blood vessels, compression of the spinal cord may occur, and may be accompanied by mixed paresis of the arms. The patient complains of pain in the neck, upper shoulder, posterior surface of the shoulder, scapula, and hypotension of the shoulder muscles. The pain can be shooting or chronic. Cervical dorsalgia does not cause sensory impairment. The causes of this type of dorsalgia can be various factors, among them: osteochondrosis, microtrauma of joints and tendons.
Basic information
Dorsalgia is a symptom of various ailments, which are characterized by curvature of the spine, destruction of cartilage or bone tissue, mechanical injuries, etc. Pain appears when nerve endings are pinched, inflammation develops, and physical damage to bones occurs. Moreover, the more intense the pain syndrome, the more damaged the nerve tissue is. If the nerves are located near the spinal column, then the likelihood of pinching the spinal cord increases, and this can lead to serious complications.
Reference. Dorsalgia of the thoracic spine is quite insidious, as it often has a gradual course. This is due to the fact that the thoracic segment is inactive, so the signs of the disorder are less pronounced. For this reason, patients seek medical help late, when the disease becomes chronic.
The main symptom of the syndrome is pain, other symptoms depend on the disease that provoked the disorder.
To diagnose dorsalgia, it is necessary to conduct instrumental as well as laboratory tests. Treatment tactics are drawn up after determining the cause of the disorder. Most often, conservative therapy is performed.
The code for dorsalgia in the international classification of diseases is M 54, and for a syndrome of unspecified origin is M 54.9.
Reference. Dorsopathy is a whole group of pathologies of the spinal column, surrounding muscles, ligaments and other soft tissues. Dorsalgia is one of the types of dorsopathies, which manifests itself as pain.
Treatment of dorsalgia and prognosis for recovery
Did you know that...
Next fact
If a patient has acute back pain, treatment of dorsalgia must be comprehensive. Then the patient is prescribed drug therapy and is recommended to visit a physiotherapy room and exercise therapy room. In some cases, surgery may become necessary.
Drug therapy for dorsalgia involves the use of the following groups of drugs:
| Nonsteroidal anti-inflammatory drugs (NSAIDs) | They play a vital role when the patient has severe pain. For severe pain, they are prescribed as intramuscular injections. For mild or moderate pain, they can be used in the form of tablets or capsules. For greater effectiveness, gels and ointments can be used simultaneously with drugs of this group in tablet form or in injection form. |
|
| Muscle relaxants | Prescribed to relax the back muscles, as well as the smooth muscle fibers of the blood vessels. Drugs in this group help to get rid of pain (sometimes not completely), which allows you to restore the mobility of the spinal column, normal gait and posture. |
|
| Chondroprotectors | They help restore damaged cartilage tissue, but treatment with these drugs should be carried out over several months. |
|
| Glucocorticosteroids | They are used to enhance the effect of drugs from other groups (especially NSAIDs). Helps get rid of pain and swelling of soft tissues. Glucocorticosteroids help restore physiological processes in the body. |
|
| Angioprotectors | Prescribed to improve metabolism between blood and body tissues, improve the patency of blood vessels. Allows you to get rid of swelling of soft tissues. |
|
| Biostimulants | They are prescribed to stimulate metabolic processes in the body, improve blood circulation and transmit nerve impulses. Helps speed up the restoration of body tissues. Strengthen the body's resistance to diseases. |
|
| Vitamins | Vitamin complexes help strengthen the body, slow down the progression of the disease, accelerate the exchange between blood and body tissues, and stimulate the restoration of damaged tissues. For dorsalgia, vitamin B complexes (B1, B2, B6, B12) are needed. |
|
Attention! Nonsteroidal anti-inflammatory drugs are not recommended for use for treatment longer than 5-7 days. Drugs in this group can cause complications, in particular diseases of the gastrointestinal tract.
It is recommended to visit the physiotherapy office after the symptoms of dorsalgia subside - the pain syndrome disappears, tissue swelling disappears, and the inflammatory process decreases.
Physiotherapy for dorsalgia involves the use of the following treatment methods:
- apitherapy (use of bee venom and bee products in treatment);
- acupuncture;
- magnetic therapy;
- manual therapy;
- electrophoresis.
In most cases, massage and manual therapy are used to treat back pain. Manual therapy . But massage should only be performed by a qualified specialist.
During the massage, the chiropractor acts on the deep subcutaneous layers, improving blood circulation in the muscular corset of the back and returning displaced elements of the spinal column to their places.
Exercise therapy is also effective for the treatment of dorsalgia . A set of exercises is selected by a physical therapy instructor individually for each patient, taking into account the cause of back pain.
It is recommended to exercise under the supervision of a specialist so as not to worsen your health through improper exercise or excessive stress on the back.
Surgical intervention is used extremely rarely - in cases where complex therapy does not give a positive result. In some cases, vertebroplasty is used - a gentle surgical method that allows you to strengthen the elements of the spinal column percutaneously, using special equipment and medical cement.
At home, only exercise therapy can be used to treat dorsalgia. Other methods are cold or hot compresses, wrapping, heating, tinctures, etc. can only worsen your health if the exact cause of the pain is not established.
In 90% of cases, dorsalgia and the underlying disease that caused the pain syndrome are successfully treated . In 5% of cases, back pain can be accompanied by complications and treatment can take about 3 months. In only 2% of cases, surgery may be necessary to treat dorsalgia.
Video: “Exercises for the spine for osteochondrosis”
What is lumbodynia
Pain with lumbodynia can be chronic or acute/subacute, but in any case it is caused by spinal pathology. Lumbodynia syndrome is considered a sign of osteochondrosis of the lumbar spine, although often with this diagnosis there may be no pain at all. The severity of pain can vary and depends on the individual and a combination of a number of factors. It occurs mainly in people of working age (25-45 years).
Lumbar pain can be localized only on one side or on both (right-sided, left-sided, symmetrical). It most often worries in the lower lumbar region and can radiate to the gluteal region (one or both buttocks).
Risk factors, causes
Dorsopathy can occur for several reasons.
Some of them:
- Sedentary lifestyle;
Pay attention to the risk factors for dorsopathy. Poor nutrition. Abuse of fats, especially trans fats, leads to their accumulation and the appearance of unpleasant, painful sensations;- Spinal tumors. As the tumor progresses, it begins to cause pain and put pressure on the intervertebral discs, which in turn can pinch nerve endings, which leads to severe pain;
- Spinal injuries. If not treated in time, the damage becomes chronic;
- Infections;
- Smoking tobacco. When smoking, the blood circulation process is disrupted. Intervertebral discs and cartilage tissue do not fully receive the substances they need, and inflammatory processes begin;
- Curvature of the spinal column – scoliosis, kyphosis, lordosis.
People engaged in heavy physical labor and athletes of strength sports need to pay close attention to the health of the spine. Elderly people, due to the aging of the body, are at risk.
If several people in a family have diseases associated with spinal column deformation, then the risk of the disease appearing and developing in a healthy family member increases.
Constant exposure to cold and places with high humidity increases the risk of developing dorsopathy.
Consequences
Diagnosis at a late stage or lack of treatment can lead to serious consequences.
The pain will become stronger, become chronic , and degenerative processes will occur with greater force. a slight numbness of the limbs may occur , and then lead to complete numbness and incapacity of the patient.
In severe cases, only surgical intervention can help.
Characteristics of dorsalgia and its types
Depending on the cause of its occurrence, dorsalgia is divided into:
- vertebrogenic - occurs due to pathological changes in the components of the spine, which are accompanied by an inflammatory process, are a consequence of trauma to the spinal column, or are neoplastic in nature (malignant tumors);
- nonvertebrogenic – occurs against the background of muscle strains, prolonged stress and other psychogenic factors, as a result of muscle spasms and prolonged tension in the back muscles.
Depending on the causes of dorsalgia, the pain syndrome can be vertebrogenic and non-vertebrogenic
Based on the location of painful sensations, the following types of pain syndrome are determined::
- cervicalgia – pain in the cervical spine;
- Thoracalgia – pain in the thoracic spine;
- lumbodynia - pain in the lumbar spine.
Dorsalgia can be combined and simultaneously affect two or three parts of the spine.
Causes
Back pain can appear for various reasons; for convenience, predisposing factors are divided into groups: 1. Pathologies of the spine:
Pain in the lumbar spine
- osteomyelitis is a purulent-necrotic disease that affects bone, bone marrow, and surrounding tissues;
- osteochondrosis, which is complicated by intervertebral hernia;
- osteoporosis – decreased bone density, increased fragility;
- spondylolisthesis – displacement of the vertebrae relative to each other.
- curvature of the spinal column;
- spondyloarthrosis is a pathology characterized by damage to all components of the bone joint, especially the cartilaginous lining;
- tuberculosis of bone tissue - progressive destruction of bones;
- protrusion – protrusion of the nucleus pulposus of the intervertebral disc without rupture of the outer shell;
- spinal canal stenosis;
- fractures and other bone injuries.
One of the causes of dorsalgia is osteoporosis, which increases bone fragility
Reference. Spondylogenic dorsalgia is usually diagnosed with degenerative disorders of the spine.
2. Muscle disease:
- fibromyalgia – musculoskeletal pain;
- Crick;
- inflammation of skeletal muscles;
- involuntary muscle contraction.
3. Other reasons:
- bleeding of the pelvic organs;
- purulent hematomas in the retroperitoneal space;
- diseases of the digestive organs, kidneys;
- dissecting aortic aneurysm - rupture of the largest artery and its further dissection with escaping blood;
- shingles;
- rheumatological diseases.
Important. The likelihood of dorsalgia increases with massive injuries, lifting heavy objects, prolonged exposure to an uncomfortable position, and frequent hypothermia. In women, the disorder may appear during pregnancy or menstruation. Dorsalgia often occurs in patients with psychological disorders (frequent depression, anxiety).
No ads 1
Symptoms of pathology
Dorsalgia rarely occurs on its own. Most often it is accompanied by symptoms of the pathologies that caused it. For example, with urogenital diseases, nagging pain is felt in the lower abdomen and spreads to the thighs and buttocks. And with cervical osteochondrosis, dorsalgia is accompanied by visual and hearing disorders, and dizziness. The development of which diseases is indicated by the combination of dorsalgia with other specific signs:
- reactive arthritis, psoriatic, rheumatoid - skin redness, swelling, increased local temperature, stiffness;
- spondyloarthrosis, osteochondrosis - morning stiffness of movements, crunching, clicking, crackling when bending or turning the body or head.
If dorsalgia is provoked by an infectious lesion of the spine, then symptoms of general intoxication of the body often occur. These are increased body temperature, chills, and excessive sweating.
Treatment and prevention
To plan the most appropriate and effective treatment, doctors must know exactly the causes of dorsalgia. In fact, there are many strategies and methods for relieving back pain, but it is necessary to specifically intervene in the factors that caused it. Unfortunately, not all pathological conditions at the onset of dorsalgia can be cured, since they are degenerative, but they can be kept under control or significantly alleviated.
As mentioned above, the central nervous system is involved in maintaining chronic pain, and in some cases, in addition to treatment by a vertebroneurologist, consultation with a psychiatrist/psychotherapist is required to achieve a positive treatment result.
To reduce the duration and frequency of painful episodes, the following should be observed:
- if you have a sedentary job, try to do a short warm-up at least once an hour, walk around the office, stretch;
- you need to reconsider the organization of your workspace: move the trash can to such a distance that you have to get up to throw out garbage; place stationery items on your desk beyond arm's length so that you have to reach for them; correctly position the monitor directly in front of you so that your eyes are at the same level with it and you do not need to turn your head and body; You can place a small pillow on the chair to create support for the lower back and relieve it;
- avoid overload and too sudden movements;
- try to maintain correct posture;
- watch your weight;
- Take regular walks - this is good for the spine and helps reduce stress levels.
- dosed exercise is safe and beneficial for your back.