The relevance of hyaluronic acid injections into the knee and other joints
Joint diseases are widespread among people around the globe. Recently, there has been a tendency towards an increase in the incidence of this group of pathologies, as well as its “rejuvenation”.
This is due to many factors, in particular:
- deterioration of the environmental situation, and, as a consequence, disruption of bone mineralization and other metabolic processes in all human tissues;
- an increase in average life expectancy, which, of course, leads to an increase in the number of diseases in older people, which include degenerative joint pathologies;
- obesity is a problem that is increasing in scale and causing increased stress on the joints;
- hormonal changes in the body of both men and women are associated not only with age-related changes in the body, but also, often in our time, with the use and receipt of hormonal and other drugs with food that change a person’s hormonal profile;
- receiving specific sports loads, and for professional athletes they are often excessive and lead to injuries, and for amateurs they are unsystematic and often without observing safety precautions, which ultimately also leads to injuries;
- a sedentary lifestyle is becoming more and more common; muscle weakness progresses over the years and, as a result, the risk of joint injury increases;
- an increase in the number of people with genetic and immune diseases who have various disorders of the structure and function of joints as a symptom;
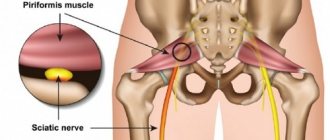
The joint has a complex structure, and disruption of at least one of its elements leads, over time, to the spread of the problem to all its structures. That is why the relevance of new solutions is growing not only in surgical traumatology and orthopedics, but also in the means of conservative treatment of joints. These agents include hyaluronic acid, which is part of the synovial fluid and is an important component of articular cartilage, contributing to its elasticity.
Principle of the method
The PRP method in the treatment of knee joints is based on enhancing the regeneration of intra-articular tissues. Thanks to platelet-rich plasma, cartilage, menisci, ligaments and other tissues are restored faster.
Even in ancient times, doctors drew attention to the fact that traumatic injuries accompanied by the formation of a hematoma heal much faster. The reasons for this have been established only in recent decades. It turned out that platelets secrete a number of substances that accelerate regeneration. These are the growth factors:
- epidermal;
- epithelial growth;
- endothelium;
- fibroblasts;
- insulin-like;
- transformative.
These substances have a polypeptide (protein) structure. They have different purposes. But all of these compounds take part in tissue regeneration. They stimulate the mitotic activity of cells, accelerate their growth and division.
Plasmolifting (PRP therapy) of the knee joint makes it possible to significantly increase the intensity of reparative processes of both soft and bone tissues. In medicine, platelet-rich plasma is increasingly used. It is used for any injuries: soft tissue damage, muscle and ligament ruptures, bone fractures. All types of tissues regenerate faster if a sufficient number of platelets are present.
Operating principle
When joint pathology occurs, an acute or chronic inflammatory process usually occurs in it. At the same time, the amount of enzymes that destroy hyaluronic acid in the synovial fluid increases, as a result of which its viscous properties decrease. As the disease progresses, when cartilage is destroyed and thinned due to progressive osteoarthritis, hyaluronate production decreases. This also affects the performance of the synovium, which works as a “lubricant” for the joints, promoting their sliding relative to each other, preventing friction and damage, which, in turn, is accompanied by inflammation. Intra-articular injection of hyaluronate helps break this vicious circle, improves the viscoelastic properties of synovial fluid, and protects articular cartilage from destruction.
Indications
Among knee joint diseases, the following diseases and conditions are considered indications for the use of PRP:
Arthrosis of the knee joint or gonarthrosis. A degenerative disease associated with the gradual degradation of articular cartilage. The use of PRP at stages 1-2 can improve regenerative processes in cartilage tissue. Thanks to this effect, a significant slowdown in the development of the pathological process is achieved. With the help of PRP, doctors are able to eliminate many symptoms of arthrosis, delay the need for knee replacement, or even abandon the operation completely if an effective conservative therapy regimen is used, in which PRP is one of the elements.
Injuries. The knee is often injured by athletes. Most often these are ligament ruptures and meniscus damage. Intra-articular fractures occur. If the doctor determines that conservative treatment is sufficient, he or she may use PRP to speed up the healing of the lesions. Otherwise, they can take a very long time to recover. This process takes weeks, or even months.
Operations. After arthroscopic surgery on the knee, a rehabilitation period follows. It continues until all tissue damage is restored. PRP can be used to speed up this process.
Defects of the articular surface. PRP is used for cartilage deficiency of articular surfaces of any origin. The cause may be injuries, arthrosis, inflammatory diseases of the knee, metabolic pathologies, psoriasis, systemic connective tissue lesions and other diseases. With a small defect, it is possible to enhance the regenerative processes of PRP. If there is a significant area of cartilage thinning, surgical treatment is indicated.
The effectiveness of hyaluronic acid in the treatment of joints
Sodium hyaluronate administered intra-articularly is also called synovial fluid prosthesis and acts as follows:
- Protects cartilage from destruction, especially where it is already damaged.
- Stimulates the synthesis of its own hyaluronic acid, the level of which may decrease over time or due to the development of arthrosis.
- Improves the shock-absorbing properties of the joint.
- Helps improve the properties of intra-articular fluid, increases viscoelastic indicators.
- Reduces stiffness, improves gliding of articular surfaces.
- Helps stop the inflammatory process.
Numerous clinical trials have proven the safety of hyaluronic acid preparations. They practically do not cause allergic reactions or side effects.
How many injections need to be given?
The effect of corticosteroids can last from 2 weeks to 3 months. Injections with hyaluronic acid are prescribed taking into account the stage of the musculoskeletal system disease. 1 course consists of 3-5 procedures, which are carried out once a week. In the early stages this is enough. If the joint is very bothersome and arthrosis has already entered the 2-3rd stage, the courses are repeated every 6 months. Names of drugs with hyaluronic acid:
- gialgan;
- hialubrix; (hormones);
- Hyalon.
Injections into the joint are made with a syringe with a very long needle, which should fall exactly into the joint space. The procedure is performed under sterile conditions and under ultrasound control.
After intra-articular injections, it is recommended to limit thermal and water procedures for 24 hours; there are no restrictions on physical activity. Intra-articular injections are a very responsible procedure, which should only be performed by qualified specialists. If you have problems with the hip joint - it has become difficult to walk or perform various movements - contact our center. You will receive competent advice: the doctor will assess the severity of the problem and prescribe a course of treatment procedures, selecting the most suitable drug.
When are hyaluronic acid injections prescribed?
Experts prescribe a course of injections according to indications:
- When the integrity of the articular cartilage is damaged.
- To reduce motor dysfunction.
- For osteoarthritis as one of the methods to prevent the development of the disease.
- For the treatment of pain and reduction of inflammation.
- To normalize the composition of intra-articular fluid after joint surgery, including after arthroscopy.
At the SportClinic, doctors use only high-quality drugs strictly according to indications for injection into large joints (knee, shoulder, elbow, hip, ankle), they have extensive experience in such prescriptions with results of their high effectiveness in complex treatment.
What is this?
PRP is platelet-rich plasma. The patient's own plasma is used during the treatment process. It is prepared from autologous blood immediately before injection into the knee.
Platelets are the formed elements of blood that perform the function of forming a blood clot. By gluing, they initially form a “plug” in damaged vessels. This happens immediately after the injury. Then platelets provide their surface for the formation of the main reactions of plasma blood coagulation.
Not long ago, another important function of platelets was established. It turned out that they secrete a large number of growth factors and take part in regenerative processes.
Normally, the concentration of platelets in the blood ranges from 180 to 360 thousand cells per μl. Even this amount is enough to somewhat speed up the regenerative processes. But they occur faster and more intensely if a lot of platelets are injected into the joint. Therefore, the plasma is pre-prepared. Other formed elements of blood are removed from it. The platelet concentration increases 5 or more times.
It has been established that the maximum regenerative potential of tissues is achieved when they are exposed to plasma containing at least 1 million platelets per 1 μl. Further increases do not provide significant benefits. If the platelet count exceeds 1.8 million, inflammatory reactions may be enhanced. Therefore, too high a concentration of these cells is not recommended for use for intra-articular administration.
After operation
PRP knee therapy is used after ligament and meniscus surgery. There are many studies demonstrating the effectiveness of this procedure for accelerating the recovery of intra-articular structures.
One common area of application remains rupture of the anterior cruciate ligament of the knee. She herself cannot fully recover from a complete rupture. Therefore, to normalize its fusion (ligamentization), surgical treatment is used. Free autografts are used.
There are different types of them. STG (intrinsic tendon) and BTV grafts (“bone-tendon-bone”) are used. In both the first and second cases, the introduction of PRP into the knee allows one to achieve significant positive treatment results.
First of all, PRP is performed to speed up the rehabilitation period. Studies show that when using STG grafts, the ligamentization period is on average 369 days (about 1 year), while the use of PRP reduces this period to 177 days (6 months). That is, the terms are reduced by 2 times.
Even more significant results can be achieved when using PRP therapy for the knee after using a VTV graft to reconstruct the anterior cruciate ligament. The average time for ligamentization is about 1 year. When using PRP it was possible to reduce it to 3.5 months.
Studies demonstrate that ligamentization after surgery is significantly better in patients receiving PRP therapy than in the control group. True, the results are better only 4-6 months after surgery. The examination of patients after 1 year shows that the final results are the same.
However, PRP therapy can significantly reduce the recovery time for patients after surgery. This is especially important for professional athletes who want to return to training as quickly as possible.
Effectiveness for arthrosis
When to expect results depends on the purpose of using PRP and the indications for treatment. In any case, it does not develop instantly. PRP is not a pain reliever. Platelet-rich plasma only enhances tissue regeneration, and this process takes quite a long time.
For arthrosis of the knee joint, the maximum effect develops 3-6 months after the start of treatment. Only a few patients report a decrease in pain after the first injection. For others, the first results are achieved within a month from the start of therapy.
In comparative studies, PRP shows much better results than intra-articular glucocorticoids. These differences are especially noticeable in grade 3 gonarthrosis. Pain syndrome in patients with this method of treatment is less pronounced. In addition, PRP has a more beneficial effect on cartilage - plasma stimulates its regeneration, while glucocorticoids, on the contrary, have a chondrotoxic effect.
According to E.Kon, 80% of people were satisfied with the results of the treatment after a series of injections of platelet-rich plasma for osteochondrosis. Results were assessed after 5 weeks. Another study found that treatment results were rated as positive by 67.3% of patients six months after undergoing PRP therapy for knee arthrosis. In the control group this figure was only 4.3%.
Another study calculated the average amount of time that elapses from the first injection until the therapeutic result is obtained. Patients considered this to be a reduction in clinical symptoms. This period was 17.63 days.
It should be noted that PRP has two main effects: anti-inflammatory and reparative. When surveying patients, only short-term symptomatic effects are taken into account. It develops more quickly after administration of platelet-rich plasma, but goes away more quickly after completion of the course of therapy. The first results of treatment are due to hyperplasia of the synovial membrane and modulation of the level of cytokines in the articular cavity.
At the same time, the main effect of PRP is chondrogenesis. But this process is happening too slowly. Patients cannot feel it. Only by comparing the symptoms and radiological parameters of the main and control groups are researchers able to obtain data on the effectiveness of PRP therapy for the knee joint several months after the course of treatment.
Safety
PRP therapy for the knee joint is one of the safest treatment methods. There is no risk of complications. The exception is the human factor. The doctor may miss the needle into the joint or cause an infection if he does not follow the rules of asepsis and antisepsis.
But if you turn to a highly qualified specialist who has extensive experience in performing this type of medical manipulation, the procedure will go smoothly. If a joint is deformed, if it is difficult for a doctor to get into its cavity, ultrasound can be used. Therefore, there is no risk of damage to healthy tissue during PRP therapy.
The drug itself for injection into the joint cavity is prepared from the patient’s blood. Therefore, the risk of transmission of infection or allergic reactions is eliminated. Your own blood does not carry an antigenic load. It is completely safe.