Symptoms of cervical osteochondrosis in women Symptoms of cervical osteochondrosis in men General symptoms of cervical osteochondrosis Treatment and prevention of symptoms of cervical osteochondrosis
Symptoms of cervical osteochondrosis bother every 2nd person whose age has exceeded 30 years. Young and old are susceptible to this disease, its prevalence is colossal, and its consequences are varied and serious. Untreated cervical osteochondrosis can lead to vertebral artery syndrome, cervical radiculitis, deterioration in hand motor skills, vision, hearing, and serious problems with memory and other cognitive functions.
The disease is especially merciless for urban residents - symptoms of cervical osteochondrosis are observed in them already at the age of 25, earlier than any other diseases of the musculoskeletal system (except, perhaps, autoimmune ones). How to recognize the symptoms of cervical osteochondrosis in time so as not to lose your ability to work long before retirement?
Osteochondrosis - definition and mechanism of development
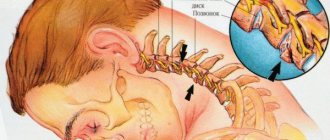
Osteochondrosis is a chronic progressive disease of the spine. During the examination, gradual destruction of cartilage and deformation of bone segments are observed. The cervical spine consists of six vertebrae - bone segments connected by ligaments. For shock absorption during movement, turns and tilts of the head, intervertebral cartilage is located between adjacent vertebrae. Special openings contain vertebral arteries and nerves that go to the brain, and protecting them from damage is one of the functions of the cervical spine.
With osteochondrosis, the cartilage tissue of the intervertebral discs loses its elasticity. Its main reason is insufficient supply of blood and nutrients to the cartilage tissues of the intervertebral discs. This process may be associated with age-related changes, insufficient blood supply to cartilage, as well as the consequences of injuries and inflammatory diseases of the joints. The intervertebral discs become thin and insufficiently elastic, so they cannot absorb shock during movement. This leads to decreased neck mobility, painful sensations, and compression of the nerves and blood vessels that pass through this area. The process progresses because the cervical spine is the most mobile and has a weak muscle corset.
Possible complications and consequences
In the neck area there are many nerve endings and blood vessels that directly affect the functioning of other parts of the body: if cervical osteochondrosis is not treated, it can lead to an increase in many other diseases:
- Migraine – it is in the neck area that the vertebral artery delivers blood to the brain: narrowing also leads to severe headaches.
- Visual impairment - the carotid and vertebral arteries, which are responsible for supplying blood to the visual organs, pass through the neck: compression of the nerve roots and blood vessels leads to decreased vision.
Causes of headaches with cervical osteochondrosis
Cervical osteochondrosis is a common disease among both elderly and young people. It is accompanied by limited mobility of the neck in all or in a certain direction, deterioration of hearing or vision, as well as acute headache. These symptoms appear already at the initial stage of the disease and only progress over time.
Headache with cervical osteochondrosis is associated with a number of pathological changes:
- decreased clearance between adjacent cervical vertebrae;
- compression of nerves and blood vessels that go to the brain;
- insufficient blood supply to brain cells;
- deformation of bone tissue, formation of growths, fusion of vertebrae - a mechanism of adaptation of the body against abrasion of bones during movement.
Headaches with osteochondrosis can only occur when the cervical spine is affected. This area contains arteries and nerves that carry blood to the brain and participate in its innervation. When the thoracic and lumbar regions are affected, pain in the head does not occur. However, the disease is most often diagnosed in this area, since it is the most mobile and the supporting muscle corset is poorly developed. Incorrect posture, prolonged sitting, lack of physical activity, or, conversely, too intense exercise without sufficient warm-up contribute to the rapid development of osteochondrosis at any age.
Stages of development of osteochondrosis
In the development of cervical osteochondrosis, it is customary to distinguish 4 stages. But this is a rather arbitrary division, since most of the symptoms of the disease can also manifest themselves in other pathologies. In addition, the actual degree of tissue degradation of the cervical spine may not correspond to the externally manifested symptoms.
First stage (preclinical)
At the initial stage, symptoms are mild and are often attributed to stress or other diseases. You feel unpleasant stiffness in the neck, pain with sudden movements or bending. At this stage, it is quite possible to get rid of incipient osteochondrosis with the help of therapeutic exercises or simply move more and adjust your diet.
Second stage
The pain intensifies, becomes constant, and becomes severe with sharp turns or bends. Severe headaches appear, the patient begins to get tired quickly, becomes absent-minded, and areas of the face periodically become numb.
Third stage
The formation of disc herniation often causes dizziness, weakness of the arms, pain radiates to the back of the head and arms, and is constantly felt in the shoulders.
Fourth stage
Eventually, the intervertebral discs are destroyed and replaced by connective tissue. The nerves are pinched, which leads to difficulties in movement, acute pain, increased dizziness, and tinnitus.
The nature of pain caused by osteochondrosis
Headaches with osteochondrosis are a symptom by which the disease can be identified even in the absence of any damage to the neck area. However, it is impossible to make a final diagnosis based on examination alone. There are several options for what types of headaches there are with osteochondrosis, depending on the cause of their occurrence:
- when the vertebral artery is compressed, the pain resembles a migraine, often spreading to only one half of the head;
- when the roots of the spinal nerves are pinched - pulsating, sharp, intensified during turns and tilts of the head;
- chronic headaches are associated with ischemia, a lack of oxygen and nutrients in certain areas of the brain.
With osteochondrosis, headache is often accompanied by additional symptoms. The main one is stiffness in the neck, muscle spasm and discomfort. In addition, the patient may experience numbness in his hands and a tingling sensation in the skin of his palms. If there is insufficient blood flow to the brain, hearing and vision deteriorate, and difficulties with coordination of movements appear. There is also increased sensitivity to bright light and loud sounds and tactile stimuli. These signs disappear after blood circulation is restored.
Why is cervical osteochondrosis dangerous?
Many vital vessels, arteries, and capillaries are concentrated in the neck area, so any disturbance there can have unpleasant consequences, including oxygen starvation, hypertension, and vegetative-vascular dystonia.
Cervical osteochondrosis affects the segments of the spine that control the functioning of the shoulder and elbow joints, the thyroid gland, hands and other organs. With osteochondrosis, if left untreated, there is a high probability of pinched nerves and compression of blood vessels, which inevitably affects the functioning of other organs.
Diagnostic methods
Headaches with osteochondrosis of the cervical spine are a symptom for which it is difficult to make an accurate diagnosis. To begin treatment, it is necessary to determine the location of the problem area, the stage of the disease and the pathological changes caused by the disease. To do this, a set of examinations is prescribed, including:
- MRI of the head is one of the most informative and accurate diagnostic methods, thanks to which you can assess the condition of brain tissue;
- MRI of the cervical spine is a simple way to get an accurate picture of all the disorders that appear in this area (thinning and decreased elasticity of the interarticular cartilage, proliferation of the articular surfaces of the bones.
- Dopplerography of the vessels of the neck and head - performed with the addition of a contrast agent to monitor cerebral blood flow and determine areas of the brain that suffer from ischemia.
At the Clinical Brain Institute, you can undergo a full examination, determine the stage of the disease and monitor the dynamics of treatment. For this, only modern techniques and precise equipment are used, which allows us to obtain a detailed image of the area under study in any projection. In addition, experienced specialists will be able to accurately determine the causes and stage of the disease, thanks to which the patient quickly receives competent and effective prescriptions.
Diagnostics
Since the symptoms of osteochondrosis are mild and often overlap with other pathologies, it is better to conduct an initial examination with a therapist or other specialist - a neurologist, orthopedist. He will ask you about pain and other symptoms, check neck mobility, skin condition, balance, and reflexes.
If a primary diagnosis of “cervical osteochondrosis” is made, the doctor will then refer you for additional studies. The most effective of them is MRI, followed by computed tomography. X-ray studies are much less effective than the first two, especially with advanced disease. The condition of soft tissues is checked using ultrasound. If your doctor suspects blood vessel damage, you may be referred for a vascular duplex scan.
Since some symptoms overlap with signs of angina and coronary heart disease, you may need to consult a cardiologist who will refer you for an ECG and echocardiography.
Treatment of headaches with cervical osteochondrosis
Treatment of headaches with cervical osteochondrosis is symptomatic. The attacks can be relieved at home, but they will continue to occur. It is important to understand that osteochondrosis is a chronic, progressive disease, and it is impossible to completely restore the structure of the affected part of the spine. The goal of therapy is to slow down further destruction of the vertebrae, restore normal blood supply and innervation, and also get rid of pain and other unpleasant symptoms.
At the Clinical Brain Institute, individual treatment regimens are selected. They depend on the stage of osteochondrosis, the age of the patient and the characteristics of the course of the disease, as well as on additional symptoms. Most patients are treated at home, but it is important to periodically return for re-examination to track the dynamics of the disease and evaluate the effectiveness of therapy. However, during the period of diagnosis and undergoing a course of procedures, there is the possibility of staying in a hospital.
Drug treatment
Most patients are prescribed a comprehensive treatment regimen for osteochondrosis. You can take a pain reliever at home, but the headache will return. It is important to choose an effective set of medications that will affect not only the symptoms, but also the causes of headaches. Timely initiation of treatment will help maintain the condition of the spine at the same level and prevent further deterioration of well-being.
Doctors can prescribe several types of medications to relieve headaches with cervical osteochondrosis:
- non-hormonal anti-inflammatory drugs - eliminate pain and relieve inflammation in the joints (Nurofen, Solpadein);
- muscle relaxants - a group of drugs that relieve muscle spasms, thereby improving blood circulation in the vertebral artery (Mydocalm);
- vasodilators - necessary for high blood pressure, as well as to eliminate vascular spasm (magnesium sulfate);
- nootropics are an additional category of medications that are selected to improve blood circulation in brain cells.
If your head and neck hurt with osteochondrosis, medications can be prescribed either in the form of tablets or injections, or as an ointment. To improve blood circulation and nourish cartilage, gels with a warming component and anti-inflammatory effect are useful. They stimulate blood circulation and regeneration processes, therefore supporting the condition of the spine during periods of exacerbation of the disease.
Additional techniques
Treatment of headaches due to osteochondrosis includes a number of techniques that strengthen the cervical spine and prevent compression of important nerves and arteries. They represent special exercises for the formation of a muscle corset, as well as physical and other methods of influencing the affected area. They are prescribed in combination with drug therapy and are carried out in a course of several sessions.
- Therapeutic exercises are simple exercises to strengthen muscles and ligaments and increase their elasticity. Warm-up consists of turns and bends, circular movements of the head. Next, you should alternately place your palm on your forehead, temple and back of your head. The head is tilted towards the hand, and the palm offers resistance. At home, you can perform exercises in the morning and evening, devoting at least 20-30 minutes a day to physical exercise.
- Massage is an effective technique that will help relieve severe headaches with osteochondrosis, as well as prevent the progression of the disease. At home, you can do self-massage, which kneads the muscles of the back and sides of the neck, as well as the trapezius muscles. It is useful to attend therapeutic massage sessions, which are carried out in a course of 5–10 procedures. The course is repeated every 4–5 months.
- Physiotherapy is a set of techniques that a doctor can prescribe to improve well-being in case of cervical osteochondrosis. This can be magnetic therapy, electrophoresis, paraffin baths and other methods of influence. Under external influence, blood flows faster to the damaged area, nutrition of damaged intervertebral discs and their oxygen saturation improves. In addition, restoration processes are activated at the cellular level, due to which the disease does not develop further.
Regular exercise, attending massage sessions and physiotherapy will help get rid of severe headaches due to osteochondrosis. The main condition is to complete the full course of procedures. They are carried out at intervals of several days to a week, and up to 10 sessions may be needed to achieve maximum effect. During treatment, ease of movement, absence of headaches and other symptoms, improvement in concentration and performance are noted. However, it is important to remember that osteochondrosis is a chronic disease, so the course of procedures is repeated every 4-6 months.
Surgical treatment of osteochondrosis
Surgery is prescribed only in cases where conservative treatment is ineffective. This occurs in advanced cases, if the patient experiences fusion of adjacent vertebrae or the formation of osteophytes - bone growths on the articular surfaces of bones. These changes lead to constant headaches, neck stiffness, and chronic ischemia of some areas of the brain. The operation can be performed in several ways:
- removal of pathological growths on the surfaces of the vertebrae that prevent them from participating in movement;
- connecting adjacent vertebrae to reduce compression of nerves and blood vessels;
- replacement of the damaged segment with an implant.
The decision regarding surgical intervention is made individually. It is worth understanding that this is a complex operation that will require a long recovery period. In the early stages it is not carried out, since there is no threat to the patient’s health. Doctors at the Clinical Institute of the Brain will be able to choose the optimal method for treating osteochondrosis and headaches caused by these diseases, based on the results of a full examination.
OSTEO-VIT. Vitamins for bone health
Cervical migraine
, which differs from the manifestations of classic migraine, is one of the symptoms of vertebral artery syndrome (impaired blood flow in both or one of the vertebral arteries), resulting in severe headaches similar to migraine attacks.
One of the most common causes of cervical migraine is cervical osteochondrosis,
which is degenerative-dystrophic modifications of the cervical vertebrae (first and second).
Since in the cervical spine there is practically no free space for the passage of nerve trunks and blood arteries that supply the brain, degenerative-dystrophic changes in the cervical vertebrae lead to pinching of the nerve trunks and pressure on the blood vessels, which is often accompanied by characteristic symptoms of cervical migraine
.
There are other causes of cervical migraine
, divided into groups. To cope with a painful headache, treatment for cervical migraine should begin with treatment of the main cause that provoked it.
Causes of cervical migraine.
Causes of cervical migraine
are divided into two groups: not associated with changes in the cervical vertebrae (non-vertebrogenic) and associated with modifications of the vertebrae (vertebrogenic).
The first group includes factors such as the presence of atherosclerotic lesions of blood vessels, congenital pathologies of their structure or features of anatomical location. This group should also include injuries received, most often resulting from car accidents (whiplash injuries), frequent myositis (inflammation of skeletal muscles) or spastic myoclonus of the neck muscles.
The second group of causes of cervical migraine is caused by problems with the cervical vertebrae: abnormal congenital structure of the vertebrae, injuries of the cervical vertebrae, their instability, and, as one of the most common causes of cervical migraine
- cervical osteochondrosis, a process affecting the first and second cervical vertebrae.
There are also possible idiopathic (unclear etiology) causes of cervical migraine
, which also lead to
symptoms of cervical migraine .
Symptoms of cervical migraine.
All causes of cervical migraine
, indicated above, lead to pinching of nerve trunks and compression of the vertebral arteries, which in turn becomes a factor in vasospasms and acute narrowing of vascular clearance, which causes
cervical migraine . Vascular spasms can be either persistent or appear when moving the head or changing body position, which can impair cerebral circulation. The development of cervical migraine
occurs in two stages.
At the initial stage (reversible stage), sporadic vasoconstriction occurs, which is accompanied by outbreaks of headaches with symptoms characteristic of the first stage. At the second (irreversible) stage, the narrowing of the walls of blood vessels increases and the symptoms of cervical migraine
, which become significantly more frequent.
Headache attacks with cervical migraine
can be either episodic or constant, localized mainly in the occipital region, radiating at the time of an attack to the frontal, ear or parietal part of the head, usually on one side, changing when the head position changes.
The pain is pulsating, burning and pulsating (usually coinciding with the heart rhythm), significantly intensifying with any kind of touch, and when turning the head, accompanied by itching and burning. Headache, the etiology of which is cervical migraine , may be accompanied by vomiting and nausea, a feeling of a lump in the throat and cause difficulty swallowing, dizziness, especially when raising the head suddenly, ringing in the ears and decreased visual acuity, the appearance of a veil, “midges,” double vision eyes, fever or chills.
Diagnosis and treatment of cervical migraine.
The diagnosis is cervical migraine , based on complaints, the presence of injuries or cervical osteochondrosis. Tests are carried out by pressing the projection of additional vertebral arteries with worsening symptoms. In addition, the following are additionally prescribed:
- X-ray of the neck area, which helps to identify pathology of the cervical vertebrae, to clarify the cause of cervical migraine ;
- Ultrasound with Doppler to assess blood flow through the vertebral arteries;
- rheoencephalography;
- MRI and CT.
A laboratory blood test is ordered to check lipid and cholesterol levels.
Drug therapy for cervical migraine includes anti-inflammatory and painkillers, drugs that improve cerebral circulation, B vitamins (vitamin B6 is of particular importance), neuroprotective agents, antispasmodics, as well as drugs used in osteopathic practice. In particularly severe conditions in the presence of bone processes, stabilization of the cervical vertebrae is achieved using a surgical treatment method.
In the treatment of cervical migraine
, the main cause of which is cervical osteochondrosis, eliminating the development of the degenerative-dystrophic process in the intervertebral discs is of great importance.
Vitamin D, which has a high anti-inflammatory effect and takes part in mineral metabolism in the body, will help stop the inflammatory process, which allows you to eliminate deposits of calcium salts in soft tissues, blood vessels, joint and cartilage tissues, which helps to avoid the formation of osteophytes (bone growths), which contribute and significantly complicating the course of cervical migraine
. Vitamin D3 (one of the active forms of vitamin D) and vitamin B6, which is also involved in mineral metabolism and improves cerebral circulation, are part of the Osteo-Vit vitamins, acting together with difficult brood, which is a natural beekeeping product that provides the body with almost all useful substances , but also has an impact on hormonal levels, a significant change in which is often the cause of osteochondrosis and other diseases of the musculoskeletal system (osteomalacia, osteoporosis, arthritis, arthrosis, osteopenia). That is why taking the biologically active Osteo-Vit complex is of particular importance for women during menopause and postmenopause to strengthen bones and joint health, including in the complex treatment of autoimmune diseases, including rheumatoid arthritis. If there is a lack of calcium in the body, the biologically active complex Osteomed is indicated, which is used to eliminate calcium deficiency in the body, treat and prevent diseases of the joints and bone tissue.
Improve cerebral circulation, the disruption of which causes the symptoms of cervical migraine
It is recommended to take the Memo-Vit vitamin complex, which has a nootropic and hepatoprotective effect, helping to strengthen the walls of blood vessels in the brain.
In the treatment of cervical migraine caused by instability of the structures of the cervical spine or cervical osteochondrosis , it is important not only to restore cerebral circulation, but to improve the condition of the structures of the cervical spine, primarily to slow down and stop the degenerative-dystrophic process. For this purpose, it is important to take chondroprotectors, among which the leader among herbal products is the drug Dandelion P, produced on the basis of dandelion root using innovative cryogenic grinding technology, which has a significant advantage over herbal drugs made using traditional technology.
Herbal medicine for cervical migraine also includes taking valerian officinalis, on the basis of which the drug Valerian P is produced, which has the ability to relax spasmodic muscles, including the muscles of the neck, which allows, especially at the initial stage of cervical migraine
stop the development of a more severe irreversible process.
Timely treatment of cervical migraine has a favorable prognosis, allowing it to be stopped, significantly alleviate the condition and prevent the development of further organic changes.
We recommend reading:
How to stay healthy in old age? What is the danger of vitamin D deficiency in the body of older people?
Cervical spondylosis, symptoms, causes and treatment.
Vitamin D – its application in medicine is great and relevant!
Frequent back pain is the result of rapid aging of the spine. How to keep your spine healthy?
Neck pain is one of the symptoms of cervical spondyloarthrosis (cervicoarthrosis). Causes and treatment of cervical spondyloarthrosis.
Seasonal exacerbation of osteochondrosis. What to do during an exacerbation of osteochondrosis?
Dorsalgia is pain in the spine. Symptoms and treatment of dorsalgia.
Crunching in the neck when turning the head. Causes, symptoms and treatment
← What are the degrees of knee arthritis? Causes, symptoms and treatment methods for arthritis of the knee joint.
Symptoms of vitamin D overdose. How to choose vitamin D? →
Prevention methods
Symptoms and treatment of headaches with cervical osteochondrosis are associated with the mechanism of development of this disease. Injuries are one of its causes, but the pathological process can also manifest itself in a healthy person. Doctors recommend instilling the right habits from an early age that will help maintain the health of the cervical spine and prevent the development of dangerous diseases:
- correct posture both when walking and while working at the monitor is the main condition for an even load on the spine;
- moderate physical activity - even a healthy person can benefit from performing simple exercises daily to strengthen and increase the elasticity of the muscles and ligaments of the neck;
- a properly selected mattress and pillow will help avoid pinched nerves and ischemia of brain cells during sleep;
- avoiding heavy loads in everyday life - do not try to carry heavy loads in uncomfortable bags and packages;
- for those who do sedentary work - regular breaks for a short warm-up;
- in the cold season, wearing a scarf is mandatory.
Patients of the Clinical Institute of the Brain are often interested in whether a headache can occur from cervical osteochondrosis and how to prevent this unpleasant symptom. Pain in the head area, especially the occipital part, indeed often manifests itself even in the early stages. It is important not only to get rid of discomfort, but also to influence the pathological process and stop further tissue destruction.
Clinical Brain Institute Rating: 4/5 — 26 votes
Share article on social networks