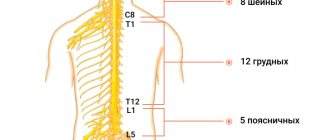
Chest pain can occur due to various diseases; it is sometimes difficult even for a doctor to understand it right away, so patients with such complaints usually undergo additional examination. Chest pain can manifest as diseases of the heart, respiratory system, gastrointestinal tract, spine, mediastinum, and central nervous system. All human internal organs are innervated by the autonomic nervous system, the trunks of which arise from the spinal cord. When approaching the chest, the nerve trunk gives off branches to individual organs. That is why sometimes pain in the stomach can be felt like pain in the heart - they are simply transmitted to the common trunk, and from it to another organ. Moreover, the spinal nerve roots contain sensory nerves that innervate the musculoskeletal system. The fibers of these nerves are intertwined with the fibers of the nerves of the autonomic nervous system, and therefore a completely healthy heart can respond with pain in various diseases of the spine.
Finally, chest pain may depend on the state of the central nervous system: with constant stress and high neuropsychic stress, a malfunction occurs in its functioning - neurosis, which can also manifest itself as pain in the chest.
Some chest pains are unpleasant, but not life-threatening, but there are chest pains that need to be relieved immediately - a person’s life depends on it. In order to figure out how dangerous chest pain is, you need to see a doctor. Perhaps this will save your life or calm you down if no serious problems with your health are found.
Causes of chest pain
- Heartburn. Acidic stomach acid that flows from the stomach into the esophagus (the tube that connects the mouth to the stomach) can cause heartburn, a painful burning sensation in the chest. It is often combined with a sour taste and belching. Heartburn chest pain is usually associated with food intake and can last for hours. This symptom most often occurs when bending or lying down. Taking antacids relieves heartburn.
- Panic attacks. If you experience attacks of unreasonable fear, combined with chest pain, rapid heartbeat, hyperventilation (rapid breathing) and profuse sweating, you may be suffering from “panic attacks” - a unique form of dysfunction of the autonomic nervous system.
- Pleurisy. Sharp, localized chest pain that gets worse when you inhale or cough may be a sign of pleurisy. The pain occurs due to inflammation of the membrane lining the inside of the chest cavity and covering the lungs. Pleurisy can occur with various diseases, but most often with pneumonia.
- Tietze syndrome. Under certain conditions, the cartilaginous parts of the ribs, especially the cartilage that attaches to the sternum, can become inflamed. Pain in this disease can occur suddenly and be quite intense, simulating an attack of angina. However, the location of pain may vary. With Tietze syndrome, pain may increase when pressure is placed on the sternum or ribs near the sternum. Pain during angina pectoris and myocardial infarction does not depend on this.
Osteochondrosis of the cervical and thoracic spine leads to so-called vertebrogenic cardialgia, which resembles angina pectoris. In this condition, there is intense and prolonged pain behind the sternum, in the left half of the chest. There may be irradiation into the arms and interscapular area. The pain increases or decreases with changes in body position, head turns, and arm movements. The diagnosis can be confirmed by performing an MRI of the spine. Magnetic resonance imaging of the spine will help determine the cause of pain in the chest if it is caused by pinched nerve roots or the presence of herniated intervertebral discs.
- Pulmonary embolism. This type of embolism occurs when a blood clot enters the pulmonary artery, blocking the flow of blood to the heart. Symptoms of this life-threatening condition may include sudden, sharp chest pain that occurs or gets worse with deep breathing or coughing. Other symptoms are shortness of breath, palpitations, anxiety, loss of consciousness.
- Other lung diseases. Pneumothorax (collapsed lung), high pressure in the blood vessels supplying the lungs (pulmonary hypertension), and severe asthma may also cause chest pain.
- Muscle diseases. Pain caused by muscle diseases usually begins to bother you when you turn your body or raise your arms. Chronic pain syndrome such as fibromyalgia. May cause persistent chest pain.
- Damage to ribs and pinched nerves. Bruises and fractures of the ribs, as well as pinched nerve roots, can cause pain, sometimes very severe. With intercostal neuralgia, pain is localized along the intercostal spaces and intensifies with palpation.
- Diseases of the esophagus. Some diseases of the esophagus can cause difficulty swallowing and therefore chest discomfort. Esophageal spasm can cause chest pain. In patients with this disease, the muscles that normally move food down the esophagus work uncoordinated. Since esophageal spasm can resolve after taking nitroglycerin - just like angina - diagnostic errors often occur. Another swallowing disorder known as achalasia can also cause chest pain. In this case, the valve in the lower third of the esophagus does not open as it should and does not allow food to pass into the stomach. It remains in the esophagus, causing discomfort, pain and heartburn.
- Shingles. This infection, caused by the herpes virus and affecting the nerve endings, can cause severe chest pain. The pain can be localized in the left half of the chest or be of a girdling nature. This disease can leave behind a complication - postherpetic neuralgia - the cause of prolonged pain and increased skin sensitivity.
- Diseases of the gallbladder and pancreas. Gallstones or inflammation of the gallbladder (cholecystitis) and pancreas (pancreatitis) can cause pain in the upper abdomen that radiates to the heart.
- Myocardial infarction - a blood clot that blocks the movement of blood in the arteries of the heart can cause pressing, squeezing chest pain that lasts more than a few minutes. The pain can radiate to the back, neck, lower jaw, shoulders and arms (especially the left). Other symptoms may include shortness of breath, cold sweats, and nausea.
- Angina pectoris. Over the years, fatty plaques can form in the arteries of your heart, limiting the flow of blood to the heart muscle, especially during exercise. It is the restriction of blood flow through the arteries of the heart that causes attacks of chest pain - angina. Angina is often described by people as a feeling of tightness or tightness in the chest. It usually occurs during physical activity or stress. The pain usually lasts about a minute and goes away with rest.
- Other causes of chest pain include inflammation of the lining of the heart (pericarditis), most often due to a viral infection. Pain with pericarditis is most often acute, stabbing in nature. Fever and malaise may also occur. Less commonly, the pain may be caused by a dissection of the aorta, the main artery in your body. The inner layer of this artery can separate under blood pressure and the result is sharp, sudden and severe pain in the chest. Aortic dissection can be the result of chest trauma or a complication of uncontrolled hypertension.
Because chest pain can have many different causes, do not self-diagnose, self-medicate, or ignore severe or prolonged pain. The cause of your pain may not be so serious - but in order to establish it, you need to contact a specialist.
Chest pain caused by changes in the central nervous system
Chest pain can also occur with other diseases. One of the most common diseases that causes frequent and prolonged pain in the chest is cardioneurosis, which develops against the background of a temporary functional disorder of the central nervous system. Neuroses are the body’s response to various mental shocks (intense, short-term or less intense, but long-lasting).
Pain due to cardioneurosis can have a different character, but most often it is constant, aching and is felt in the area of the apex of the heart (in the lower part of the left half of the chest). Sometimes pain due to cardioneurosis may resemble pain due to angina pectoris (short-term acute), but taking nitroglycerin does not relieve it. Often attacks of pain are accompanied by reactions from the autonomic nervous system in the form of facial flushing, moderate heartbeat, and a slight increase in blood pressure. With cardioneurosis, other signs of neuroses are almost always present - increased anxiety, irritable weakness, etc. Helps with cardioneurosis are the elimination of traumatic circumstances, the correct daily routine, sedatives, and for sleep disorders - sleeping pills.
Sometimes cardioneurosis is difficult to distinguish from coronary heart disease (CHD); the diagnosis is usually made based on careful observation of the patient, since there may be no changes on the ECG in either case.
A similar picture can be caused by changes in the heart during menopause. These disorders are caused by changes in hormonal levels, resulting in neurosis and metabolic disorders in the heart muscle (menopausal myocardiopathy). Pain in the heart is combined with the characteristic manifestations of menopause: flushing of the face, bouts of sweating, chills and various sensory disturbances in the form of “goosebumps”, insensitivity of certain areas of the skin, etc. Just as with cardioneurosis, heart pain is not relieved by nitroglycerin; sedatives and hormone replacement therapy help.
Diagnostics
A comprehensive examination begins with a general practitioner or family doctor. The specialist conducts a physical examination and identifies the leading pathological syndrome, and if necessary, sends the patient for consultation with specialized specialists (pulmonologist, cardiologist). To establish a diagnosis, the results of instrumental and laboratory tests are necessary, of which the following are most often prescribed:
- X-ray of the OGK.
Radiation diagnostics helps to differentiate cardiac and pulmonary pathology. Damage to the respiratory system is manifested by focal infiltrates, rounded shadows, and increased vascular pattern. Signs of cardiac problems are changes in the size and configuration of the heart shadow, congestion in the lungs. - Electrocardiography.
An ECG evaluates the electrical activity of the myocardium. The cardiogram reveals a decrease in the voltage of the waves or their inversion, deviation of the heart axis, and signs of disturbances in the myocardial conduction system. Daily ECG monitoring and bicycle ergometer test are of great diagnostic value. - Echocardiography.
Ultrasound diagnostics shows structural and functional abnormalities in the activity of the heart. The method is necessary for diagnosing pericarditis (effusion in the heart sac), cardiomyopathy (expansion of cavities or thickening of the walls of the organ). EchoCG allows you to measure the contractile function of the left ventricular myocardium. - Invasive methods.
In case of pathological processes in the pericardium, a diagnostic puncture is performed for bacteriological and cytological examination of the exudate. In case of coronary artery disease, coronary angiography is performed to assess the extent of vascular damage. The functional state of the myocardium is determined by perfusion scintigraphy. - Laboratory diagnostics.
Analyzes are of auxiliary value. In case of cardiac pathology, an extended biochemical study is indicated with determination of the lipid spectrum and acute phase parameters, measurement of myocardial markers. Diagnosis of pulmonary diseases requires microscopy and sputum culture.
Echocardiography
Chest pain due to diseases of the spine and ribs
Chest pain, very similar to heart pain, can occur with various diseases of the spine, for example, with osteochondrosis, herniated discs, ankylosing spondylitis, etc. Osteochondrosis is dystrophic (metabolic) changes in the spine. As a result of poor nutrition or high physical activity, bone and cartilage tissue, as well as special elastic pads between individual vertebrae (intervertebral discs), are gradually destroyed. Such changes cause compression of the spinal nerve roots, which causes pain. If changes occur in the thoracic spine, the pain may be similar to pain in the heart or pain in the gastrointestinal tract. The pain can be constant or in the form of attacks, but it always intensifies with sudden movements. Such pain cannot be relieved with nitroglycerin or antispasmodics; it can only be relieved by painkillers or heat. Pain in the chest area can occur when a rib is fractured. These pains are associated with injury and intensify with deep breathing and movement.
Chest pain due to lung diseases
The lungs occupy a significant part of the chest. Chest pain can occur against the background of inflammatory diseases of the lungs, pleura, bronchi and trachea, with various injuries to the lungs and pleura, tumors and other diseases.
Chest pain occurs especially often when there is a disease of the pleura (the serous sac that covers the lungs and consists of two layers, between which the pleural cavity is located). With inflammation of the pleura, pain is usually associated with coughing, deep breathing and accompanied by fever. Sometimes such pain can be confused with heart pain, for example, with pain due to pericarditis. Very severe chest pain occurs when lung cancer grows in the pleural area.
In some cases, air (pneumothorax) or fluid (hydrothorax) enters the pleural cavity. This can happen with a lung abscess, pulmonary tuberculosis, etc. With spontaneous (spontaneous) pneumothorax, sharp sudden pain appears, shortness of breath, cyanosis, and blood pressure decreases. The patient has difficulty breathing and moving. The air irritates the pleura, causing severe stabbing pain in the chest (in the side, on the affected side), radiating to the neck, upper limb, and sometimes to the upper abdomen. The patient's chest volume increases and the intercostal spaces widen. Help for such a patient can only be provided in a hospital.
Treatment
Help before diagnosis
Heaviness in the chest occurs when various organs and systems are affected, so self-medication at home is unacceptable and is fraught with the progression of the underlying disease and the development of complications. Patients experiencing chest discomfort are advised not to delay contacting a therapist. If squeezing pain is felt in the chest, the person experiences suffocation, febrile fever, and requires emergency medical attention.
Conservative therapy
Treatment measures are selected after identifying the causes of the condition. Heaviness in the chest does not require special symptomatic therapy and disappears after eliminating the underlying pathology. All patients are prescribed a gentle motor regimen, maximum limitation of stress and traumatic factors. Medicinal effects include drugs from the following pharmacological groups:
- Antianginal agents
. Used in combinations for long-term therapy of coronary heart disease. They are supplemented with antiplatelet agents to prevent myocardial infarction and thrombosis. Nitrates are recommended to relieve angina attacks. - Anti-inflammatory drugs
. Nonsteroidal anti-inflammatory drugs are indicated for myocarditis and pericarditis, acute respiratory diseases. They act pathogenetically and also relieve discomfort and pain. If nonsteroidal drugs are ineffective, corticosteroids are taken. - Antibiotics
. Antimicrobial drugs are prescribed for pneumonia, pleurisy, purulent bronchitis as etiotropic treatment. Penicillin antibiotics are effective for inflammatory lesions of the heart due to rheumatism. To treat tuberculosis, 3-4 specific drugs are combined. - Antiallergic drugs
. Leukotriene receptor antagonists and mast cell membrane stabilizers are used for basic therapy of bronchial asthma. Classic antihistamines are used as pathogenetic therapy for many inflammatory processes with an allergic component. - Metabolic drugs
. To improve the delivery and utilization of oxygen in the myocardium under conditions of ischemia, it is necessary to take cytoprotectors. Therapy is enhanced with ascorbic acid and B vitamins, which accelerate metabolic processes in the body.