In the modern era of high technology, with a predominantly sedentary lifestyle and work, a total lack of movement and an unfavorable ecological state of the external environment, spinal diseases are significantly common among almost all age groups of the population.
Unfortunately, not all spinal pathologies and their stages can be resolved with conservative treatment methods alone. In many cases, surgery remains the only chance to gain health, restore an active lifestyle, or get rid of pain. Despite the fact that spine surgery is considered one of the most complex and risky areas of orthopedics and traumatology, today innovative and microinvasive techniques of spinal surgery have brought it to a completely new level of development. Modern technologies and surgical techniques make it possible to solve the problem as safely as possible for the patient, significantly reducing intraoperative risks and shortening the postoperative recovery period.
Conditions for minimally invasive spinal surgery
- High resolution X-ray and imaging devices
- Cutting-edge software
- Endoscopic equipment
- Highly qualified specialists
- High-tech diagnostic tools (MRI)
- Neurosurgical diagnostic training
- Optimization of diagnostic and neurosurgical measures
- Combination of minimally invasive endoscopy and radiofrequency equipment (MDETT)
- Application of laser surgery
The benefits of minimally invasive surgery have been known for a long time. In many areas of medicine and partly orthopedics, minimally invasive procedures have proven themselves to be the best.
However, such operations did not immediately gain recognition in the medical world. The idea of minimally invasive spinal intervention seemed unattainable due to the lack of high-tech equipment needed in this field of medicine.
Currently, to perform an operation, a surgeon requires computers and special X-ray machines, which must have a high-resolution optical system. Such equipment can be quite expensive and requires a lot of training. This is why endoscopic spine surgery is offered by few clinics.
Laser vaporization
This surgical minimally invasive intervention is indicated for the early stages of protrusion and herniation of the intervertebral disc before the onset of sequestration. In this case, a conductor needle is inserted into the disk, through which a laser LED is supplied. Laser radiation is supplied through it, which coagulates the inner part of the disc. As a result, the pressure inside the disc decreases, its protrusion and compression of the spinal roots decreases.
The procedure has significant clinical advantages, such as less trauma, surgery lasting no more than an hour, low risk of complications and short recovery period.
Example of endoscopic spine surgery: Nucleoplasty of the intervertebral disc
The last and most important condition for successful minimally invasive spinal surgery is a team of highly qualified specialists who, together, can cope with the task.
In order to provide careful dorsal access to the spine, the most modern microendoscopic systems equipped with multifunctional surgical instruments are used. Better and clearer recognition of anatomical structures is made possible thanks to the latest generation of ultra-sensitive optics.
When performing endoscopic operations on the spine, access is made along existing main routes to avoid injury to bones and muscles. © Joimax
Why does your back hurt and why can’t you tolerate it?
Almost every person over 20 has experienced back pain at least once. What is the reason? The musculoskeletal system of Homo sapiens is well adapted for upright walking, and in some places even retains nostalgic memories of tree climbing (for example, the latissimus dorsi muscles, now needed only by climbers and bodybuilders).
Latissimus dorsi muscles. Any bodybuilder is far from a gorilla
Our main support - the spine - is made so as to spring and soften the “recoil” when walking, running and other fast, sudden movements. This occurs both due to its ventral (forward) and dorsal (backward) bends, and due to the elastic “gaskets” between the vertebrae - intervertebral discs.
The spinal column springs like a hybrid of a spring and shock absorber
But a comfortable civilized life arrived, by historical standards, literally yesterday, and life did not prepare us for this. Human biomechanics does not provide for the body to sit motionless in a car for 3 hours a day and at a computer for 8-10 hours. And if you deviate the spine from the vertical or change its natural deflection (for example, slouch), the pressure on the intervertebral discs increases significantly.
The pressure on the intervertebral discs in different conditions, the standing position is taken as 100% and is 5 bar (compared to: in a car tire - 2 bar)
Nature did not count on the fact that it would become fashionable to carry weights in the gym three times a week for the sake of beauty.
Load on the lumbar spine during exercises with weights - up to 730 kg
How many kilograms hang around your neck when you take out your smartphone?
The general conclusion is that the spine suffers for various reasons in almost all modern urban residents. You yourself or someone you know almost certainly has lower back or neck pain, discomfort and numbness in the limbs, severe headaches, tinnitus and spots in the eyes.
But people are so accustomed to these symptoms in everyday life that they simply adapt to them: they prop up pillows, roll over, or smear their backs with ointment from TV commercials.
Almost 90% of our patients, before coming to the clinic with complaints, self-medicated. Many have only made the problem worse. While a person lives with pain, changes occur in his bone, cartilage, and nervous tissue, often irreversible.
Pain is the first signal of such changes. Therefore, no one can tolerate it - it doesn’t matter that you are still young and accustomed to the fact that you usually have “nothing serious.”
Go to the doctor in time and get an MRI - this small effort can save you years of free movement and prevent really serious problems, even paralysis.
Open spine surgery - possible complications
- Damage to blood vessels
- Nerve damage
- Bone surgery
- Postoperative complications are more common
- Higher likelihood of infection due to long rehabilitation
- Removal of surgical sutures
- Prolonged wound healing
- Formation of chronically painful scar tissue that causes irritation
Surgery using tubular drainage avoids large incisions in the skin, muscles, nerves and bones. The surgeon performs this operation through an incision less than 1 cm in size. In both cases of protrusion and herniated intervertebral disc, this method is an excellent alternative to open spinal surgery.
Hernia, protrusion, stenosis and other troubles
The most common cause of acute back pain, impaired movement and function of the limbs in relatively young patients (under 50 years of age) is a herniated disc.
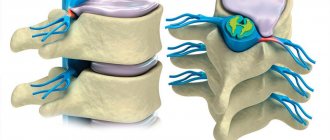
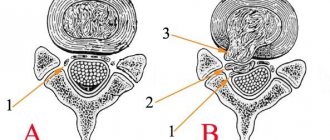
Here are healthy vertebrae and the disc between them.
The structure and position of a healthy intervertebral disc
The disc consists of a dense fibrous fibrous ring, inside of which there is a gel-like structure - the nucleus pulposus. The disc is covered with cartilage tissue above and below.
Intervertebral discs act as shock absorbers when we move, sit or stand for a long time. They prevent contact and abrasion of the vertebrae. If the intervertebral disc is subjected to strong pressure for too long and regularly, degenerative changes occur in it.
The fibrous ring gradually deforms and becomes uneven in thickness. And the nucleus pulposus is still subject to stress. Where the thickness of the “bruised” fibrous ring is minimal, the core pushes it outward, beyond the boundaries of the vertebral body. This protrusion with a violation of the homogeneity of the fibrous ring is called protrusion.
It may not cause serious problems. If you take precautions, you can live with protrusion for the rest of your life. But it is dangerous that problems already exist, and without symptoms a person does not know about them and does not consider it necessary to protect the spine.
Then, over time, the protrusion increases. And where the fibrous ring is thin, that’s where it breaks. The nucleus pulposus is squeezed out. This is how a hernia is formed.
If it extends towards the spinal canal, it compresses the spinal cord or nerve roots passing there, causing severe pain and disrupting nerve conduction.
Acute pain syndrome, immobilization (“jammed back”), dysfunction of the limbs, dizziness, sometimes even temporary paralysis and dysfunction of some organs appear.
Development of a degenerative process in the intervertebral disc
A hernia can occur at 20 or at 70 years old, but in old age (after 50 years) the cause of problems with the back and limbs is often not acute, as in the case of a hernia, but a gradual chronic process. Stenosis is a narrowing of the spinal canal.
The reasons are common: age-related changes in intervertebral discs, their “wear and tear”. Consequently, there is destabilization of the vertebrae, a decrease in the distance between them, and overstrain of the facet joints. Plus a decrease in bone density and weakening of muscles, which makes the vertebrae even less able to withstand the load.
The body tries to compensate for instability of the spinal column by building up rigid, dense structures in “weak spots.” Quite often, hypertrophy (enlargement) and ossification (ossification) of the ligamentum flavum, proliferation of facet joints, and formation of osteophytes (growths of bone tissue) develop. All these “additional reinforcements” take up space, narrowing the spinal canal.
The most likely causes of spinal canal stenosis
All this leads to pain syndromes, neurogenic lameness, etc.
Advantages of minimally invasive technique compared to open surgery
- Minimal incision: faster recovery process
- Reduced blood loss, rapid recovery
- Smaller incision: minimal pain after surgery
- Minimal soft tissue damage without scarring
- Small surgical wound: minimal risk of complications, faster return to professional activities.
- Local anesthesia: reducing surgical risk
- Local anesthesia and sedation
- Skin incision 5-6 mm.
- An endoscope (optical instrument) is passed through natural spaces in the vertebrae
- The endoscope is directed to the location of pain inside the spinal cord, under constant X-ray control
- Visualization of spinal cord nerve roots
- Herniated discs are removed using microscopic instruments
- Constant monitoring and documentation of the process
- The procedure lasts 30-45 minutes
- No stitches required
- Immediate mobilization of the patient on the day of surgery
- Physiotherapy begins after one day. Treatment must be continued on an outpatient basis.
Complications characteristic of open spine surgery occur after minimally invasive techniques in extremely rare cases.
What are the conditions of stay at the Gelenk Clinic?
Single ward at the Gelenk Clinic in Gundelfingen.
© joint-surgeon During your inpatient stay at the clinic, you are in a single room with a shower and toilet. Each room has towels, a bathrobe and slippers. Also, you will have a minibar, safe and TV. You must bring your own medications, comfortable clothes and nightwear. After surgery, the patient is cared for by experienced medical staff and professional physiotherapists 24 hours a day. As a rule, hospital stay does not exceed three days. Your relatives can stay at a hotel located a few steps from the clinic. We will gladly take care of your hotel room reservation and will be happy to organize your treatment in Germany.
When can your spine specialist suggest alternative treatments?
- Progressive spinal stenosis
- Scoliosis
- Herniated disc in the cervical spine
- Spondylolisthesis (slipping of a vertebra)
- Ankylosing spondylitis (Bechterew's disease)
- Spondylosis (hardening or fixation of the vertebrae as a result of pathological changes in the spine)
- Intervertebral disc herniation beyond the reach of the endoscope (transforaminal access)
For more detailed information, please contact our clinic specialists.
Minimally invasive spine surgery is a promising branch of medicine with clear advantages over other treatment methods. Due to their high qualifications, the experienced surgeons of our clinic can perform the most complex procedures on the spine and spinal cord with a minimal level of tissue trauma. The recovery period is short and the surgical risk is minimal. However, compared to other spinal surgery methods (eg open microsurgical discectomy using a surgical microscope), the minimally invasive technique is a fairly new procedure.
- Clinical research
on many techniques and indications in minimally invasive spine surgery remains limited. Short-term results are successful, but the method has its drawbacks - Disadvantages of established standards for MIS operations
Many decisions in minimally invasive spine surgery depend not on established standards, but on the individual experience of a highly qualified surgeon. - Limited field of view:
Reduces the ability to respond to complications that may arise during surgery. In some cases, if unexpected complications arise during endoscopic surgery, the surgeon may decide to perform open surgery. - The standard curriculum
of many educational institutions does not include training in the technique of performing MIS operations. Therefore, patients must ensure the qualifications and long-term experience of the surgeon.
medical request
Displacement of the cervical vertebrae: treatment
Displacement of the cervical vertebrae is a serious disease that can lead to irreversible destruction processes leading to disability. This is why you need to start treatment immediately.
The latter is prescribed by a doctor, who constantly monitors all manipulations during recovery. The main method of treatment is surgical. Stabilization of the cervical vertebrae will avoid serious consequences. The operation is performed under general anesthesia. Discharge after 10 days.