Each finger of the hand has the ability to move freely throughout the entire range of motion. The efficiency, smoothness and strength of such movements are made possible thanks to a unique system of blocks. This system consists of a number of retinacular (retaining) type structures that are either annular or cruciform in nature. There are five ring blocks (A1-A5) and three cross-shaped blocks (C1-C3).
Flexor apparatus of the hand
The condition trigger finger syndrome (FFS) is thought to be caused by inflammation and subsequent narrowing of the A1 block of the affected finger (usually the third or fourth). The A1 block is most often affected, but there is some evidence that the A2 and A3 blocks are affected. Additionally, this problem can occur in the thumb and the condition is then called snapping thumb syndrome.
A decrease in the size difference between the flexor tendon sheath and the flexor tendon itself can lead to increased friction between the two surfaces and therefore disruption of the gliding process, leading to progressive inflammation between the tendon and its sheath.
Friends, on July 17 in Moscow, as part of the #RehabTeam project, Anna Ovsyannikova’s seminar “Rehabilitation of the hand after a fracture of the distal radius (fracture of the “radius in a typical place”)” will take place.” Find out more... In addition, on July 18, she will conduct a seminar “Rehabilitation of the hand after fractures of the metacarpal bones (Boxer fracture).” Find out more...
SSP is called “stenosing tenosynovitis.” However, histological studies have shown that inflammation occurs more in the tendon sheath rather than in the tendon itself, making this name a misleading description of the actual pathophysiology of the disease.
Epidemiology/Etiology
According to statistics, this problem occurs in the fifth or sixth decade of life, and women suffer more often. The average age is 58 years. The chance of triggering finger is 2-3%, but in the diabetic population it increases to 10%. This is not due to the glycemic profile, but rather to the duration of the disease. SSP may occur in patients with
- carpal tunnel syndrome,
- de Quervain's disease,
- hypothyroidism,
- rheumatoid arthritis,
- renal failure,
- amyloidosis.
Many potential causes of SCP have been discussed in the literature. However, there is little clear evidence of the exact etiology of this disease.
- Occupational causes of SSP have been proposed, but the research on this is very inconsistent.
- The authors hypothesize that SCP may occur as a result of any activity that requires prolonged forceful flexion of the fingers (eg, carrying shopping bags or briefcases, prolonged writing, rock climbing, or strenuous grasping of small tools or objects with sharp edges).
- It is important to take into account that the cause of SSP is often multifactorial in nature.
- It is also known that this condition can develop idiopathically or secondary to other pathologies.
Clinical picture
Stuck finger (before and after treatment)
SSP has a number of clinical manifestations. Initially, patients may experience a painless clicking sound when moving the affected finger. This may progress to painful sticking and jerking of the finger, usually at the metacarpophalangeal and proximal interphalangeal joints.
Possible additional symptoms are:
- Stiffness and swelling (especially in the morning).
- Intermittent fixation of the finger during active flexion, requiring passive extension.
- The finger locks or snaps in a bent position and then suddenly straightens.
- Decreased flexion/extension amplitude.
- A palpable tender nodule proximal to A1 and/or the finger is fixed in a flexed position.
- A slight thickening at the base of the finger and pain that may radiate to the palm or the distal part of the finger.
What is trigger finger?
Trigger finger, or in other words stenosing ligamenitis, is a disease that blocks the finger. It will not be possible to align the blocked finger with the other hand and bring it to its normal position. When you try to straighten a bent finger, you may hear a clicking sound. Especially in the morning, after waking up, obvious swelling can be observed in painful and stiff fingers. Trigger finger disease can affect one or more fingers. This disease most often affects the little finger, ring finger and thumb, and mainly on the right hand.
Differential diagnosis
The main characteristic of this disease is stuckness and intermittent movements of the affected finger. However, this characteristic is not unique to the snapping finger. Other etiologies associated with finger sticking include:
- Dupuytren's contracture;
- focal dystonia;
- swelling of the flexor tendon or its sheath;
- sesamoid bone abnormalities;
- post-traumatic entrapment of the tendon in the area of the head of the metacarpal bone.
Rating scales
- Digital pain rating scale.
- Measuring hand grip strength (using a JAMAR dynamometer).
- DASH Questionnaire.
Stages of stenosing tenosynovitis
- 1 is normal.
- 2 - painful compaction.
- 3 - clicks.
- 4 - the proximal interphalangeal joint (PIP) gets stuck during flexion and unlocks during active extension.
- 5 - The PMS gets stuck during flexion and unlocks during passive extension.
- 6 - The PMS is fixed in a bent position.
Stage 5 or 6 according to the above classification
Survey
History taking
Ask the patient specific questions to better understand the nature of their symptoms, which will help you diagnose the condition. For example:
- Recent injury.
- Repetitive movements associated with work.
- Clicking or getting stuck in the affected finger when bending or straightening it.
- Referred pain in the palm or fingers.
Accompanying illnesses
- People with diabetes are 4 times more likely to suffer from this disease.
- Disorders that cause connective tissue changes, such as rheumatoid arthritis and gout, may also be associated with PTS.
Inspection
- Finger fixed in a flexed position.
- Bone proliferative changes in the adjacent PMS.
Palpation
- A painful nodule in the MCP joint is secondary to swelling of the tendon or tendon sheath.
Range of motion
- Decreased range of motion, mainly extension.
Manual testing
- Flexor digitorum profundus.
- Superficial flexor digitorum.
- Measuring hand grip strength.
Note: If your finger is blocked, testing may not be possible.
Additional joint movements
- Distal and proximal interphalangeal joints, metacarpophalangeal and carpometacarpal joints of all fingers.
- Surrounding soft tissue.
- Wrist joint.
Special tests
- Fist flexion test (10 times). The patient must actively clench his fingers into a fist 10 times. Accordingly, the number of clicks is assessed on a 10-point scale. If the patient's finger remains blocked at any point in time, the test ends with a score of 10/10.
Causes of Knott's disease
Often patients do not understand why their fingers click when unclenching their fist and mistake this for normal tissue behavior after tension. However, it is not. Prerequisites for the development of such a disease may be:
- genetic predisposition;
- severe physical stress on the hand, excessive finger tension;
- violation of metabolic processes;
- diseases of the joints and ligaments (arthritis, arthrosis);
- systemic connective tissue diseases;
- hand injuries;
- inflammatory processes.
Knott's disease sometimes occurs in children. In these cases, the causes may be heredity and diseases affecting the connective tissue.
Treatment
The chronic nature of symptoms associated with snapping finger makes conservative treatment difficult and often ineffective. However, conservative treatment is always recommended as a first step before surgery.
Non-operative treatment
Corticosteroid injections
The use of corticosteroids has been shown to be effective in reducing pain and the frequency of clicking. The drug is injected into the affected tendon and reduces inflammation and pressure on the tendon, which leads to improved gliding through the flexor pulleys. This option is an effective and safe alternative to surgery. Patient satisfaction, safety, and functional improvement are characteristics of steroid injections compared with surgical treatment. Surgery is associated with higher costs, longer absences from work, and the possibility of complications. Studies have also shown that combining corticosteroid injections with lidocaine is significantly more effective than lidocaine alone.
Possible side effects
- Inflammation at the injection site.
- Tendon damage.
- Allergic reactions.
- Atrophy of subcutaneous fat at the injection site.
Contraindications
- Age up to 18 years.
- Any previous treatment or surgery in this area within the last six months.
- Possible traumatic or tumor origin of symptoms.
Physical therapy
As with all diseases of the upper extremity, screening of the proximal segments is necessary. Additionally, because poor posture can contribute to distal problems, it should be corrected to ensure optimal patient outcomes.
Patient education
Since SCP is also considered an overuse injury, patient education is critical. This concerns
- recreation;
- physical activity modifications;
- postures;
- orthoses.
Orthotics
Orthotics for trigger finger syndrome
The first step in treatment is to stop the activities that make the condition worse. Orthotics/splinting is one of the best ways to limit movement. Most authors agree that the goal of orthosis is to alter the biomechanics of the flexor tendons to maximize differential tendon gliding. However, experts disagree on which joints should be splinted and how to properly position the joints. There are different ways to orthose a patient, but ultimately it will depend on what gives the patient the most relief. Orthoses are usually worn for 6-10 weeks. Some authors recommend positioning the MCP joint at 0 degrees, which allows full range of motion of the distal interphalangeal joint (DIP). It should be noted that splinting has lower success rates in patients with severe conditions or long-term symptoms.
There are two options for orthotics that have shown (according to recent studies) good results:
- Orthotics DMS. In 50% of cases this leads to a reduction in symptoms.
- MCP joint orthosis in a position of 15 degrees of flexion, which in 92.9% of cases leads to resolution of symptoms.
Exercises
There are three exercises that are recommended when treating patients with snapping finger (especially after surgical release):
- Fixation of the finger: the patient fixes the PFJ and flexes the finger in the MCP. This exercise can be performed with all fingers simultaneously or separately. The same can be done for VHI. The number of repetitions and sets are recommended depending on the level of pain and stiffness.
- Range of active movements: finger abduction and adduction are recommended to strengthen the palmar interosseous and lumbrical muscles.
- Tendon Sliding: Watch the video below.
Other events
Techniques such as heat/ice, ultrasound, electrical stimulation, massage, stretching, and joint mobilization (active and passive) may have some benefit for SCP. It is believed that heat may help by providing increased blood flow and stretchability of the tendon. Stretching after applying heat can provide greater extensibility. Movement and joint mobilization increase joint and soft tissue mobility (eg, slow passive traction and translational gliding).
Although there is no strong evidence, there are some documented cases and studies showing improvement in symptoms.
- 74 patients were treated with ten sessions of paraffin therapy, ultrasound, muscle stretching and massage. After 3 months, 68.8% of patients reported no pain or clicking. Of these 68.8% of patients, none had pain or clicking over the subsequent 6 months.
- 48 children were treated daily with passive exercises for the affected thumb. After 62 months, this resulted in improvement (80% of cases for stage 2 and 25% of cases for stage 3).
Extracorporeal shock wave therapy
Recently, extracorporeal shock wave therapy (ESWT) has been promoted as a possible alternative to surgical treatment of musculoskeletal disorders in patients refractory to traditional conservative treatment. Yildirim and colleagues conducted a prospective randomized controlled clinical trial to determine the effectiveness of ESWT in the treatment of PSP compared with corticosteroid injections. Patients were followed up for one, three and six months. The researchers found that three sessions of ESWT treatment could be as effective as a corticosteroid injection in reducing symptom severity and functional status in Quinnell grade 2 patients. Patients in the ESWT group received 1000 shocks at 15 Hz over three sessions. There was a week's break between sessions. They found that both the ESWT and corticosteroid groups showed statistically significant improvements in all outcomes after treatment.
ESWT is thought to induce repair of inflamed tissue by stimulating tissue regeneration and nitric oxide synthesis, which is thought to lead to suppression of inflammation. There is also weak evidence that one of these mechanisms may have a beneficial effect on the thickening of the flexor tendon and its sheath. This allows you to overcome the obstacle in the snapping finger. ESWT offers an alternative for people who refuse corticosteroid injections due to potential complications (fear) or who are allergic to local anesthetics.
Surgical treatment
Open surgery
If conservative treatment is ineffective, surgical intervention is indicated. Open surgery combined with effective rehabilitation can quickly and significantly improve hand function with a low risk of complications. This technique, considered the gold standard, is performed by making a longitudinal incision in the palmar crease over the MCP joint of the involved finger, followed by release of the flexor digitorum profundus and flexor digitorum longus tendons. This procedure lasts 2-7 minutes and has an average discomfort time of 45 days after surgery. The advantage of this method is that it allows visualization of the block and therefore has a lower risk of damage to nearby nerves compared to endoscopic methods.
Endoscopic technique
This technique is performed by making two incisions: one in the palmar crease above the MCP joint and the other in the finger. An endoscope is then inserted to cut the block, releasing the flexor tendons. This procedure lasts two to nine minutes and has a shorter average time of discomfort (23 days) after surgery. Other advantages are the absence of scars and associated problems, as well as shorter post-operative recovery.
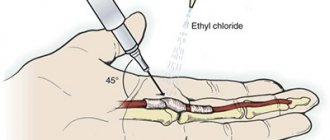
Transdermal release
This method can be performed with or without visualization. Percutaneous release without visualization (blind) is performed using anatomical landmarks to avoid damage to tendons and neurovascular structures. Recovery time is shorter than with open surgery, but there is a greater chance of nerve damage to the fingers, especially the 1st, 2nd, and 5th digits. The new ultrasound-guided technique helps clearly identify tendons and neurovascular bundles, preventing the potential complications that arise with percutaneous release without imaging, and also compares favorably with surgical techniques.
Non-Surgical Treatment for Snapping Finger
In one out of five cases, trigger finger disease tends to resolve on its own, without the need for surgery. In such cases, some anti-inflammatory drugs can be used as maintenance treatment. A splint or steroid therapy may be used. However, patients who came to our clinic with this problem say that despite using all these methods, they could not be cured. For Non-Surgical Treatment of Snapping Finger, we carry out a procedure that gives effective results and perform it under local anesthesia. The tendon sheath can be expanded with just a small incision and fine needles. That is, the clamped tunnel becomes freer. After the procedure, there is no need to wear a bandage on the arm for several weeks and lose its functionality, as happens during surgical operations; the bandage is applied only to the micro-access site and the patient can immediately return to their previous social life.