Today, spinal diseases affect more people of working age due to the specific nature of their work activities. The degree of activity during work can be at one of the extremes. This can be static sitting or standing work (for example, office workers, combine operators, workshop employees), or hard, exhausting work (loaders, construction workers). Few pay attention to the first occurrence of pain in the lower back, back or neck and go to the doctor with the problem; pain is a signal of the onset of degenerative changes in the joints, which is what subchondral sclerosis essentially is.
Features of the disease
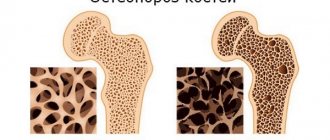
Few people know what spinal sclerosis is, although almost everyone has heard of this pathology. The disorder occurs due to the proliferation of bone structures and an increase in their density. This is not an independent disease, but rather a consequence of negative changes in the body. A characteristic change can develop in any area of the spine (cervical, thoracic, lumbar).
The pathology affects people of working age, mainly office workers, combine operators, workshop employees, and construction loaders. Anyone whose professional activity involves exhausting work and long periods of being in an uncomfortable position. The signal for the onset of characteristic changes is acute pain at the site.
There is no such pathology as subchondral sclerosis of the endplates of the vertebral bodies. The definition is used by doctors to indicate structural changes in joints on an x-ray. There are visible white spots on it, which indicates that these areas absorbed the most X-rays. It occurs as a result of damage to the intervertebral disc. Motor activity is significantly reduced and osteophytes develop.
Classification
Spinal endplate sclerosis can begin to develop anywhere in the skeleton. The greatest danger to a person is the pathology in the upper back, because even a slight mechanical impact can cause a compression fracture. The violation is classified as follows:
What are osteophytes on the spine
- Sclerosis of the cervical spine. Patients experience acute pain in the area of the cervical vertebrae. In addition, a number of neurological disorders may be present that occur due to damage to important vessels supplying the brain. Unpleasant symptoms also affect the upper limbs.
- Sclerosis of the spinal endplates.
- Sclerosis of the thoracic region. The development of such a pathological process often leads to a complete loss of motor function of the spine. There is an acute pain syndrome in the back, which patients often attribute to cardiac dysfunction due to its characteristic location.
- Sclerosis of the lumbar region. The lesion is widespread and extends to the entire lower back.
The affected area looks like compaction of bone tissue, as a result of which growths and osteophytes begin to appear. They, in turn, cause inflammation and cause pain. Regardless of the type of pathological process, every patient needs to receive medical care. Self-medication is excluded; consultation with an experienced specialist is required.
Only a doctor can make an accurate diagnosis based on the test results obtained.
Reasons for appearance
Sclerosis of the ridge develops against the background of an acute metabolic disorder in the body. The spinal tissue stops receiving useful substances, which leads to degenerative changes.
The main reasons for the changes are:
- Degenerative-dystrophic lesions (arthrosis, osteochondrosis).
- Joint injuries regardless of location.
- Presence of cracks in the vertebrae.
- A disease of an endocrine nature.
- Immune dysfunction, hormonal imbalances.
- Chronic inflammatory processes or infections.
- Autoimmune diseases.
- Obesity, excessive body weight.
- Poor nutrition, poor intake of vitamins and minerals.
- Sedentary work and sedentary lifestyle.
Provoking factors are also premature aging of fibers and inflammatory processes. Therefore, older people are at risk. Genetic predisposition and frequent stress should not be excluded from the list. The disease is concomitant and develops in the presence of other pathologies of the musculoskeletal system.
[node:field_similarlink]
Preventive measures
For prevention purposes, it is recommended:
- normalization of weight: excess body weight creates a constant high load on the joints of the limbs;
- rejection of bad habits;
- rational alternation of loads and rest without overwork;
- consult a doctor at the first signs of joint dysfunction;
- gymnastics, swimming.
Degenerative changes in joints are an integral part of the aging body. A balanced diet, moderate activity and timely treatment of inflammation will help maintain mobility longer.
Symptoms
Symptoms of the disease are easily confused with other pathological processes. They are directly related to acute disruption of the brain and pinching of nerve endings that enter the intervertebral space. Patients most often complain of the following conditions:
- Acute pain in the back, the exact localization depends on the location of the lesion.
- Problems with flexion and limited mobility of the neck.
- Difficulty carrying heavy bags.
- Poor coordination, unclear movements.
- Loss of sensation in the extremities (legs with lumbar sclerosis, arms with cervical or thoracic sclerosis).
- Deterioration of psychological state, appearance of depression.
- Memory problems, poor concentration.
- Impaired hearing or vision.
- Sudden weight loss not related to nutrition.
Symptoms of the disorder are not pronounced, and signs often appear in separate groups. In some patients, osteosclerosis is asymptomatic, which makes its timely detection in the early stages difficult.
X-ray is one of the effective ways to detect pathology
Osteosclerosis of the shoulder joint and head of the bone
Subchondral osteosclerosis of the shoulder joint can involve both the head of the bone and the glenoid cavity of the scapula. This disease can be caused by habitual dislocation of the shoulder, destruction of the articular labrum, cervical osteochondrosis, glenohumeral periarteritis and many other pathological processes.
Progressive osteosclerosis of the humeral head is manifested by the following clinical symptoms:
- nagging or aching constant pain in the shoulder area;
- inability to freely raise the arm in front of you and when abducted to the side;
- a decrease in muscle strength and, as a consequence, a decrease in the volume of the forearm due to degenerative processes;
- increased hand fatigue when performing work that is usual in volume and length;
- pain along the brachial and radial nerves;
- destruction of joint tissue and the appearance of crunching and clicking sounds typical for this process during rotational movements in the plane of the shoulder joint.
It is possible to treat osteosclerosis of the humerus without surgery only in the initial stages. Therefore, if you experience any pain in the shoulder area, we recommend that you immediately seek medical help.
Diagnostics
An orthopedic surgeon makes the diagnosis and treatment. You should contact him for advice when the first symptoms of the disease appear. To clarify the condition and exclude the presence of atherosclerosis or multiple sclerosis, the following types of instrumental studies are prescribed:
- X-ray. The easiest and fastest way to obtain complete information about the condition of the patient’s bone tissue. It is carried out in a clinic on the day of treatment.
- Ultrasonography. Prescribed for cervical localization, to clarify the condition of blood vessels or the functioning of internal organs.
- Magnetic resonance or computed tomography. Patients are referred only if there is a need to clarify certain information.
- Osteodensitometry. Using this examination technique, the size and condition of the formed bone compaction is determined.
Additionally, the patient will need to undergo urine and blood tests to identify the inflammatory process. Special tests help determine the genetic nature of the disease.
As a result of the data obtained, the degree of damage to the joint, features of changes in its structure, and the amount of growth of connective tissue are visualized. All this allows the doctor to determine the most correct tactics of control to return the patient to a normal quality of life.
No ads 1
Examinations that are carried out for the disease
The primary diagnosis of pathologies manifested by sclerosis is made on the basis of the clinical picture and anamnesis. To confirm it, a number of instrumental studies are carried out.
Here are the most informative:
- X-ray in 2 or 3 projections. Helps to detect the localization of altered tissues and determine the severity of the inflammatory or degenerative process.
- Magnetic resonance imaging. Used when radiographic examination is uninformative or when certain details are clarified.
- CT scan. It is carried out to assess the state of the circulatory network of the subchondral layer and determine the degree of innervation disorder.
Laboratory diagnostics are required only to determine the cause of the disease. Biological fluids (usually intra-articular exudate) are collected for microscopy and cytological examination. A general blood test is also indicated to assess general health.
Treatment of spinal sclerosis
There is simply no specific treatment for spinal sclerosis. Based on a thorough diagnosis, the specialist prescribes complex therapy, which is aimed at eliminating unpleasant symptoms, improving blood circulation in the damaged area and slowing down the progression of the pathology. It should be borne in mind that all degenerative changes in bone tissue are irreversible. Therefore, the sooner the patient consults a doctor, the higher the chances of maintaining health and normal physical activity.
Therapy involves taking painkillers, immunomodulators, and visiting a physiotherapist. Additionally, therapeutic exercises are prescribed and nutrition is adjusted. During the process of receiving treatment, the dynamics are monitored to exclude the rapid progression of the pathology. If a conservative approach does not give the expected result, the doctor prescribes surgery.
Drug therapy
Pharmacological products will help eliminate unpleasant symptoms and return the patient to the ability to move normally. A set of medications is selected individually, taking into account the patient’s age, health status, and the presence of chronic pathologies. It usually includes the following categories of medications:
- Non-steroidal anti-inflammatory drugs (Ketoprofen, Indomethacin, Ketorolac). With their help, the inflammatory process is eliminated, the condition is alleviated and back mobility is restored.
- Chondroprotectors (“Inoltra”, “Aflutop”, “Mukartrin”). The drugs are aimed at activating regeneration processes in the body to restore damaged cartilage tissue. The effect is cumulative, so the patient will need to take the medication chosen by the doctor for at least 3 months.
- Muscle relaxants (Tizanidine, Baclofen, Mydocalm). Medications are aimed at eliminating muscle spasms and improving general condition.
- B vitamins, calcium, phosphorus. Such components are important for ensuring tissue regeneration.
Drugs are prescribed in tablets, capsules or injections. In some cases, ointments are used to relieve pain, or special patches. Changing the medications chosen by the doctor or reducing the dosage is strictly prohibited. This will not allow you to get the expected result and will lead to rapid progression of the pathology.
No ads 2
Physiotherapy
Physiotherapeutic procedures have proven themselves in the treatment of spinal sclerosis. They can increase blood flow to the affected area, reduce inflammation and speed up tissue repair. All this slows down the progression of the pathology and improves the patient’s condition. The main methods prescribed by the doctor are:
- Electrophoresis. Allows you to increase blood circulation in the affected area. It is carried out using a drug. Due to microcurrents, they penetrate deep into the tissues and locally affect the problem.
- Ultrahigh frequency therapy. Prescribed to patients in the absence of contraindications. The procedure is carried out using special equipment that creates high-frequency electromagnetic fields that improve the condition of damaged tissues.
- Mud or hydrogen sulfide baths. They have a general healing effect on patients. They are carried out in special rooms, most often in sanatorium conditions. Courses of 10 sessions allow for a noticeable improvement in the patient’s condition.
- Massage. A visit to a specialist can increase the strength of muscle tissue, stabilize the spine, increase blood flow in the massaged area, and eliminate muscle spasms. The process uses various techniques, stroking, kneading, rubbing, to normalize physiological processes in the damaged area.
- Acupuncture. Impact on certain points in the body allows you to activate the regeneration process and improve the condition of the muscles. But the session must be carried out by a specialist with extensive experience and qualifications, otherwise unprofessional influence can provoke serious complications.
Physiotherapeutic procedures allow you to achieve lasting results and improve the patient’s well-being
During an exacerbation, visiting the physiotherapy room is strictly prohibited. Sessions are prescribed only during the period of elimination of acute pain syndrome and relief of the patient’s condition. The entire process of exposure is strictly controlled by a doctor.
Physiotherapy
It is almost impossible to achieve lasting results from complex treatment without a course of exercise therapy. The orthopedic doctor prescribes a set of physical exercises to the patient aimed at restoring spinal mobility, normalizing blood flow and eliminating muscle spasms. It is compiled individually, based on methods developed by specialists (Dikul, Bubnovsky, Shishonin).
Regular training allows you to minimize the likelihood of ossification of the ridge, will strengthen the body and muscles as a whole, and fix the vertebrae in the correct position. Loads should always be moderate, with a gradual increase in the number of movements as the condition improves. Otherwise, there is a high risk of injury.
No ads 3
Surgical intervention
When conservative treatment does not produce the expected results and the disease continues to progress, the doctor resorts to surgery. Predominantly arthroscopic techniques are used, one of which is endoprosthetics. It allows you to completely replace the articular platform or a separate part of it.
The main indication for prescribing such a radical treatment method is sclerosis of the joints and joints, when loss of motor function is at risk. After the intervention, patients require rehabilitation.
Spinal sclerosis is a serious pathological process that develops against the background of a chronic disease of the musculoskeletal system. The main cause of development is an acute circulatory disorder in the back, which often occurs due to injury, characteristics of professional activity or other negative effects on the body. To receive comprehensive treatment, you will need to undergo an examination.