The beauty of women has always been of great importance. Perhaps all modern men will agree with this, and what’s more, even the classics of Russian literature mentioned it. However, it happens that legs, or rather feet, lose their beauty due to a protruding “bone” at the base of the big toe. It is important to understand how to deal with the bunion so as not to torment yourself with pain all your life.
A sore “bunion” (as deformities on the big toes are often called) is perhaps the most popular orthopedic problem, and it is mainly women who suffer from it. Statistics say that men are four times less susceptible to it. The cause of pain in the bone lies in the failure of the ligamentous apparatus - a congenital problem transmitted mainly through the female line.
Peculiarities
When there is a painful bulge on the outside of the foot at the base of the little toe, podiatrists diagnose Taylor's deformity, or "tailor's disease." For the first time, a detailed description and diagnosis was carried out by the American specialist H. Davis in 1949, noting complete identity with the development of Hallux Valgus.
An inflamed area forms on the lateral surface of the head of the little finger bone, causing the finger to deviate inward. The pain can radiate to the lateral part of the foot and provoke inflammation of the ligaments, bone and cartilage tissue. Characteristics:
- the forefoot expands, the angle between the 4th and 5th toes increases;
- the little finger takes on the shape of an arc; with the varus subtype, it can overlap the ring finger in a cruciform manner;
- a “bone” is formed on the outside.
For a long time, the pathology develops asymptomatically. The foot gradually increases in volume due to a growth, an increase in the fourth intermetatarsal angle. Conservative treatment eliminates the disease only at the initial stage. In most cases, surgery is performed using different methods.
Causes
The disease is not common, but is not a rare pathology. In most cases, orthopedists associate the appearance of a painful growth with genetic predisposition and hereditary risk factors. In many patients, the formation is observed on both legs at the same time.
When diagnosing the causes of Taylor deformity, they are conventionally divided into several types:
- Post-traumatic. The growth forms after a fracture, improper fusion of bones, against the background of frequent subluxations and dislocations.
- Structural. The reasons are associated with an abnormal disorder during the intrauterine formation of the arch of the foot. Genetically weak ligaments do not hold the fingers in the correct position when walking or running. Pathological redistribution of the load provokes expansion of the anterior section and its deformation.
- Functional. Congenital or acquired gait features in which the main load is on the outer part. The problem is exacerbated by wearing tight or narrow shoes.
The fifth metatarsal bone is often deformed due to congenital clubfoot, a pathological absence of small bones in the little toe area. In response to increased load, the bone head grows and changes in the structure of cartilage tissue occur.
The main factors that increase the risk of developing the disease:
- osteoporosis;
- rickets;
- inflammatory diseases of the joints;
- excess weight;
- abnormal structure of the foot;
- lack of physical activity, sedentary lifestyle;
- systemic connective tissue diseases;
- disruption of collagen production in the body.
The formation of growths is caused by the abnormal structure of the little finger, including the hammer-shaped or dumbbell-shaped bones. At risk are people with a history of cerebral palsy, Lederhosen contracture and meningitis.
An external cause of deformation can be wearing tight shoes with narrow toes and high heels. Such shoes connect the toes, incorrectly redistribute the load on the foot, provoke a fanning of the metatarsal bones, and deform the head.
Arthrosis of the big toe - hallux-valgus, deformity of the big toe
Arthrosis of the big toe, colloquially called gout, actually has nothing in common with gout. Although true gout does often affect the big toe, it is much less common than arthrosis.
Moreover, while gout affects mostly men, arthrosis of the big toe develops most often in women. You can read more about classic gout here *
Many people mistakenly assume that arthrosis and deformity of the big toe occur due to poor nutrition or due to mythical salt deposits. But that's not true.
In fact, arthrosis of the thumb sometimes develops after a fracture, a severe bruise, or after a subluxation that occurs during an awkward movement of the foot (after a person stumbles or steps on, say, a stone).
But the most common cause of arthrosis and accompanying arthrosis deformation of the big toe is the special structure of the foot (“wide foot”), coupled with flat feet and prolonged wearing of fashionable shoes with a narrow toe or shoes that are too tight.
Women in our country often had to wear such shoes (partly because of fashion, partly due to lack of choice) in times of total shortage. Perhaps it is precisely this circumstance that has led to the widespread spread of thumb pathology among our middle-aged and elderly women.
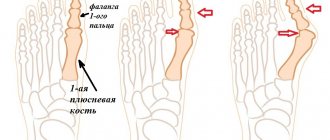
As a result of the pressure of tight shoes on the big toe, it eventually deviates strongly inward and is pressed against the second toe. The bone that protrudes due to deviation of the toe receives additional traumatization (rubbed by shoes) while walking and gradually becomes deformed.
Later, not only the protruding bone, but also the entire joint is deformed. It becomes much thicker than it was before. The joint is blocked, and movement in such a joint is severely limited.
With advanced arthrosis, the deformity usually fixes the finger in the wrong position so strongly that it is almost impossible to return it to its normal position. In addition to this, due to constant friction, inflammation of the periarticular bursa - bursitis - can occur. Then the joint swells, turns red and hurts when walking or the slightest touch.
On a note. Pain in arthrosis, even complicated by bursitis, with rare exceptions, occurs only when walking, from pressure on the big toe. In bed, they almost always go away within 1-2 hours - this is their difference from arthritic pain, which, as you remember, manifests itself more strongly at rest, at night, closer to dawn.
The situation with the deformation of the big toe is aggravated by the fact that it often “pushes out” the second and third toes with its pressure, which leads to a combined deformation of the entire foot, which is very difficult to treat with therapeutic methods.
Treatment of arthrosis of the thumb
To eliminate problems that have recently arisen, sometimes it is enough to choose the right shoes. For example, give up narrow-toed shoes and give preference to those with a wide toe, and use comfortable sports shoes more often.
You can use special spacers placed between the big and second toes to prevent the toes from closing. Such pads are now sold in many pharmacies.
Splints are not able to eliminate inflammation of the big toe bone, but they help straighten the sore toe and prevent it from deforming further.
Overlays for the metatarsal bone of the foot are available for night and day. They are made from different materials and have different prices. An orthopedist will help you choose an overlay (fixator).
In addition , if the joint of the big toe is not yet too severely deformed, you should try to restore it with the help of therapeutic exercises and with the help of therapeutic compresses.
Excellent therapeutic exercises for the big toe are given here: Exercises for bunion *
For compresses, dimexide , or bischofite , or medical bile are used . You need to buy these substances at the pharmacy.
I recommend starting with treatment with dimexide, and if it doesn’t help, move on to compresses with medical bile. Or with bischofite.
Socks with dimexide
Buy dimexide (liquid for compresses, in bottles). The drug can sometimes cause allergies, so before starting treatment it is necessary to test for sensitivity to it. To do this, apply dimexide with a cotton swab to the skin of the arm or shin and wait for about 1 hour.
If severe redness and itching appears, the medicine should not be used. If there is no reaction (a slight tingling feeling does not count), the drug can be used. If the test does not reveal the presence of an allergy to dimexide, we proceed to the procedure itself.
Voltaren - gel or diclofenac - gel into the inflamed bone of the big toe .
Then take a tablespoon of cold boiled water and a tablespoon of dimexide, and mix them in a cup.
After this you will need a sterile bandage. We moisten the bandage with the prepared solution, and wrap it around the foot (over the sore bone) 3-4 times, put on a transparent (but not colored!) plastic bag on top, and socks on top of it.
We wear this sock for 20 minutes the first time, and for subsequent days - up to one hour (no longer!). The procedure is done daily, but only once a day. The course of treatment is 20 days.
Attention! Under no circumstances should the compress be kept for longer than 1 hour!!! This may cause burns! Attention! Do not mix dimexide with water in advance, for example, the night before. The next day, the prepared solution no longer has any therapeutic activity! That is, you need to prepare a fresh solution every time.
Contraindications to Dimexide: - severe liver damage; severe kidney damage; angina pectoris or myocardial infarction; severe atherosclerosis; various types of stroke; glaucoma or cataracts; coma; - children under 12 years of age; pregnancy; lactation period; - hypersensitivity to dimethyl sulfoxide or other components of the drug.
Compresses with medical bile on the thumb bone
Compresses with medical bile are made as follows: 4–6 layers of gauze (gauze pad) need to be soaked in bile and applied to the sore joint.
Then we take a roll of cling film and bandage the gauze with bile with this film. And in addition, we wrap the entire foot so that the bile does not leak. Additionally, you can put a transparent plastic bag on your foot and cotton socks on top of it.
These “socks with bile” should be worn for 2 to 4 hours.
If you tolerate the procedure well and you are not allergic to bile, then after the first 3-4 procedures such “socks with bile” can even be left on overnight.
The procedures are carried out every other day, the course of treatment is 20 procedures.
Attention! Remember that bile is very soiled and can easily ruin clothes or bedding if it leaks from under your socks!
Contraindications: Hypersensitivity to the components of Medical Bile, violation of the integrity of the skin in the areas where the drug is intended to be applied, skin diseases (including inflammatory diseases of the skin and subcutaneous tissue, pustular diseases, erysipelas), acute diseases of the lymphatic system (lymphangitis and lymphadenitis).
With caution: Pregnancy, lactation, childhood.
Side effects: Possible irritation at the site of the compress, which goes away when the drug is discontinued. In this case, subsequent use of compresses is possible, but not earlier than after 15–40 days.
Important: medical bile should not be mixed with other medicinal substances.
Socks with bischofite
bischofite in liquid form. Most likely, bischofite will be sold under the label “bath liquid”, and it will be written that for baths it must be diluted with water. But you don’t need to dilute it for compresses!
At the same time, bischofite is often sold with herbal supplements - which one to buy does not matter. Buy any liquid bischofite.
We make a compress like this: soak a regular medical bandage generously in liquid bischofite and wrap the foot over the sore joint with this bandage. We put a transparent plastic bag on top of the foot, and woolen socks on top of the bag.
You need to take off this “sock” after 2–3 hours. But if you tolerate the procedure well, you can do it overnight. The course of treatment consists of 30 procedures performed daily.
Bishofite in gel form
Rub Bischofite gel into the joint and apply gauze (gauze pad) on top. Then we take a roll of cling film and bandage the gauze to the leg with this film. We put a transparent plastic bag on top of the foot, and woolen socks on top of the bag.
You need to take off this “sock” after 2–3 hours. But if you tolerate the procedure well, you can do it overnight. The course of treatment consists of 30 procedures performed daily.
***
If the deformity of the big toe has already gone too far, and neither compresses, nor fixatives, nor therapeutic exercises help you, then in this case, apparently, corrective surgery .
***
Article by Dr. Evdokimenko© for the book “Arthrosis”, published in 2003. Edited 2021. All rights reserved.
READ MORE:
- You can read the first chapters from the book “The Secret Formula of Health” here
- Chapters from other books by Dr. Evdokimenko
- Where to buy books by Dr. Evdokimenko
Symptoms and signs
At the initial stage, the formation at the fifth finger is almost invisible. As you grow, the following symptoms are observed:
- throbbing pain, burning and discomfort, which intensifies when walking or active movements;
- aching pain in a resting position;
- problems when choosing shoes due to widening of the foot;
- painful callus at the base of the little finger;
- swelling;
- skin redness;
- the appearance of corns.
Anatomical changes in the structure of the foot lead to severe pain, forcing a person to change his gait. Often the joint acquires a hammer-shaped shape, the little finger extends onto the fourth finger,
Indications for surgery
At the initial stage, conservative therapy helps to reduce the load on the affected joint and reduce pain. But you can completely get rid of the deformity only with the help of surgery. Among the main indications for resection:
- persistent calluses that develop into purulent wounds, ulcers that threaten sepsis, necrosis of the skin;
- loss of elasticity of the ligamentous apparatus, inability to bend or straighten the little finger;
- loss of support on the foot, which makes it difficult for a person to stand or walk;
- frequent relapses of purulent bursitis;
- loss of sensitivity due to damage to nerve endings.
Taylor's deformity leads to decreased quality of life. Pain limits mobility and leads to disability at a young age. A persistent inflammatory process provokes the destruction of cartilage plates and accelerates the development of osteoarthritis.
The main indication for surgical removal of a bone growth is the results of radiography. When receiving the image, the orthopedist measures the angle between the 4th and 5th fingers and the size of the head of the joint. The choice of tactics may be influenced by the severity of the deformity, the presence of flat feet or club feet in the patient, the development of bursitis and other inflammatory processes.
Conservative approaches for treating “bumps”
- Laying various fabrics (for example, felt) to reduce pressure on the bunion area.
- Physiotherapy treatment: laser, ultrasound are carried out to relieve the inflammatory and degenerative manifestations of the disease.
- Any calluses or abrasions on the skin that are also a source of pain should be treated.
- In order to prevent deviation of the first toe, it is recommended to wear physiological, properly selected shoes.
- If the deformity of the toe is severe, it is necessary that the shoes stretch well, especially the toe - this will relieve pressure on the bone.
- It is recommended to wear individual orthopedic insoles, which help to correctly distribute the loads on the foot when walking and running.
- Range of motion should be improved through exercise therapy and foot massage.
Features during operations
The mechanism of development of Taylor's pathology or tailor's disease largely mirrors the pathogenesis of hallux valgus in Hallux Valgus. this allows surgeons to use identical treatment and surgical techniques.
The purpose of surgical intervention is to restore the biomechanical connections in the forefoot, improve the condition of the ligamentous apparatus, and eliminate the aesthetic defect. It is necessary to remove the valgus deformity of the fifth metatarsal bone and return the parabola of the little finger to its natural position.
What is bunion surgery?
It’s still not entirely clear what to do if the bones on your feet near your big toe hurt? Let's take a closer look at the operation to remove the diseased bone. Surgical intervention on the bone of the big toe is expressed in the correction of the angle between the metatarsal bones and the phalanges of the fingers. This allows you to return the big toe to its normal position, correct transverse flat feet, and ultimately relieve pain and return the foot to its full function.
In each specific case, the surgical plan may vary depending on the degree of deformity of the foot and accompanying changes in the other toes.
Advantages of minimally invasive techniques
With early treatment, in 80% of cases, surgeons prescribe low-traumatic foot surgeries. The work is carried out through small incisions or pinhole punctures. Advantages of the methods:
- allow you to correct complex deformities in one procedure;
- give predictable results;
- You can operate on two feet at the same time;
- with the percutaneous technique, the patient can stand on his feet and move freely from the first day;
- no plaster cast or crutches are required.
Minimally invasive operations are highly specialized and are performed by highly qualified orthopedic surgeons using a special technical base.
Surgeries for Taylor deformity take from 25 minutes to an hour and can be performed on both legs simultaneously. In most cases, there is no significant blood loss, which shortens the rehabilitation period.
What is the treatment for a bunion? What to do if the bones on your toes hurt?
Many people have asked this question. Let's deal with him.
There are many methods to combat thumb deformation, including traditional ones:
- compresses,
- iodine nets,
- foot massage
- warm foot baths with herbal infusions and sea salt.
and others.
These remedies can help relieve pain and reduce inflammation, but they cannot cure the disease itself. The joint remains deformed, and the pain in the foot eventually returns. Only qualified orthopedic surgeons can truly cure this disease, and the radical treatment is surgery on the bone.
Main types of operations
If Taylor's pathology is diagnosed, doctors offer the following options for surgical removal of the painful defect:
- distal osteotomies (for types 1 and 2 of the disease);
- osteotomies at the level of the bone diaphysis (with type 2 or 3);
- operations in the proximal part for severe deformities of the 4th and 5th types.
In the latter case, the most popular and effective are: distal transverse osteotomy of the fifth metatarsal according to the method of Hohmann, Wilson, Mitchel, Helal and distal chevron osteotomy.
Some specialists prefer percutaneous distal osteotomy (Austin operation or CHEVRON), which aligns the axis of the foot. The technique is indicated for the formation of hammertoes and does not require intervention on the ligamentous apparatus.
In most cases, soft tissue surgery is additionally performed. Special plastic surgery involves excision of part of the damaged capsule, which remains in a stretched position after removal of the bone exostosis. The surgeon transposes the tendon from the main phalanx of the toe to the metatarsal head to hold it in the correct position.
Classic exostosis removal
At the initial stage, a minimally invasive technique is recommended, in which the surgeon makes punctures at the base of the finger. Using a special thin drill, it grinds down and removes bone growth and corrects the shape of the head, making it more natural.
On the inside of the foot, a thin triangular cut is made through a second puncture in the body of the metatarsal bone. The head is lowered into the formed recess, the finger takes the correct position relative to the longitudinal axis. The punctures are closed with intradermal sutures, a corrective bandage is applied to the foot and tightly fixed during dressing.
Operation by SERI
A minimally invasive method is recommended for stages 1 and 2 of Taylor's disease. During the procedure, a small incision is made on the outside of the foot, through which the surgeon removes up to a third of the head of the bone. After reducing the deformed area, the finger is fixed in its natural position using short-length metal knitting needles. In this case, the specialist does not touch the tendons, which reduces the recovery and healing time of the wound.
A characteristic feature of the operation using the SERI method is that the work is performed through an incision no more than 2-4 cm long. The wires hold the head of the bone in the correct position. The muscle frame is gradually formed. After complete healing and rehabilitation, the metal rods can be removed.
CHEVRON
Chevron osteotomy has been used to correct deformities since 1962. The operation allows you to reduce the angular dimensions and bring the 4th and 5th metatarsal bones closer together, reconstructing their anatomical position. An incision of no more than 3-4 cm is required.
Main stages:
- the surgeon cuts the skin on the foot under the damaged metatarsophalangeal joint;
- expands the joint capsule and injured ligaments, excises fibers that have shrunk due to deformation;
- after compression of the operated ligaments, the angle between the 4th and 5th bones decreases, the cause of the pathology is eliminated;
- the doctor makes an additional incision on the side of the foot and removes the bone tumor;
- moves the head of the bone, fixes the little finger with a titanium bolt or staples.
At the last stage of the operation, fluoroscopy of the foot is performed: the surgeon needs to make sure that the metatarsal bones are correctly positioned. The bolts must remain in the leg for at least 3 months.
Scarf osteotomy
For moderate and severe forms of deformity with an angle of up to 40°, scarf osteotomy is used. It allows you to eliminate the strong rotation of the little toe relative to the foot and the longitudinal axis. Advantages of the technique:
- allows the doctor to shift and rotate bone fragments to achieve optimal connection and correct position;
- if necessary, it is easy to shorten the metatarsal bone or lengthen it in case of a congenital anomaly or lack of longitudinal size;
- you can move the fragment up or down to correct the load when walking and reduce the risk of relapse;
- the surgeon can simultaneously correct the valgus deformity at the base of the big toe, which often complicates the course of Taylor syndrome.
During a Scarf osteotomy, the surgeon makes a thin incision on the side of the foot and divides the metatarsal bone in a zigzag (Z-shape) pattern, completely separating the head. Using a titanium bolt, it strengthens it in the anatomically correct position, while simultaneously adjusting the length and angle between the fingers.
During the operation, the tendons are additionally strengthened and, if necessary, cut and shortened. This increases the flexibility of the fibers and helps keep the bone in the anatomically correct position. All manipulations are performed under general anesthesia.
Weil's operation
With severe flat feet, patients often develop hammertoe and claw-like curvature of the 4th toe. The combination with curvature and cruciform overlap of the little finger leads to partial loss of support and gait disturbance.
Bayle's operation is performed under conduction or spinal anesthesia. For additional correction of hallux valgus, general anesthesia is recommended. During manipulations, the surgeon shortens the metatarsal bones of the deformed fingers, restoring their correct direction relative to the longitudinal axis. This allows you to change the load when walking and eliminate hypertonicity of the extensor apparatus.
Open angle osteotomy
It is performed from the inside, preserving bone tissue. During manipulation, part of the metatarsal bone is not shortened, but lengthened. Recommended for congenital pathologies and deformities associated with arthrosis. For plastic surgery, a fragment of pseudoexostosis is used, which is secured with titanium knitting needles and bolts. The technique is used to a limited extent and is often combined with other methods of treating Taylor syndrome.
Oblique diaphyseal rotational osteotomy
Indicated at an intermetatarsal angle of 12°. The surgeon removes the plantar surface of the head of the little finger bone at the bottom. The technique is used as a last resort in the absence of effectiveness from other methods of treating tailor's foot. Contraindicated in case of poor blood supply to the lower extremity, does not exclude repeated deformation.
Why does the bone in my foot hurt?
We need to figure out what is the root cause of the diseased “bone.” This, not surprisingly, is flat feet. A healthy person has a concave foot. There are two concavities in total: the longitudinal concavity is located inside the sole, the transverse one is located near the base of the toes. When the ligaments and tendons cannot withstand the load, the foot becomes flat.
In the case of transverse flatfoot, the metatarsal bones, instead of running parallel to each other, begin to fan out, and the toes follow them. What's wrong with this, you ask? This causes the appearance of a protruding bone: the big toe does not move outward, but, unlike its metatarsal bone, turns inward. As a result, the head of the metatarsal bone of the big toe begins to move out of the joint, and we see a “bump” at the very base of the big toe - this is a visual manifestation of the “bunion”.
Further, the deformation of the bone progresses. Why does the bone in my foot start to hurt? Contact of the protruding knuckle with shoes provokes chafing, which eventually becomes inflamed, and the person feels pain in that same bone on the toe. Next, osteochondral overgrowth appears, and the bone protrudes even more. After some time, its neighbors begin to suffer from the pressure of the deformed thumb. They bend in the wrong position, are fixed in it, eventually acquiring an unnatural curved shape, and pain appears in them too.
This leg disease is a serious problem, especially for women. There is a constant feeling of heaviness and pain in the feet, and the ability to wear shoes and other elegant footwear is lost.
Preparing for surgery
In most cases, manipulations are performed under spinal anesthesia. To exclude complications and develop a surgical plan, the patient is prescribed the following preparatory procedures:
- radiography of the foot in two projections;
- blood chemistry;
- coagulogram;
- tests for sexually transmitted diseases, HIV, hepatitis C;
- Ultrasound of the lower extremities;
- X-ray of the chest and respiratory organs.
For chronic diseases of the cardiovascular and endocrine systems, additional consultation and examination by specialized doctors is required.
Why is modern equipment important?
If you tried to find information about shock wave therapy on the Internet, you probably noticed that reviews about it are not only positive - sometimes the patient complains of discomfort, and sometimes that the operation was ineffective. The fact is that some clinics are trying to save money on patients and conduct therapy using outdated equipment, and this not only spoils the reputation of the method, but also poses a specific threat to your health.
Treatment of a bump on the leg at the clinic of the GENESIS Medical Academy is carried out using the most modern device “Dermablate Effect” from the German company, with which our clinic cooperates directly. A modern device can provide the following treatment benefits:
- Shock wave therapy is absolutely painless. The wave passes through soft tissues without causing you any discomfort;
- this technique is safe. The main danger of classical surgery is the risk of infection. In this case, this risk is absent, since the integrity of the skin is not compromised;
- The shock wave method is non-traumatic, especially when compared with surgery. This allows you to minimize the rehabilitation period;
- Treatment of hallux valgus with acoustic waves is fast. One session lasts about half an hour;
- during the treatment process there is no need to apply anesthetic ointments to the body or wear any special clothing;
- our device has a memory of settings, so it will be able to “remember” you during the first session, and during subsequent visits it will simply recreate the necessary settings and thereby save your time;
- the procedure carried out on our device is absolutely safe, since it is equipped with a special control system that is able to monitor the operation of all other systems and prevent any unforeseen failures;
- You will notice the first results of shock wave therapy after the first couple of sessions.
Rehabilitation period after surgery
On the first day, the patient is recommended to remain in the clinic under the supervision of a surgeon. The patient is fitted with special orthoses - Baruk boots, which, when walking, relieve the load from the forefoot and toes on the heel. These shoes must be worn for at least 6 weeks. In a difficult situation, you can additionally rely on crutches and limit physical activity.
After surgery, for 2 weeks it is recommended:
- bed rest;
- place a pillow or cushion under your feet to stimulate the outflow of excess fluid;
- for severe pain, apply cold compresses for 30 minutes up to 4 times a day.
To reduce pain, the doctor selects medications individually and calculates the dosage for home use. Swelling begins to decrease on the 3rd–5th day after surgery. After 14 days, it is recommended to visit the surgeon again to remove the skin sutures.
After 6 weeks, the patient is sent for a repeat x-ray. With pronounced positive dynamics and the absence of contraindications, walking without corrective orthoses with a load on the toes is allowed.
In some older patients, swelling may persist for a long time, which is associated with decreased tone of the veins of the extremities. In such a situation, lymphotropic therapy and contrast foot baths are prescribed.
Stages of development of hallux valgus
| Stage | Symptoms |
| 1 | At this stage of the disease, there are practically no complaints of pain. However, the thumb moves approximately 20 degrees from its normal position |
| 2 | This stage is characterized by more noticeable displacement and the appearance of primary, quickly passing pain, which is usually not noticed. Most often, painful sensations appear after a person has covered a long distance on foot. |
| 3 | At this stage, the finger has already shifted 30–50 degrees from its normal position. The pain becomes severe and increases when putting on shoes. Immobilization of the joint occurs. The pain is very disturbing when walking for a long time |
| 4 | The thumb angle is more than 50 degrees. The person feels severe pain all the time. Calluses, corns, and inflammations become its integral companions. |
It is necessary to visit a doctor already at the first stage, since in this case the treatment of the bunion on the big toe will be much more effective and painless. At the very beginning of the disease, it is possible to eliminate the problem yourself, using folk recipes or special medications. At the last stage, mandatory medical intervention is required, and in some cases only surgery helps.
Recommended articles on the topic:
- How to massage the abdomen for weight loss: different techniques for health and beauty
- Stone massage: description, benefits, methods
- MRI of three parts of the spine: when is it necessary and what are the features of the procedure
Contraindications for surgery
Absolute or temporary restrictions for performing an osteotomy on the foot are:
- osteoporosis and reduced bone tissue regeneration;
- exacerbation of rheumatoid arthritis;
- obesity 3-4 degrees;
- acute stage of infectious diseases.
Minimally invasive surgeries are allowed for varicose veins and joint bursitis.
Taylor syndrome leads to the formation of a painful growth at the base of the little finger, swelling, and calluses. New methods of surgical treatment can relieve the patient of complications and restore lightness to his gait.
Surgery
If all conservative measures are not effective, then a decision is made on surgical treatment. Currently, there are more than 100 surgical techniques for the treatment of Hallus valgus. The main tasks in surgical treatment are as follows:
- remove bunion
- reconstruct the bones that make up the big toe
- balance the muscles around the joint so that there is no recurrence of the deformity
Removing the “growth”
In some mild cases of bunion formation, only the growth on the joint capsule may be removed during surgery. This operation is performed through a small incision on the side of the foot in the area of the bunion. Once the skin is cut, the growth is removed using a special surgical chisel. The bone is aligned and the skin incision is closed with small sutures.
It is more likely that reconstruction of the big toe will also be necessary. The main decision that must be made is whether the metatarsal bone needs to be cut and also reconstructed. To resolve this issue, the angle between the first metatarsal and the second bone is important. The normal angle is approximately nine or ten degrees. If the angle is 13 degrees or greater, the metatarsal bone will most likely need to be cut and reconstructed. When the surgeon cuts and repositions the bone, it is called an osteotomy. There are two main techniques used to perform osteotomy and reconstruction of the first metatarsal bone.
Distal Osteotomy
In some cases, the distal end of the bone is cut and moved laterally (this is called a distal osteotomy). This effectively reduces the angle between the first and second metatarsals. This type of surgery usually requires one or two small incisions in the leg. Once the surgeon has achieved satisfactory bone alignment, the osteotomy is followed by fixation of the bones using metal pins. After surgery and healing, the pins are removed (usually they are removed 3-6 weeks after surgery).
Procymal osteotomy
In other situations, the first metatarsal bone is cut at the proximal end of the bone. This type of surgery usually requires two or three small incisions in the leg. Once the skin is cut, the surgeon performs an osteotomy. The bone undergoes reconstruction and is temporarily fixed with metal pins. This operation also reduces the angle between the metatarsal bones. In addition, the tendon of the adductor big toe muscle is released. Therefore, after the operation, a special bandage is put on.
Rehabilitation after surgery
It takes an average of 8 weeks for the soft tissue and bones to heal. During this period, it is better to place the foot in shoes with a wooden sole or a special bandage in order to prevent trauma to the operated tissues and allow normal regeneration. Immediately after surgery you may need crutches.
In patients with severe bursitis, physiotherapy (up to 6-7 procedures) may be prescribed a certain time after surgery. In addition, you must wear shoes with wide fronts. It is also possible to use correctors. All this can allow you to quickly return to normal walking.