© cunaplus — stock.adobe.com
Share:
The concept of a hand joint includes the wrist, midcarpal, intercarpal and carpometacarpal joints. Dislocation of the hand (according to ICD-10 code – S63) implies dislocation of the wrist joint, which is damaged more often than others and is dangerous due to damage to the median nerve and tendon jumper. This is a complex joint formed by the articular surfaces of the bones of the forearm and hand.
The proximal part is represented by the articular surfaces of the radius and ulna. The distal part is formed by the surfaces of the carpal bones of the first row: scaphoid, lunate, triquetrum and pisiform. Its most common injury is dislocation, in which there is a displacement of the articular surfaces relative to each other. A predisposing factor for injury is high mobility of the hand, which makes it unstable and highly susceptible to injury.
Causes
In the etiology of dislocation, the leading role belongs to falls and blows:
- Fall: on outstretched arms;
- while playing volleyball, football and basketball;
- while skating (skating, skiing).
- contact sports (sambo, aikido, boxing);
© Africa Studio - stock.adobe.com
Cause of radial head subluxation in children
The reason that causes subluxation of the head of the radial bone is usually a movement in which the child’s arm, which is in an extended position, is subjected to a sharp stretch by the hand or the lower end of the forearm along the longitudinal axis of the limb, often upward, sometimes forward. From the anamnesis it is possible to establish that the child stumbled or slipped, and the adult who was leading him, most often holding his left hand, pulled it to keep the child from falling. Sometimes in a small child this stretching of the arm occurs during play, when he is taken by both hands and rotated around himself, or when putting on and taking off a narrow sleeve. In some cases, adults indicate that the hand crunched.
How to distinguish a dislocation from a bruise and a fracture
| Type of hand injury | Features |
| Dislocation | Partial or complete limitation of mobility. It's hard to bend your fingers. The pain syndrome is pronounced. There are no signs of fracture on the radiograph. |
| Injury | Characterized by swelling and hyperemia (redness) of the skin. There is no impairment of mobility. The pain is less severe than with a dislocation or fracture. |
| Fracture | Swelling and pain are pronounced against the background of almost complete limitation of mobility. Sometimes there may be a crunching sensation (crepitus) when moving. Characteristic changes on the radiograph. |
Rehabilitation after dislocations
Immediately after the reduction of any dislocation in the wrist joint, it is necessary to develop the fingers of the hand, and after removing the plaster cast, the entire hand;
Restoring the functionality of the hands includes:
- Physiotherapy (magnetic therapy, ultrasound treatment, inductotherapy, mud therapy, UHF)
- Therapeutic gymnastics (with a recommended set of exercises to develop an injured joint)
- Massage of the fingers; after removing the cast, lymphatic drainage massage is prescribed
- Hydrotherapy
- Vitamin therapy
- The use of wound healing and restorative ointments
First aid
If a dislocation is suspected, it is necessary to immobilize the injured hand by placing it in an elevated position (it is recommended to provide support using an improvised splint, the role of which can be played by an ordinary pillow) and using a local bag of ice (ice must be used within the first 24 hours after the injury, applied for 15 -20 minutes to the affected area).
When applying a homemade splint, its leading edge should extend behind the elbow and in front of the fingers. It is advisable to place a bulky soft object (a lump of fabric, cotton wool or bandage) into the brush. Ideally, the injured arm should be above the level of the heart. If necessary, taking NSAIDs (Paracetamol, Diclofenac, Ibuprofen, Naproxen) is indicated.
In the future, the victim should be taken to the hospital for consultation with a traumatologist. If more than 5 days have passed since the injury, the dislocation is called old.
Treatment for subluxation of the radial head
Reduction of subluxation of the radial head on the 1st day is usually easy (without prior anesthesia).
Reduction technique. subluxation of the head of the radial bone in children: The shoulder is fixed in the area of the elbow joint with one hand, the first finger is placed in the projection of the head of the radial bone. With the other hand, carefully bend the forearm at the elbow joint at a right angle while simultaneously supinating and pressing the surgeon’s finger on the head. All movements are performed smoothly, but without interruption and with some force. At the moment of reduction during the transition to supination, a click is felt. The child screams, then quickly calms down, and after a few minutes free active movements are restored. In some cases, reduction is not immediately successful, and this technique must be repeated several times. Failure usually occurs from improper fixation and insufficient flexion of the arm or from incomplete supination. After reduction, immobilization is not necessary. You just need to explain to parents the mechanism of damage in order to avoid frequent relapses. It is advisable to recommend the use of “reins” when walking with toddlers. After the manipulation, the arm is suspended on a scarf for 3-5 days.
Kinds
Depending on the location of the damage, dislocation is distinguished:
- scaphoid bone (rarely diagnosed);
- lunate bone (common);
- metacarpal bones (mainly the thumb; rare);
- hands with a displacement of all carpal bones located below the lunate to the back, with the exception of the last. This type of dislocation is called perilunar. Occurs relatively often.
Lunar and perilunar dislocations occur in 90% of diagnosed hand dislocations.
Transscaphoid, as well as true dislocations - dorsal and palmar, caused by displacement of the upper row of carpal bones relative to the articular surface of the radius - are extremely rare.
Based on the degree of displacement, dislocations are verified by:
- complete with complete divergence of the bones of the joint;
- incomplete or subluxations - if the articular surfaces continue to touch.
Depending on the presence of concomitant pathologies, the dislocation can be ordinary or combined, with intact/damaged skin - closed/open.
If dislocations tend to recur more than 2 times a year, they are called habitual. Their danger lies in the gradual sclerosis of cartilage tissue with the development of arthrosis.
Fractures of the bones of the hand
Fractures of the hand bones account for up to 30% of all injuries to the skeletal system. As a rule, the injury occurs in everyday life, when falling with emphasis on the hand. A fracture of the wrist, phalanges of the fingers or metacarpal bones may occur. An accurate diagnosis can be established based on the results of an x-ray examination. Most often, specialists encounter bone fractures as a result of accidental injuries or when heavy objects fall on the hand.
Fractures of the metacarpal bones are open and closed, with and without signs of displacement, multiple, single, intra-articular and extra-articular. They can be combined with damage to other structures of the hand. Medical tactics are selected individually, based on examination data, taking into account the patient’s general well-being, his age and the nature of the injury. Diagnosis of hand injuries includes taking a medical history and conducting certain diagnostic tests. During the examination and communication with the patient, the doctor finds out the approximate time of injury, the patient’s complaints, and determines the presence or absence of motor restrictions.
Diagnostics
The diagnosis is made on the basis of the patient’s complaints, anamnestic data (indicating injury), the results of an objective examination with an assessment of the dynamics of the evolution of clinical symptoms, as well as x-ray examination in two or three projections.
According to the protocol adopted by traumatologists, radiography is performed twice: before the start of treatment and after the results of the reduction.
According to statistics, the most informative are lateral projections.
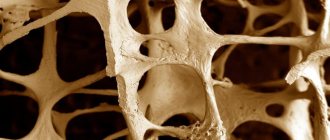
The disadvantage of x-rays is to identify a bone fracture or ligament tear. To clarify the diagnosis, MRI (magnetic resonance imaging) is used to identify bone fractures, blood clots, ligament ruptures, foci of necrosis and osteoporosis. If MRI is not possible, CT or ultrasound are used, which are less accurate.
© DragonImages - stock.adobe.com
Bruises of the hand
Classic contusion of the soft tissues of the hand occurs very often in the practice of traumatologists. It is accompanied by redness of the tissue, moderate pain and swelling, and a local increase in temperature. and no serious treatment is required in this case. Specialists limit themselves to local anesthetics that help quickly relieve swelling and relieve pain.
If, in addition to a bruise, a violation of tissue integrity is detected, it is necessary to use antiseptics, and, if necessary, antibacterial agents. This will prevent the spread of infection. In some cases, it is necessary to immobilize the limb until the diagnosis is clarified.
The quality of primary antiseptic treatment directly affects the purity of infectious complications. Many patients do not pay attention to the need to disinfect the injury site before meeting with a traumatologist. After treatment with an antiseptic and applying a bandage, it is recommended to apply dry cold to reduce the risk of bleeding and the formation of a large hematoma.
Treatment
Depending on the type and severity, reduction can be carried out under local, local anesthesia or general anesthesia (to relax the muscles of the arm). In children under 5 years of age, reduction is always carried out under anesthesia.
Closed reduction of dislocation
An isolated wrist dislocation can easily be reduced by an orthopedic surgeon. The algorithm of actions is as follows:
- The wrist joint is stretched by pulling the forearm and arm in opposite directions, and then realigned.
- After reduction, if necessary, a control X-ray is taken, after which a plaster fixing bandage is applied to the area of injury (from the fingers to the elbow), the hand is set at an angle of 40°.
- After 14 days, the bandage is removed, moving the hand to a neutral position; If a repeated examination reveals instability in the joint, special fixation is performed with Kirschner wires.
- The hand is fixed again with a plaster cast for 2 weeks.
Successful reduction of the hand is usually accompanied by a characteristic click. In order to prevent possible compression of the median nerve, it is recommended to periodically check the sensitivity of the fingers of the casted hand.
Conservative
If closed reduction is successfully performed, conservative treatment begins, which includes:
- Drug therapy: NSAIDs;
- opioids (if NSAIDs are not effective enough):
- short acting;
- prolonged action;
- therapeutic soft tissue massage;
Surgical
Surgical treatment is resorted to when closed reduction is impossible due to the complexity of the injury and the presence of associated complications:
- with extensive skin damage;
- ligament and tendon ruptures;
- damage to the radial and/or ulnar artery;
- compression of the median nerve;
- combined dislocations with splinter fractures of the forearm bones;
- torsion of the scaphoid or lunate bone;
- old and habitual dislocations.
For example, if a patient has an injury lasting more than 3 weeks, or the reduction was performed incorrectly, surgical treatment is indicated. In some cases, a distraction device is installed. Often, reduction of the joints of the distal row of bones is impossible, which is also the basis for surgical intervention. If signs of compression of the median nerve appear, emergency surgery is indicated. In this case, the fixation period can be 1-3 months. Having restored the anatomy of the hand, the orthopedist immobilizes the hand by applying a special plaster cast for up to 10 weeks.
Dislocations are often temporarily fixed with wires (rods or pins, screws and staples), which are also removed within 8-10 weeks after complete healing. The use of these devices is called metal synthesis.
Rehabilitation and exercise therapy
The recovery period includes:
- ERT;
- massage;
- therapeutic exercises.
© Photographee.eu - stock.adobe.com. Working with a physiotherapist.
Such measures make it possible to normalize the functioning of the musculo-ligamentous apparatus of the hand. Exercise therapy is usually prescribed 6 weeks after injury.
Basic recommended exercises:
- flexion-extension (the exercise resembles smooth movements (slow strokes) of the hand when saying goodbye);
- abduction-adduction (starting position - standing with your back to the wall, arms at your sides, palms on the side of the little fingers adjacent to the hips; it is necessary to move the hand in the frontal plane (in which the wall is behind the back) either towards the little finger, then towards the thumb );
- supination-pronation (movements represent rotations of the hand according to the principle of “carrying soup”, “spilling soup”);
- extension-contraction of fingers;
- squeezing the wrist expander;
- isometric exercises.
If necessary, exercises can be performed with weights.
At home
ERT and exercise therapy are initially carried out on an outpatient basis and are supervised by a specialist. After the patient becomes familiar with the full range of exercises and the correct technique for performing them, the doctor gives him permission to practice at home.
Medicines used include NSAIDs, ointments with an irritating effect (Fastum-gel), vitamins B12, B6, C.
Clinical picture. Symptoms of subluxation of the radial head
Whatever the reason that caused the damage, according to others, the child screams in pain, after which he immediately stops moving his arm and has since held it in a forced position, stretched along the body and slightly bent at the elbow joint.
When you try to force the child to move his arm, he protests and complains of pain in the elbow, and sometimes in the wrist area. When collecting anamnesis, you should always try to understand the mechanism of injury and remember that subluxation occurs when there is a sharp stretch along the axis of the limb. If it is possible to establish the fact of such a sprain, the doctor immediately receives very valuable instructions for diagnosis.
The clinical picture of subluxation of the radial head is always typical. The arm hangs along the body like a paralyzed one, in a position of slight flexion at the elbow joint and pronation. An attempt to make movements in the elbow joint causes the child to cry, since the movements are painful. However, you can carefully perform slow flexion and extension at the elbow, while rotational movements are impossible (pain!). With palpation, it is sometimes possible to determine that pressing on the head of the radial bone is painful, but no visible changes are noted in this area. No pathological changes are visible on radiographs.
Complications
Based on the time of occurrence, complications are divided into:
- Early (occurs in the first 72 hours after injury): limitation of joint mobility;
- damage to nerves or blood vessels (damage to the median nerve is a serious complication);
- congestive swelling of soft tissues;
- hematomas;
- hand deformation;
- feeling of numbness of the skin;
- hyperthermia.
- the addition of a secondary infection (abscesses and phlegmon of different localization, lymphadenitis);
Complications of a semilunar dislocation often include arthritis, chronic pain, and wrist instability.
What happens if you don't get treatment?
Fresh, uncomplicated dislocations respond well to treatment. Doctors can easily adjust them. A person wears a cast for several weeks, and after it is removed, he “develops” the affected hand. At the end of the rehabilitation period, the functions of the injured limb are completely restored. Most patients return to their normal lifestyle, including playing sports and performing precise manual work.
If left untreated, displaced bones begin to “overgrow” with connective tissue. After this, it is impossible to return them to their place. Dislocations that previously could be easily reduced using a closed method become irreducible. In this case, the functions of the hand can only be restored through surgery.
Contracture is one of the complications in the absence of correct treatment.
All complicated dislocations require immediate treatment. If left untreated, they can lead to permanent loss of hand function.
First aid for a dislocated finger
- If there are rings on the knocked-out finger, or at least on this hand, you should try to carefully remove them as quickly as possible. Dislocation very often leads to swelling, in which any compression is dangerous.
- Apply ice and try to keep your hand elevated. This will help reduce swelling, one of the most unpleasant consequences of a sprain. The more successfully you manage to prevent swelling in the first minutes and hours, the faster the hand will restore its functionality.
- If it is possible to press the healthy finger against the damaged one, it is useful to apply a bandage that secures them together.
- If the pain is severe, you can take an analgesic.
- It is imperative to seek medical help - to a traumatologist or surgeon, where a diagnosis will be made to rule out other injuries, the finger will be professionally reset, and treatment will be prescribed.
Consequences of injury
After treatment, the patient will continue to feel the effects of the injury for a long time. The patient may be bothered by periodic pain in the healed joint, but it also happens that they become chronic. This usually happens if the victim does not contact a traumatologist in a timely manner.
The sooner the dislocation was reduced, the greater the chance that the injury will resolve without complications. You should not delay visiting a doctor if an injury occurs. Having received a dislocation of the hand, you need to be examined, since only a traumatologist knows how to treat it.
Dislocations accompanied by compression of nerves or complicated by osteoarthritis are especially dangerous. Such injuries are difficult to treat. The presence of an inflammatory process in the wrist joint makes the rehabilitation process long. Subsequently, the mobility of the hand or fingers may be impaired.
What should be done?
After an injury occurs, an adult should immobilize a limb and seek professional help at an emergency room or the nearest traumatology department.
If signs of dislocation are observed in a child, it is necessary:
- Fix the limb and tape it to the body;
- Apply cold to the site of dislocation;
- If you complain of pain, give painkillers.
It is forbidden to carry out treatment on your own, as there is a serious risk of worsening the situation.
How to make an appointment with a pediatric traumatologist
Our clinic employs qualified doctors who have extensive experience in diagnosing and treating dislocations. Experts will tell you how to significantly reduce risks and protect your child from injury. Modern equipment for diagnosing and treating various types of injuries is available to patients. To make an appointment with a specialist, you can use any convenient method:
- by phone;
- on the clinic website by filling out a special online form.
Also on the website you can find out the cost of the services provided, see a list of available equipment, and choose which doctor you want to undergo treatment with. Contact us, we will always help you and your children!
1.General information
Strictly speaking, the lunate bone in ancient times (and in the modern Latin nosological lexicon) is called “lunar”: os lunatum. However, its crescent shape resembles a crescent moon rather than a lunar disk, and therefore in many languages its name was later transformed into “semilunar bone” (the semilunar bone, le semi-lunaire os, etc.). This is a relatively small carpal bone, which is located at the base of the palm; It is separated from the radius by the scaphoid bone; nearby are the trapezoid and other bones of the wrist joint.
In general, the lunate bone does not differ in anything remarkable, with one exception: of all carpal dislocations recorded in traumatology, the largest share is due to dislocation of the lunate bone. It is located in such a way that, while providing the unique mobility of the human hand, it is also the most vulnerable to “careless” impacts and strains.
A must read! Help with treatment and hospitalization!
Prevention
If a patient is diagnosed with a dislocated hand, how to treat it and how the traumatologist decides. But such injury can be prevented. To do this, it is recommended to adhere to certain preventive measures:
- If you fall, you must avoid landing on outstretched arms.
- If you have to walk on a slippery surface, you should be as careful as possible. You can't rush if the floors are wet or there is ice under your feet during winter.
- It is recommended to carefully select your shoes. Shoes should be comfortable.
- Traumatologists advise strengthening joints and bones. To do this, you need to introduce calcium-rich foods into your diet.
- You should protect yourself during sports competitions. You can use an elastic bandage or special equipment for your hands. This is especially true for sports such as basketball or volleyball.
- In order to avoid frequent falls, it is recommended to strengthen the calf muscles. Experts advise brisk walking.
These measures will help minimize the risk of damage. Prevention of any dislocations and fractures in adults is to prevent the development of this type of injury.
When to see a doctor
Only a doctor can accurately determine the type and severity of damage. Therefore, if a child receives an injury and the symptoms described above appear, it is necessary to immediately consult a traumatologist.
When a patient comes in, the doctor conducts a diagnosis. The initial stage of diagnosis is visual inspection and palpation. During palpation, the traumatologist determines the degree of hand mobility and skin sensitivity, and measures the pulse. This method also makes it possible to identify changes in the shape of the composition and the location of the articular endings. The next stage is hardware research. Most often this is an x-ray. With its help, you can identify damage to internal tissues that was caused by a dislocation.
Why is it so important to treat sprains right away?
Many patients do not understand why it is necessary to treat a dislocated finger by a traumatologist immediately after the injury? If the joint is not adjusted in time, it will remain deformed. As a result, the functional ability of the finger will be impaired and you will not be able to produce the range of movements to which you are accustomed.
Old dislocations that occurred more than 2-4 weeks ago are not subject to classical treatment. The head of the joint moves relative to the glenoid cavity and pinches the soft tissue. Therefore, such a displaced joint can only be realigned through surgery.
If a dislocated finger occurs as a result of a fall or blow, then soft tissue is often damaged and without qualified treatment the risk of wound infection increases sharply. With properly selected therapeutic measures, the patient quickly recovers: pain disappears, swelling decreases, and the range of physical activity gradually expands. Restoration of lost hand functions continues for several months. At this time, specialists prescribe local painkillers that suppress pain and relieve signs of inflammation and swelling from damaged tissues.