The joints do not have a direct blood supply. Their nutrition is provided by synovial fluid. It is a thick but elastic substance that reduces friction and prevents wear and tear of cartilage. Lack of fluid in the knee joint leads to a deterioration in the functions of the musculoskeletal system in general. There is creaking, clicking, and morning stiffness. Over time, intense pain in the knee develops, and degenerative changes increase. Without timely treatment, a person experiences difficulty moving. The quality of life deteriorates significantly, even to the point of disability.
Fluid in the knee joint: causes and treatment
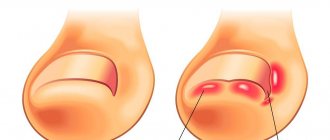
Knee diarthrosis is the second, after the hip, in size and importance in the human body. When moving, it takes on the entire weight of the body, therefore it is susceptible to wear, destruction and injury like no other. Traumatologists daily encounter knee problems in patients caused by illnesses and injuries, stress and falls. One of the serious problems is considered to be synovitis - the collection of effusion in the diarthrosis cavity. And if there is additional swelling, pain and swelling, we can say with complete confidence that excess joint fluid has accumulated in it. The special term “synovitis” itself comes from the direct name of the lubricating thicket of the joints – synovium. It is considered a rather dangerous disorder, and in case of it it is better not to postpone a visit to the clinic. It won’t hurt to figure out why synovitis occurs, how to fight it, what measures to take and what it threatens.
Classification
The fluid that accumulates in the joint cavity can be classified by its nature into exudate and transudate. Accordingly, exudate is associated with the occurrence of inflammatory processes and comes in several types:
- Serous.
- Purulent.
- Hemorrhagic.
- Frail.
Transudate is formed for other reasons that are not related to inflammation, but are associated with circulatory disorders and other abnormalities.
Signs that synovial mass is accumulating in the limbs
If fluid collects in the knee joint, symptoms vary depending on what disease is causing the synovitis. But there are so-called general symptoms:
- swelling in the area of diarthrosis of varying degrees;
- redness;
- local swelling;
- increase in the size of the knee relative to the second;
- pain of various types;
- restriction of movement, it becomes difficult and painful to move the leg;
- compaction palpated in the joint area; in the popliteal region;
- temperature;
- chills.
Of course, it is impossible to determine synovitis based on the last three signs. They are taken into account only if there are others, more “closer” to the knee - local edema, swelling, etc. Signs of this pathology tend to appear not immediately after an injury or illness, but after several hours or even days.
A complex approach
Lack of fluid in a joint is an alarming phenomenon. The condition requires urgent intervention. Our clinic specialists will conduct a thorough diagnosis and develop an individual program for each patient. In our work we are guided only by innovative knowledge and methods. Among the procedures:
- PRP therapy;
- acupuncture;
- hardware physiotherapy;
- joint puncture (if indicated).
Themes
Joints, Pain, Treatment methods Date of publication: 02/02/2020 Date of update: 02/02/2020
Reader rating
Rating: 5 / 5 (1)
Reasons why synovitis may develop
Limbs are often injured and suffer from excessive stress of various origins. And they react to some injuries by accumulating fluid in the knee joint. Treatment will depend on what exactly caused the synovitis. Among the traumatic root causes of its formation are: fractures of the components of the articulation, ruptures or other damage to the diarthrosis ligaments, internal hemorrhage in it, and meniscal injury. Diseases that cause the accumulation of synovium may be the following:
- arthritis
is an inflammation of diarthrosis caused by injury, infection, immune disorder, permanent stress, mental trauma. It often occurs in people who are overweight, sedentary, eat poorly and live in environmentally unfavorable areas; - bursitis
– occurs after injury and infection. With bursitis, the synovial bursa becomes inflamed, the dysfunction of which causes the accumulation of effusion. Bursitis most often affects those who, by profession, frequently and heavily load certain groups of diarthrosis; - arthrosis
– occurs as a consequence of natural aging or injury. There are two stages of arthrosis: the first - when the volume of the lubricating mass decreases and the joint suffers from its insufficiency, and the second - when the volume, on the contrary, increases excessively and entails swelling of the affected area.
Inflammatory processes leading to the accumulation of water can be of three types:
- Immune .
Excess fluid produced appears due to damage to connective tissues.
Purulent.
Negative microorganisms penetrate into diarthrosis and begin to multiply there.
In addition, the cause of purulent lesions is sometimes penetrating local wounds. Aseptic.
With them, there are no purulent elements or pathogenic organisms in the synovium. Such inflammations appear as a result of a knee injury, the spread of an acute viral infection throughout the body, reactive arthritis, or excessive hypothermia. It can also be a consequence of the accumulation of metabolic products in the joint capsule.
Diagnostics
A simple examination by a doctor is not enough to make a diagnosis. However, anamnesis and palpation allow the specialist to draw preliminary conclusions. The condition requires a complex of studies, including instrumental and laboratory techniques.
To assess damage to the joint capsule and knee joint, use:
- Clinical and laboratory diagnostics
. Determination of the level of leukocytes, as well as the release of C-reactive protein, makes it possible to identify the fact of inflammation and determine its intensity. Additionally, specific studies are indicated: for rheumatoid arthritis (ACCP, rheumatoid factor), for ankylosing spondylitis (HLA-27B) and others. General blood and urine samples are indicated. - X-ray
. Allows you to examine the condition of the knees and identify some of the root causes: sacroiliitis, osteoporosis, arthritis. In most cases, radiography is not enough to obtain the correct result. The result does not contain soft tissue data. - Ultrasound diagnostics
. A safe non-invasive method that allows you to study the joint, ligaments, cartilage and bursae. Allows you to detect pathologies in the early stages. - MRI of the joint
. The advantage of the technique is the assessment of the state of the joint not only from the outside, but also from the inside. It has a minimal list of contraindications. It is considered the most informative diagnostic tool. - CT
. Allows you to obtain an accurate image superior to X-rays. For objectivity of the result, it is sometimes performed with contrast. The injection of a contrast agent helps detect even small changes. - Goniometry
. Allows you to evaluate the range of motion of the joint, which has changed due to lack of fluid.
What role does the synovia perform?
The knee contains a synovial membrane - a strong and impenetrable substance that envelops and covers the bone tissue and tendons. The synovial mass in knee diarthrosis plays the role of a protector against aging and rapid wear due to constant friction. The membrane cells secrete this liquid and it covers the entire surface of the diarthrosis and prevents the rubbing of its elements. If there is a lot of this lubricant or, conversely, a little, this is considered a pathology. Important: any disturbances in the production of joint secretions can be detrimental to the health of diarthrosis and require immediate treatment.
What to prepare for: are there any complications?
Products based on hyaluronic acid sometimes cause unwanted reactions:
- itching and heat at the injection site;
- skin irritation;
- hives;
- swelling of soft supra-articular tissues;
- soreness in nearby muscles;
- numbness and tingling in the limb (during the treatment of gonarthrosis);
- local inflammatory reactions;
- rarely – anaphylactic shock.
Each body responds to therapy individually, so it is impossible to be 100% sure of the success of treatment. Injections should be carried out in a medical office, under the supervision of a specialist. The procedure is technically different from standard intramuscular injections and is performed under ultrasound guidance. It should be done by a rheumatologist or orthopedic traumatologist with the appropriate skills.
Prostheses are most often inserted into the knee, hip and shoulder joints
What to do if effusion accumulates, how to treat it?
First of all, it should be taken into account that whatever the reason for the fact that water accumulates, recovery is not limited to just taking pills or just surgery. A comprehensive treatment is always carried out to achieve the most favorable result. At the moment, there are two ways to eliminate the problem - surgery and a conservative method. The conservative (non-surgical) method is treatment with tablets and dietary supplements, manual therapy, massages, physical therapy. Based on the doctor’s assessment of the degree of complexity and advanced stage of the disease, the most appropriate of these two methods is prescribed. Even if surgical intervention is proposed, it may be preceded by a conservative one aimed at relieving pain and stopping inflammation, in the presence of which surgical measures cannot be started. After surgery, massages, physical therapy and vitamin support are usually prescribed, which contribute to the development of the joint, the formation of general and local immunity and the establishment of metabolic processes in tissues. The intervention itself proceeds as follows:
- 1. A specially designed needle is inserted into the problematic diarthrosis. 2. Using a needle and syringe, the accumulated biomass is removed from the knee area. 3. After this, the medicinal substance is administered. This is done in order to avoid infection and the development of inflammation. Typically this procedure is performed without the use of anesthesia.
The conservative method is carried out using immunostimulating therapy, anti-inflammatory therapy, reflexology, physiotherapy, massage and manual therapy, and therapeutic exercises.
Immunostimulating therapy consists of taking a course of special drugs that strengthen the immune system, vitamin complexes, calcium and general strengthening medications. Anti-inflammatory therapy consists of a course of drugs depending on the causes of the disease and the use of local remedies - gels and ointments that prevent inflammation. Pharmacopuncture may also be prescribed if necessary. Reflexology, or acupuncture, is the effect of acupuncture on the foci of the disease, in which biologically active points of the body are stimulated. Reflexotherapy effectively improves blood circulation and metabolic processes, saturates tissues with oxygen, relieves spasms of blood vessels and muscles, and helps relieve inflammation. Physiotherapy is carried out using electromagnetic influence, hydrotherapy, heat and cold. People with fractures or bursitis need to ensure immobility - immobilization - of the affected joint. To do this, they are given a plaster cast. If synovial thickening accumulates due to injury, the patient is prescribed an antibiotic and the damaged area is treated with an antiseptic. These measures are taken to avoid the onset of a purulent or infectious disease. Chronic diseases that tend to recur cannot be cured completely, of course, but remission can be maintained through constant medication, diet and a set of therapeutic exercises. In addition, such a patient should regularly attend health courses in a sanatorium. When effusion collects in the cavity of the knee joint, this is a very alarming bell that cannot be ignored and left to chance. Therefore, self-medication is unacceptable.
And folk remedies can be used only after consultation with a doctor and only as additional supportive therapy, and not an independent course.
Manufacturers of synovial fluid prostheses based on hyaluronic acid
| The product's name | Manufacturer country |
| Fermatron | Great Britain |
| Synvisc | USA |
| Hyalurome CS | Romania |
| Sinokorm | Austria |
| Visco Plus | Sweden |
| Go-on | Ireland |
| Ostenil | Germany |
| Giruan-Plus | Korea |
| RusVisk, Giastat | Russia |
Preparations based on hyaluronic acid have very different effects. How these drugs differ from each other, how effective drugs from different manufacturers are - the opinion of a specialist, supported by the arguments of evidence-based medicine:
How to treat the accumulation of effusion in the knees with folk remedies?
Popular traditional medicine recipes for treatment include bay leaf oil, comfrey ointment and rye decoction.
Bay leaf oil
Rub the sore spot with this oil three times a day until it heals. In order to prepare bay oil at home, you need to take a couple of tablespoons of dried bay leaves and a glass of vegetable oil, mix and leave for a week.
Comfrey ointment
Rub the leg with this ointment twice a day, after which an elastic bandage is applied. To make the ointment, a glass of chopped comfrey grass is mixed with 200 grams of lard and left for five days.
Rye decoction
The decoction is prepared very simply: take half a glass of rye grains per liter of water and boil them for 20 minutes.
Cool the broth and pass through cheesecloth. Add half a kilogram of honey, 200 grams of vodka and 2 teaspoons of barberry to the cold rye broth. Mix the mixture thoroughly and place in a dark place for three weeks. Take 2 tablespoons on an empty stomach three times a day. Treatment of synovial deficiency
When there is little lubricating secretion in the knee, it is just as bad as having it in excess. In people of different ages, synovia is produced from the aqueous phase contained in the blood, proteins and hyaluronic acid, which provides it with the necessary viscosity. So, it resembles blood plasma. With the difference that there is no hyaluron in the plasma and the protein level is higher. The synovial mass is thick, transparent with a yellowish tint.
When there is not enough of it, bones and cartilage begin to rub against each other, which provokes their destruction and accelerates wear. This is accompanied by discomfort, crackling in diarthrosis, pain and decreased mobility. It is designed to envelop its cavity from the inside, nourish the cartilage, protect the surfaces of the bones from wear, and promote their mobility. If it is produced in insufficient quantities, this may be a consequence of:
- disturbances in its production;
- development of helminths in the body;
- infections that dehydrate the body;
- decreased immunity;
- poor nutrition, lack of nutrients for tissues;
- insufficient water consumption;
- inhibition of hyaluronic acid production in older people;
- excessively active physical activity, during which the volume of the synovium simply does not have time to recover.
If there is no fluid in the knee joint, what to do, what foods to introduce into the diet and how to restore its production with medication? The easiest way to restore sufficient production of lubricating mass in diarthrosis is to improve nutrition and saturate the menu with products that contain collagen. Such products include jelly, jellied meat, jellied meat, chicken broth, grapes, and potatoes. Medicinal recovery by taking chondroitin and glucosamine is also possible. If it is impossible to restore the production of lubricant internally for one reason or another, doctors resort to introducing an artificial replacement directly into the patient’s leg.
To whom are they shown?
Since 2003, WHO has officially recommended the use of hyaluronic acid-based drugs for the treatment of mild and moderate forms of osteoarthritis. Most often, this technique is used when conservative methods are ineffective.
The main indications for the use of prostheses are degenerative and post-traumatic diseases of the joints (arthrosis, osteoarthritis, arthrosis deformans), which are accompanied by painful discomfort and stiffness.
For the purpose of prevention, injections are prescribed in order to stop the progression of destructive processes in cartilage, when age-related changes in the joints lead to a deficiency of natural lubrication.
Synovial fluid prostheses are a real godsend for older people
Lateral patellar fold
Schematic representation of the anatomical structures of the lateral recess of the knee joint (normal)
The lateral patellar fold is the most rarely encountered fold of the knee joint. Most often, it has a longitudinal shape, is very thin and is located 1-2 cm lateral to the patella. The lateral patellar fold originates on the lateral wall and is attached to the infrapatellar fat body. S. Ogata and HK Uhthoff hypothesized that rare persistence of the lateral patellar fold is associated with lateral displacement of the patella, leaving no room for it in the lateral recess. The lateral fold may make it difficult to perform knee arthroscopy through the anterolateral approach.
The lateral patellar fold should not be confused with the more commonly encountered pterygoid, superolateral, and transverse arcuate folds.
The arrows indicate: in Figure A - lateral patellar fold (white thin arrow), lateral pterygoid fold (black thin arrow), transverse arcuate fold (black thick arrow); in Figure B - superolateral fold (white thick arrow).
The lateral pterygoid fold is located close to the patella along the outer wall, the superolateral fold is a type of suprapatellar fold dislocated outward. A transverse arcuate synovial fold is often found at the junction of the vertical and anteroposterior portions of the lateral recess.
Mediopatellar fold
The mediopatellar fold is also called the medial fold, synovial patellar fold, pterygoid fold, patellar meniscus, and synovial protuberance. The mediopatellar fold begins in the area of the medial wall of the knee joint, goes obliquely downwards and is woven into the synovium around the Hoffa fat pad. It can be connected to the suprapatellar fold, but more often it has a separate attachment. If overdeveloped, the mediopatellar fold may extend to the medial surface of the femoral trochlea and the medial facet of the patella.
MR tomograms, axial plane, proton-weighted mode with signal suppression from adipose tissue
J. Sakakibara, based on the shape and size, identified 4 types of mediopatellar folds:
- type A – the fold is represented by a linear rope-like protrusion of the synovial wall;
- type B – the fold is represented by an elongated linear cord with uneven contours, but does not reach the medial condyle of the femur;
- type C – the fold is elongated, thickened, with uneven fringed contours, extending to the area of the medial condyle of the femur.
- type D – the fold extends to the area of the medial condyle of the femur, is thickened, uneven, and has a central defect (fenestrated fold).
This classification has received universal recognition and approval, as it is easy to use and clinically relevant. Types A and B of the mediopatellar fold are asymptomatic. Types C and D may impinge between the medial femoral condyle and the patella with subsequent thickening and induration, damaging the cartilage at the patellofemoral joint. The main mechanism of action of the fold is compression of the articular cartilage of the medial facet of the patella during flexion and the patellar surface of the medial femoral condyle during extension. A number of authors are of the opinion that the fenestrated mediopatellar fold (type D) more often causes damage (impingement) of the articular cartilage of the medial parts of the patellofemoral joint.
For visualization of the mediopatellar fold using MRI, T2- or proton-weighted images in the sagittal and axial planes with or without fat suppression are considered the most informative. The mediopatellar fold has a low MR signal and is easily recognized in a typical location against the background of a small amount of intra-articular fluid. On the other hand, one should always pay attention not only to the size of the fold and its location relative to the medial condyle, but also to the condition of the articular cartilage in the medial facet of the patella, femoral condyle, and the patient's complaints. With massive intra-articular effusion, lateral displacement of the fold may occur, complicating the differential diagnosis of types B and C. The large size of the mediopatellar fold may make it difficult to examine the medial parts of the joint during arthroscopy.
Comparison of natural and artificial hyaluronic acid by molecular weight
| GK type | Molecular weight (MM) | Characteristics |
| Natural | 3 140 000 Yes | Constantly updated, normally has excellent shock-absorbing and lubrication properties |
| Artificial with low mm | 500,000 – 800,000 Yes | It is quickly removed from the joint, therefore it requires a large number of injections and frequent repetitions of courses |
| Artificial with medium mm | 800,000 – 2,500,000 Yes | The standard course includes 5 injections, lasts a relatively short time, and is used most often |
| Artificial with high mm | More than 2,500,000 Yes | Requires fewer injections per course and lasts longer |
Infrapatellar fold
The infrapatellar fold, or ligamentum mucosum, is the most common fold of the knee joint. Its formation occurs from 8 to 12 weeks of gestation and depends on the degree of involution of the primitive embryonic membrane separating the medial and lateral sections of the joint. The shape of the fold formed the basis for its arthroscopic classification by S. Kim and W. Choe:
- 0—no fold;
- 1 - complete persistence of the fold, the fold is separated from the anterior cruciate ligament;
- 2 - complete persistence of the fold, the fold is separated from the anterior cruciate ligament and has several bundles;
- 3 - vertical fold - complete persistence of the fold, which is associated with the anterior cruciate ligament and divides the joint cavity into medial and lateral sections;
- 4 - fenestrated vertical fold - a vertical fold with a hole/defect.
The infrapatellar fold begins in the anterior parts of the intercondylar recess of the femur, expands forward and downward, and attaches to the lower pole of the patella. The thickness of the fold varies widely from submillimeter to the size of the anterior cruciate ligament.
The infrapatellar fold is easily identified on sagittal MR images as a linear, hypointense structure running through the Hoffa fat pad in a plane parallel to the anterior cruciate ligament. In some cases, especially in patients with complete rupture of the anterior cruciate ligament, a well-developed infrapatellar fold can simulate its preserved bundles. It is also necessary to carry out a differential diagnosis of the infrapatellar fold with local nodular synovitis, postoperative changes and a loose body in the area of the Hoffa fat pad. The awareness of radiologists about the existence of this anatomical structure allows in most cases to make the correct diagnosis.