Dislocation of the acromial end of the clavicle is a fairly common injury. It is known that Hippocrates was the first to separate the concepts of “shoulder dislocation” and “dislocation of the acromial end of the clavicle,” which before him were considered the same injury. Of course, from a layman's point of view, these two problems at first glance are not different from each other and are perceived simply as a “shoulder injury” or the expression “knocked out shoulder” is often heard. We specifically made such a philological digression so that you understand that injuries to the shoulder joint and adjacent structures are a separate and very complex area in traumatology. For example, one of the best medical books devoted only to the shoulder joint and its surrounding structures is a two-volume book with 1704 pages! Therefore, in case of injuries to this area, it is extremely important to be treated by a competent specialist.
A little anatomy
The clavicle is a small, S-shaped curved tubular bone, which at one end connects to the sternum (sternoclavicular joint) and at the other end to the acromial process of the scapula (acromioclavicular joint). Traditionally, the clavicle is divided into three parts: the sternal end, the diaphysis (middle part) and the acromial end.
The main injuries to the collarbone are fractures and dislocations. Since the clavicle has two ends (acromial and clavicular), dislocations can occur at both the acromial and sternal ends. More often there are dislocations of the acromial end. Several ligaments are attached to the collarbone, which connect it to the scapula.
Why does clavicle dislocation occur?
A classic example of an injury in which the acromial end of the clavicle is dislocated is a fall on the shoulder. In this case, the ligaments connecting the collarbone and scapula are torn, and after this, the collarbone moves upward under the influence of muscle traction.
Of course, since there are several ligaments attached to the collarbone, various options for their rupture are possible. For example, only the capsule of the acromioclavicular joint may rupture - in this case, dislocation will not occur or there will be subluxation, since other ligaments will hold the collarbone. If other ligaments (conical and trapezoidal ligaments) are torn, the clavicle will dislocate.
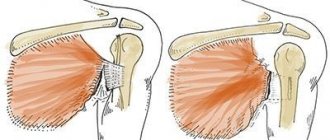
Dislocation of the acromial end of the clavicle: on the left – incomplete (subluxation), the coracoclavicular ligament is intact; on the right - complete, the conical and trapezoid ligaments, which form a single coracoclavicular ligament, are torn.
We have described the simplest classification, but in reality everything is much more complicated. Among specialists involved in the treatment of shoulder injuries, it is customary to use the Rockwood classification, which distinguishes six types of dislocation.
Dislocation of the sternal end of the clavicle[edit | edit code]
Dislocations of the sternal end of the clavicle are a fairly rare injury caused either by a blow from the side to the shoulder or a fall on an abducted arm (the cause primarily of anterior dislocations), or a strong blow from the front to the clavicle (the cause of posterior dislocations). The severity of the injury ranges from a sprain with mild subluxation of the clavicle to rupture of the ligaments and capsule and complete dislocation of the clavicle.
Anterior dislocation of the sternal end of the clavicle[edit | edit code]
Main features
- There is a history of trauma to the upper chest.
- At the site of the sternal end of the clavicle there is a painful tumor.
- X-rays and CT scans of the chest show a dislocated clavicle.
Clinical picture
The anterior dislocation of the sternal end of the clavicle occurs more frequently than the posterior one. When examining the victim, attention is drawn to a tumor at the site of the sternal end of the affected clavicle. It is not easy to confirm such a dislocation radiographically because the converging sternum, clavicle and rib obscure the sternoclavicular joint; you have to take pictures in an oblique projection. If, despite normal chest x-rays, the suspicion of a dislocation remains, it is worth resorting to a more sensitive diagnostic method - CT.
Treatment
Usually the symptoms quickly go away on their own, and the mobility of the shoulder joint is not affected. As for the reduction of the sternal end of the clavicle, there is lively debate about this. Existing operations are accompanied by a fairly high risk of complications, and after closed reduction of the clavicle it is difficult to keep it in the desired position.
Posterior dislocation of the sternal end of the clavicle[edit | edit code]
Main features
- There is a history of trauma to the upper chest.
- Pain in the area of the sternal end of the clavicle.
- Hoarseness, difficulty breathing and swallowing may occur.
- X-rays and CT scans of the chest show a dislocated clavicle.
Clinical picture
Posterior dislocation of the sternal end of the clavicle is much less common than the anterior one, but it is incomparably more dangerous, since it can be accompanied by injuries to the trachea, esophagus and great vessels. Symptoms range from mild to moderate pain at the sternal end of the collarbone to hoarseness, difficulty breathing and swallowing, and subcutaneous emphysema (when the trachea ruptures).
Treatment
Early closed reduction of posterior dislocation of the sternal end of the clavicle usually gives a stable result. To perform the reduction, a pillow is placed under the shoulders of the patient lying on his back, after which the straightened arm is retracted 90° and pulled towards himself, and if this is not enough for reduction, then the assistant, grasping the collarbone with his fingers or a sterile linen clamp, pulls it forward. In exceptional cases, closed reduction under general anesthesia or open reduction is required.
After reduction, the patient is given a splint and is recommended to apply ice to the collarbone and take NP VS orally to relieve pain. After 2-3 weeks, when the sternoclavicular joint has healed sufficiently, you can begin exercises to develop the shoulder joint. You can raise your arm no earlier than 3 weeks after the injury.
Symptoms of dislocation of the acromial end of the clavicle
Immediately after the injury, pain occurs in the shoulder girdle. If the dislocation is complete, then the collarbone sticks out, and, in some cases, it is possible to identify the symptom of a piano key: when you press on the collarbone, it is set instead (sinks down), but if you stop the pressure, it will immediately dislocate again. The absence of a key sign does not mean that everything is fine with the collarbone. Firstly, this symptom is not always easy to check due to the fact that in some patients pressing on the collarbone causes severe pain. Secondly, swelling occurs several hours after the injury. Thirdly, in obese people the collarbone may generally be poorly contoured.
When the acromial end of the clavicle is dislocated, the function of the arm is impaired - most often it is impossible to raise the arm above the shoulder or move the arm to the side.
A bruise appears around the collarbone (it is mistakenly called a hematoma, but in fact it is just a bruise - the subcutaneous fat is saturated with blood from the torn ligaments). Over the course of several days or even weeks, this bruise may increase in size and “slide” down.
The pain usually decreases within a few days, but we advise you not to wait, but to consult a doctor immediately.
Salter-Harris fractures of the sternal end of the clavicle[edit | edit code]
in athletes under 25 years of age, instead of dislocations of the sternal end of the clavicle, fractures passing through the proximal epiphyseal cartilage may occur. Clinically, such fractures (especially mixed ones) resemble dislocations and are treated conservatively. Further growth of the clavicle, as a rule, is not affected, and repositioning of fragments (unless there is a strong displacement) is not required; It is enough to prescribe painkillers. Sometimes parents discover a dense mass formation near the sternal end of the clavicle in their child and, fearing a malignant tumor, consult a doctor. When collecting anamnesis, it turns out that the child suffered an injury several weeks before, and the mass formation is just a callus at the site of a healing clavicle fracture, which is confirmed by x-ray.
Literary sources
Battaglia TC et al: Interposition arthroplasty with bone-tendon allograft: a technique for treatment of the unstable sternoclavicular joint. J Orthop Trauma 2005; 19(2): 124.
Diagnosis of dislocation of the acromial end of the clavicle
The diagnosis of dislocation of the acromial end of the clavicle is sometimes very simple and everything is obvious upon examination, and sometimes you have to solve a whole puzzle. The most optimal and common diagnostic method is radiography. It is worth saying that, just as there are no identical people, there are no identical collarbones. Most often, the cause of a false diagnosis is the individual characteristics of the acromioclavicular joint.
Therefore, it is advisable to perform an x-ray of not one shoulder, but two at once - which will allow us to assess the normal structure of the opposite clavicle.
In doubtful cases, functional radiography is sometimes performed - a weight is placed in the arm, which pulls it down and the dislocation becomes more obvious.
Clinical picture
Read more…
The leading symptom of a dislocation is pain in the acromioclavicular joint. The victim usually presses his hand to the body. It is better to palpate the collarbone in its middle third - in this case, you can be sure that if pain appears at the acromial end, it is not caused by pressure on the bruised soft tissue. With complete dislocations, when examining the area of the damaged shoulder girdle, one notices a step-like protrusion of the collarbone and sharp pain. A “key” symptom is noted: when pressure is applied to the acromial end of the clavicle, it lowers, and when the external influence stops, it rises again.
To confirm and clarify the diagnosis, radiography of the shoulder joint is necessary. It is carried out in direct and axial projection. More informative are radiographs performed using the Zanca technique or functional radiographs. Functional radiographs are taken in a standing position after a 3–5 kg load is fixed to both arms. Both shoulder girdles are removed, preferably on the same x-ray film.
The presence of a subluxation or dislocation is indicated by a displacement of the lower contour of the clavicle in the articulation area upward in relation to the corresponding contour of the acromion process.
With a displacement of up to half the thickness of the clavicle, one can think of a subluxation; with a greater displacement, one can think of a dislocation. For a more reliable assessment of dislocation, it is necessary to evaluate in a comparative aspect the distance from the coracoid process to the clavicle (i.e., the length of the coracoclavicular ligament). An increase in this distance in comparison with the healthy side by 5 mm or more indicates a rupture of the coracoid ligament, and therefore a complete dislocation of the clavicle (complete rupture of the articulation).
Treatment of dislocation of the acromial end of the clavicle
The optimal treatment method depends on the type of dislocation. Previously, in the vast majority of cases, conservative treatment was used, that is, they did not operate. The essence of this treatment was that for several weeks the patient was shackled in bulky and heavy devices that realigned and held the collarbone in the desired position.
Now conservative treatment is indicated for incomplete dislocations (subluxations), i.e. with type 1 or 2 dislocation according to Rockwood. In this case, a light, aesthetic and comfortable sling bandage is sufficient, which is worn for 3-5 weeks, depending on the type of damage to the capsule of the acromioclavicular joint. Next, a control X-ray is performed and a decision is made about rehabilitation - the bandage is removed and physical exercises begin.
On the first day after the injury, cold is applied, which reduces swelling and pain. Immobilization with a sling bandage in itself will significantly reduce the pain, but if it remains, you don’t need to endure it, tell your doctor about it and he will prescribe painkillers.
Subsequently, according to the doctor's decision, the sling bandage can be replaced with tape, which allows you to use the arm, but holds the collarbone. The tape bandage should only be applied by a specialist. For type I injuries, the tape bandage can be used from the very beginning.
Prevention of scoliosis
To ensure that the spine remains straight and all parallel bones/limbs of the body are positioned correctly, preventive measures should be taken from an early age.
- Maintain good posture both when walking and while sitting. Correct it if the slightest violations are noticed in the early stages.
- Avoid carrying excessive weights. Especially in one hand or on one shoulder.
- When sitting for a long time, your legs (knee bend) should form a 90-degree angle. The back remains straight. Every 15-20 minutes you need to get up and stretch.
- It is important to strengthen your back and abdominal muscles. Therefore, daily gymnastics is mandatory.
- You should lead a normal active lifestyle. Hiking, running, swimming, cycling will do excellent service to the spine. Refusal of prolonged sitting, standing, and excessive loads.
- It is advisable to take a general massage course at least once a year.
- Watch your weight. In thick, obese people, the load on the joints and spine increases significantly.
- If you experience prolonged discomfort in your back, you must seek qualified help in a timely manner.
Following these simple rules will keep your spine strong and healthy. At the same time, a girl, a man, a teenager, and a child will always be able to walk beautifully.
Surgical treatment of dislocation of the acromial end of the clavicle
Before we talk about operations, we need to talk about why to operate at all. As we have already noted, with types 1 and 2 of dislocation, conservative treatment is indicated, since there is nothing to be done to operate (with rare exceptions) - the collarbone is already in place. But with type 3 dislocation, when the collarbone is completely pushed up, it is necessary to consider the possibility of surgery. Of course you can - what will happen if you don’t operate? The pain will go away with rest, the hematoma will resolve.
But the following problems are possible:
- Pain on exercise
- Decreased arm strength
An unreduced collarbone will stick out all the time, which is not only a cosmetic problem, but can also limit movement, in particular, the following may occur:
- Limitation of arm abduction, i.e. the arm often cannot be raised above the shoulder.
All these problems can lead to poor posture.
For some, all these possible consequences do not pose any problem at all, since there are people with extremely small physical needs. In any case, the operation to correct the clavicle is not aimed at saving life, so it is necessary to consider the advisability of surgical treatment based on the profession, lifestyle and needs of the patient.
In general, maximum recovery for complete dislocation of the acromial end of the clavicle (types 3, 4, 5 and 6 of dislocations) is possible only with surgical treatment, during which the clavicle is reduced and fixed.
A number of recent scientific studies have shown that for athletes and people with high physical demands, it is advisable not just surgical treatment, but the earliest possible surgical treatment, which allows to obtain the best results.
In most cases, the operation is performed under general anesthesia.
Doctors practice quite a large number of surgical options, but we will focus only on the most minimally traumatic and modern methods. They are the ones that are used in our clinic for surgical assistance.
Conservative treatment
If there are no soft tissues between the articular surfaces of the acromion process and the clavicle, it is easy to set the dislocation with pieces of the ligamentous apparatus and periosteum. To do this, the shoulder is raised, pulled back and at the same time pressed with your fingers on the outer end of the collarbone. However, it is difficult to keep the clavicle in the reduced position until the ligamentous apparatus of the acromioclavicular joint fusions. With conservative treatment, splints and bandages are applied for this purpose for 4–6 weeks, providing long-term pressure on the acromial end of the clavicle. This pressure should be sufficient to achieve reduction, but not so strong as to cause a pressure sore. Such dressings include: Shimbaretsky's thoracobrachial dressing with a compression screw, Pogorelsky's dressing, CITO splint.
If, after removing the bandage, the end of the clavicle remains in the reduced position, the function of the joint is fully restored. At the end of the period, the bandage is removed, and within a week the limb is fixed with a wedge-shaped pillow. After this, rehabilitation treatment is carried out: physical therapy, as well as physiotherapeutic treatment.