Arthrodesis of the ankle joint is a surgical intervention for artificial fusion of the articulating articular surfaces of the ankle in a position that is physiologically advantageous for the functioning of the leg. The main goal of surgical treatment is to provide support to the problem area by completely blocking its mobility (creating ankylosis). Immobilization is achieved by rigidly connecting the adjacent ends of the joint bones to each other with special metal fixators (knitting needles, screws, pins, etc.). This allows the articular surfaces to firmly fuse with each other at the desired angle, that is, to bring the joint into a completely motionless state, which will help the patient get rid of severe pain and instability of the foot.
Example of fusion.
The arthrodesis technique dates back to the very beginnings of the development of orthopedics, and therefore is an outdated tactic for ankle surgery. The discovery of the “joint closure” method dates back to 1887, first proposed by the Viennese surgeon Albert. Operational technical concepts have changed little since that time.
The effectiveness of ankle arthrodesis has a long-standing evidence base, but due to the radical approach and the high incidence of postoperative complications, retro-style intervention is used in the most extreme cases.
Ankle injuries
The main purpose of the ankle joint, formed by the tibia, fibula and talus bones, is to be a reliable support for the musculoskeletal system. This section of the leg must consistently support almost 90% of the total body weight when a person stands or performs any kind of physical activity in an upright position. In addition to supporting functions, the joint provides shock absorption of the limb, various movements of the foot in a normal amplitude:
- flexion;
- extension;
- abduction;
- casting;
- rotation.
The stable functioning of the bone joint is guaranteed by the healthy condition of the ligaments, bones, cartilage, and muscles that form it. If at least one unit of a joint fails, not only its performance is impaired, but also an imbalance in the functions of the entire musculoskeletal system occurs. Diseases of the ankle joint have a detrimental effect on the ability to move, lead to deterioration of gait, and often lead to disability. Often, serious pathologies that may require arthrodesis begin with trivial injuries localized in this area:
- bruises;
- dislocations and subluxations;
- ankle fractures;
- violation of the integrity of the heel bone;
- ligamentous distortion (sprains, tears of ligaments, etc.).
Lesions of a traumatic nature often occur as a result of direct exposure to mechanical force, which is provoked by local impacts, falls from a height, unsuccessful jumps, and sharp rotational turns. After all, sometimes it is enough for a person to simply slip on a slippery surface or trip for damage to the constituent structures of the ankle.
Any traumatic lesions require timely diagnosis and immediate treatment. After a certain period, the injury, if proper medical care was not provided in due time, makes itself felt with serious consequences. Pathologies resulting from an old injury, against the background of imaginary well-being, are manifested by the sudden onset of pain and increasing limitation of the locomotor and support potential. People don’t understand what happened, where the discomfort came from, and the cause turns out to be a past injury.
Remember! Complex degenerative-dystrophic processes, often irreversible, predominantly do not develop on their own, but are diagnosed as a post-traumatic complication. The most common pathologies of post-traumatic origin with a serious progressive course are arthritis and osteoarthritis.
Arthrosis, in turn, is a consequence of arthritis. This is the chain mechanism for the development of a complex clinical situation. It is not difficult to go from injury to deforming osteoarthritis (DOA) in a couple of years. But if the injury is not difficult to treat conservatively, then with arthrosis of the ankle joint everything is different - it is an incurable disease that critically depresses the quality of life and negatively affects the statics and dynamics of the entire limb.
Indications for surgery
Blocking the motor functions of the ankle segment by bone fusion is prescribed when such pathological conditions are identified as:
- secondary (post-traumatic) and primary arthrosis, grade 3-4;
- severe chronic arthritis, including rheumatoid type;
- constant pain in the ankle and/or radiating to the knee joint, which intensifies even with minor loads;
- severe lameness due to joint deformation;
- persistent impairment of the support ability of the foot, expressed by the inability to fully stand on the leg due to weakness of the ankle system, laxity;
- severe flexion-extension contracture of the joint;
- paresis and paralysis of the leg muscles, which developed against the background of polio in the past;
- improperly healed fracture, pseudarthrosis.
Arthrosis of the left joint. The joint space is very small.
Contraindications to ankle arthrodesis
Arthrodesis is not recommended for use in the musculoskeletal segment of the ankle if:
- the patient is at an age when the musculoskeletal system continues to actively grow (surgery is strictly contraindicated before the age of 12);
- fistulas of non-tuberculous origin were found in the joint;
- active infectious and inflammatory processes in the area of proposed intervention or any common infectious diseases in the acute phase have been identified;
- the patient suffers from severe forms of pulmonary, renal or heart failure;
- there is a chronic disease in the stage of decompensation (diabetes mellitus, etc.);
- intolerance to anesthetic drugs was revealed.
Treatment of ankle arthrosis in a specialized medical center
In order not to bring this unpleasant disease to its maximum development, it is important to begin adequate treatment in our clinic as soon as possible. This is a guarantee of its success, efficiency and sustainability. In addition, fewer sessions will be required in the early stages.
You will be prescribed complex therapy. It includes:
- manual practices;
- arthrotherapy – the author’s method without jerks and blows;
- a therapeutic exercise program developed individually;
- massage;
- ankle traction on a special traction table;
- physiotherapy;
- taking chondoprotectors.
Treatment of arthrosis should be accompanied by lifestyle changes - physical activity, weight correction.
Call and make an appointment with us right now - give yourself the gift of health!
Types of surgery
When the wear and deformation of the joint is too severe, this can become an obstacle to replacing the joint block with an endoprosthesis. Therefore, even with every desire, replacing a diseased segment with an artificial analogue is not always feasible. In this and all the situations described above, there is only one way out - to use arthrodesis surgery. It will stabilize the ankle and reduce pain symptoms to a minimum, thereby significantly improving the patient’s quality of life. There are several methods of surgical intervention.
- Intra-articular. During surgery, the joint capsule is opened, followed by removal of damaged hyaline cartilage from the surfaces of the bone elements. After repositioning the bones in an advantageous position, they are fixed with metal devices.
- Extra-articular. Fixation of the bones of the articulation only by placing a bone graft, while the cartilaginous covers are not subject to resection.
- Combined. This technique involves the combination of two methods in one surgical process: intra-articular and extra-articular. Thus, the cartilaginous structures from the joint are completely removed, an autograft is introduced, which is fixed with special metal plates.
- Compression. The operation consists of squeezing the articulating surfaces with a compression or compression-distraction type apparatus for their further fusion. Widely used designs are Ilizarov, Grishin, Volkov-Oganesyan apparatuses. Removal of cartilage is not excluded. Implantation of a bone graft is not required for the compression method.
Technique No. 1.
Preparing the patient for ankle arthrodesis
When planning this type of surgical treatment, it is extremely important to evaluate all joints adjacent to the problem area. This is necessary to understand how capable neighboring segments are of taking on a larger load complex. Since the movement potential of the ankle joint is blocked after surgery, the adjacent movable joints will naturally be subject to more stress. It is especially important to reliably assess the condition of the talonavicular joint, because it is precisely this central segment of the foot that will bear the maximum share of the load. A positive effect from arthrodesis can be counted on only in the absence of degenerative pathogenesis in it.
The go-ahead to operate on a patient is given only after a comprehensive examination confirming the clear need for this medical care in the absence of contraindications. The patient is prescribed a series of diagnostic measures:
- detailed blood and urine tests, including biochemistry;
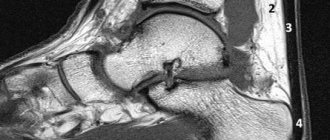
- X-ray, MRI or CT scan of the joint in several planes;
- testing for HIV, syphilis, hepatitis;
- fluorography and electrocardiography;
- examination by highly specialized doctors (cardiologist, pulmonologist, etc.);
- consultation with an anesthesiologist.
In addition, the specialist must additionally make sure that the effect of arthrodesis is most likely to “work” and the patient’s well-being will noticeably improve. To do this, a kind of test is first carried out, which consists of applying a plaster cast to the joint. So, a person walks with his ankle fixed in a cast for about 7 days, and after a week, the orthopedic traumatologist finally determines the feasibility of the operation. If the test immobilization helped to create support for the limb and significantly reduce pain, the operation is performed. If discomfort persists, pain appears or pain increases, or gait worsens, arthrodesis is cancelled.
Technique No. 2.
A week before the expected date of the intervention, the use of drugs with anti-inflammatory effects (NSAIDs) and agents that have blood-thinning properties should be stopped. On the eve of surgery, the diet should be light, stop eating 6-8 hours before.
Attention! Make sure your living space is prepared in advance when you arrive home from the hospital. You should remove carpets, runners and cords from floors that could cause your foot to get caught and fall. Place essential items and things in easily accessible places. In the bathroom it is necessary to lay non-slip mats made of rubber or silicone materials with Velcro, etc.
Preparation for surgery and contraindications
The first consultation is given by an orthopedic surgeon. He examines the sore spot and prescribes additional diagnostics: X-rays, MRI, ECG, fluorography. There are contraindications for ankle arthroscopy, so it is important for your doctor to know everything about your health.
Contraindications are divided into two groups: relative and absolute. Relative contraindications imply pre-treatment. For example, hidden damage to the ligaments and joint capsule or hemorrhage into the joint cavity. This group also includes somatic disorders. For women there is an additional point - the operation is not possible during menstruation.
List of absolute contraindications:
- intolerance to anesthesia;
- cavity fusion;
- purulent infection;
- infectious skin diseases;
- pathologies of the cardiovascular system, diabetes mellitus;
- progressive dystrophic pathology of cartilage tissue;
- HIV, hepatitis;
- herpes;
- colds.
To detect contraindications, you need to consult a general practitioner, who will make a conclusion based on a general and biochemical analysis of blood, urine, a test for the presence of hepatitis and HIV, and the testimony of an anesthesiologist. People who have had a heart attack or stroke need to visit a neurologist or cardiologist.
You will have to prepare for the operation not only mentally, but also physically. A light diet is recommended a few days before surgery, abstinence from alcohol for 10-15 days and complete absence of food 12 hours before the introduction of anesthesia. You need to take care of crutches in advance, because in the first postoperative days, stress on the sore joint is excluded.
Carrying out the operation
Arthrodesis of the ankle joint according to the traditional method is performed under general anesthesia in an open manner. Surgical procedures under arthroscope control can be performed under spinal anesthesia. The session requires an average of 2-3 hours of intraoperative time. Let's consider the principle of classical tactics.
- A pneumatic tourniquet is applied to the lower third of the thigh. Next, access is created by making a linear skin incision along the joint with a scalpel. The incision is approximately 10 cm.
- At the next stage, an opening and reliable supination of the joint is performed, which will facilitate the work with the next manipulations.
- The surfaces of the tibia and talus are then prepared. Preparation includes resection of cartilage tissue with a surgical chisel and removal of ossification.
- Then the foot is removed from the vicious position. The tibial element and the talus component are tightly juxtaposed with each other in a position that is convenient from a physiological point of view. The achieved position is secured by a metal structure of the required type.
- The surgical tracts used are closed at the final stage using layer-by-layer suturing of soft tissues, leaving drainage.
In cases of severe deformity, fibular osteotomy may be used. Extensive bone losses are compensated by grafts - fragments of similar biological material taken from the patient from the iliac crest.
If external fixation systems were used, for example, the Ilizarov apparatus, plaster is not used. When installing internal metal implants, a cast is placed on the operated limb. Until ankylosis occurs, the patient is in a plaster cast. The rate of bone fusion in each individual patient may differ due to the physiological characteristics of the body. The joint is completely fused and immobilized 3-6 months after surgery.
Ankle rehabilitation
After arthrodesis performed in the ankle area, physical therapy classes begin from the first day. They will prevent the development of muscle atrophy, prevent blood clots and prevent congestion in the lungs. With sufficiently long-term immobilization of the limb and a low level of patient activity without adequate physical training, very disastrous results can be achieved.
Surgical sutures.
Exercise therapy in the early period includes breathing exercises, isometric exercises to maintain and strengthen the calf and thigh muscles. The exercises are performed under the supervision of a physical postoperative rehabilitation methodologist. Gymnastics involves gradually increasing the load and introducing new exercises in accordance with the patient’s well-being and recovery time.
Medication treatment is mandatory for rehabilitation, including:
- highly effective therapy against the formation of infectious pathogenesis;
- use of symptomatic drugs;
- use of medications for thromboembolic complications.
From the second day they try to verticalize the patient. Walking is allowed only with the support of crutches, avoiding any load on the operated limb. Not earlier than after the first signs of ankylosis appear, and this is after about 6 weeks, it is allowed to partially include a gentle axial load on the sore leg. The patient will be able to try to walk normally no earlier than after 4-6 months. Removal of metal structures is usually prescribed after 6-12 months. Internal fixators do not always need to be removed.
How is the operation performed?
Ankle arthroscopy is performed under either local or general anesthesia, depending on how large the area being operated on is and how complex the problem is. The operation time also depends on this – from 30 minutes to 3 hours.
The shin is secured with a stand at the required height and several access incisions are made to insert instruments. Just as during shoulder surgery, a saline solution is injected to improve the visibility of the device. The surgeon's assistant stretches the joint space in the ankle so that the doctor can insert the arthroscope.
The image from the device is broadcast on a large screen, allowing you to examine the joint and periarticular space in detail.
At the end of the operation, the joint cavity is cleared of excess fluid introduced initially and filled with a healing solution. The incisions are closed with sutures and a sterile dressing.
Complications of ankle arthrodesis
The incidence of complications after a standard operation with a wide opening of the joint, as clinical experience shows, is an order of magnitude higher than after arthroscopic interventions. Here is some comparative data on negative reactions for two types of procedures (without the use of external fixators) detected during the first 3 weeks:
- phlebothrombosis is detected in 22% of cases after open ankle arthrodesis, in 1.8% after minimally invasive intervention;
- wound infection develops in approximately 12% of patients, while the risks after arthroscopy are practically absent (<0.1%)
- necrosis of surrounding tissues, respectively, in 17% and 0.2%;
- wound hematomas and seromas: 22% and 0.9%.
Persistent swelling.
Intraoperative blood loss after standard arthrodesis is 250 ml, after arthroscopic arthrodesis - about 120 ml. Failure of ankylosis after 6 months is determined in 5%-6% of people who underwent the procedure according to the traditional scenario, and in 0.5%-0.9% of patients who underwent arthroscopy with intramedullary fixation. Skipping the topic of comparison, we note that after any type of artificial ankylosis there are increased risks associated with the formation of arthrosis in other joints of the limb and shortening the leg length to 3 cm.
“I have a deformity of the left ankle joint. I suffer from constant pain. Due to joint instability, I often fall. I do gymnastics, wear special insoles, take non-steroidal anti-inflammatory drugs, chondroprotectors, but the condition of the joint does not improve. What can be done in this case?
This is a fairly common complaint seen by traumatologists. For such patients, the solution to the problem may be an operation that will restore the foot and relieve pain - arthrodesis of the ankle joint. Oleg Kezlya , head of the Department of Traumatology and Orthopedics of BelMAPO, Doctor of Medicine, spoke about it in detail sciences, professor.
Oleg Kezlya, Head of the Department of Traumatology and Orthopedics of BelMAPO, Doctor of Medical Sciences. sciences, professor
The essence of the operation
Arthrodesis of the ankle joint is an operation for artificial fusion of the articulating articular surfaces of the ankle in a position that is physiologically advantageous for the functioning of the leg. The goal is to provide support to the problem area, completely blocking its mobility (creating ankylosis).
Immobilization is achieved by rigidly connecting the adjacent ends of the joint bones to each other with special metal clamps: knitting needles, screws, pins. This allows the articular surfaces to grow together at the desired angle, that is, to bring the joint into a completely motionless state, which relieves pain.
When may arthrodesis be needed?
Common injuries in the ankle joint area can lead to serious pathologies that may require arthrodesis:
- dislocations and subluxations,
- bruises,
- ankle fractures,
- violation of the integrity of the calcaneus and talus,
- ligamentous distortion.
Falls from a height or on a slippery surface, sharp rotational turns, unsuccessful jumps are typical situations that can lead to damage to the structures of the ankle.
Therefore, any traumatic lesions require timely diagnosis and treatment. Old, untreated injuries can result in pain and increasing limitations of locomotor and support potential after a while.
The most common pathology of post-traumatic origin with a progressive course is osteoarthritis. The injury can be treated conservatively, but arthrosis of the ankle joint is an incurable pathology that significantly worsens a person’s quality of life.
Endoprosthesis replacement of a joint block is not always possible. This can be prevented, for example, by severe wear and deformation of the joint. There is only one option left - arthrodesis surgery.
Types of surgery
There are several methods of surgical intervention.
1. Intra-articular. Opening the joint capsule with subsequent removal of damaged hyaline cartilage from the surfaces of bone elements. After repositioning the bones in an advantageous position, they are fixed with metal devices.
2. Extra-articular. Fixation of the bones of the articulation only by placing a bone graft, while the cartilaginous covers are not subject to resection.
3. Combined. A combination of intra-articular and extra-articular methods in one surgical process. The cartilaginous structures from the joint are completely removed, an autograft is introduced, which is fixed with special metal plates.
4. Compression. Compression of articulating surfaces with a compression or compression-distraction type apparatus for their further fusion. Ilizarov, Grishin, Volkov-Oganesyan apparatuses are used. Removal of cartilage is not excluded. Implantation of a bone graft is not required for the compression method.
Indications
- secondary (post-traumatic) and primary arthrosis of the 3rd–4th stage;
- severe chronic arthritis, including rheumatoid type;
- constant pain in the ankle and/or radiating to the knee joint, which intensifies even with minor loads;
- severe lameness due to joint deformation;
- persistent impairment of the support ability of the foot, expressed by the inability to fully stand on the leg due to weakness of the ankle system, laxity;
- severe flexion-extension contracture of the joint;
- paresis and paralysis of the leg muscles, which developed against the background of polio in the past;
- improperly healed fracture, pseudarthrosis.
Contraindications
- age when the musculoskeletal system continues to actively grow (up to 12 years of age, surgery is strictly contraindicated);
- fistulas of non-tuberculous origin in the joint;
- active infectious and inflammatory processes in the area of the proposed intervention or any common infectious diseases in the acute phase;
- severe forms of pulmonary, renal or heart failure;
- chronic disease in the stage of decompensation (diabetes mellitus, etc.).
Patient preparation
When planning this type of surgical treatment, it is important to consider several points.
Assess all joints adjacent to the problem area in order to understand how capable the neighboring segments are of absorbing the increased load complex. It is especially necessary to reliably assess the condition of the talonavicular joint: this central segment of the foot will bear the maximum share of the load. The positive effect of arthrodesis is possible only in the absence of degenerative-dystrophic changes in it.
Prescribe the patient a comprehensive examination confirming the need for this operation in the absence of contraindications.
Main instructions for the patient:
- detailed blood and urine tests, including biochemistry;
- X-ray, MRI or CT scan of the joint in several planes;
- testing for HIV, syphilis, hepatitis;
- fluorography and electrocardiography;
- examination by highly specialized doctors (cardiologist, pulmonologist, etc.);
- consultation with an anesthesiologist.
A week before the proposed operation, the patient must stop using NSAIDs and agents with blood-thinning properties.
If external fixation systems were used, for example, the Ilizarov apparatus, plaster is not used. When installing internal metal implants on the operated limb, plaster immobilization is used in the postoperative period. Until ankylosis occurs, the patient is in a plaster cast. The joint is completely fused and immobilized 3–6 months after surgery. The rate of bone fusion may differ due to the physiological characteristics of the individual patient.
Rehabilitation
Exercise therapy. After arthrodesis of the ankle joint, physical therapy should be carried out from the first day to prevent the development of muscle atrophy, thrombus formation and congestion in the lungs. These are breathing exercises, isometric exercises to maintain and strengthen the muscles of the lower leg and thigh. Gymnastics involves a gradual increase in load.
Drug treatment. It includes highly effective therapy against the formation of infectious pathogenesis; use of symptomatic drugs; use of medications for thromboembolic complications.
From the second day the patient can get up. Walking is allowed only with the support of crutches, avoiding any load on the operated limb. After the first signs of ankylosis appear (after about 6 weeks), it is allowed to partially apply a gentle axial load on the sore leg. The patient will be able to try to walk normally no earlier than after 4–6 months. Removal of metal structures is usually after 10–12 months. Internal fixators do not always need to be removed.
Complications
The incidence of complications after standard surgery with a wide joint opening is higher than after arthroscopic interventions. Here are some comparative data on adverse reactions for 2 types of procedures (without the use of external fixators) found during the first 3 weeks:
- phlebothrombosis is detected in 22% of cases after open ankle arthrodesis, in 1.8% after minimally invasive intervention;
- wound infection develops in approximately 12% of patients, while the risks after arthroscopy are practically absent (<0.1%);
- necrosis of surrounding tissues, respectively, in 17% and 0.2%;
- wound hematomas and seromas: 22% and 0.9%.
Intraoperative blood loss after standard arthrodesis is 150–200 ml, after arthroscopic arthrodesis - about 120 ml. Failure of ankylosis after 6 months is determined in 5-6% of people who underwent the procedure according to the traditional scenario, and in 0.5-0.9% of patients who underwent arthroscopy with intramedullary fixation. After any type of artificial ankylosis, there are increased risks associated with the formation of arthrosis in other joints of the limb and shortening the leg length by up to 3 cm.
REFERENCE
The ankle is the support of the entire skeleton and muscular system. The ankle joint should normally support almost 90% of the total body weight when a person stands or engages in physical activity in an upright position. The joint also provides shock absorption for the limb and various movements of the foot in a normal amplitude. Violation of its performance can lead to deterioration of gait, limiting a person’s movement even to the point of disability.