Osteoarthritis deformans is a chronic degenerative joint disease. It is based on primary degeneration of articular cartilage with subsequent changes in bone articular surfaces and the development of marginal osteophytes, which entails joint deformation. 10-12% of the Russian population suffers from deforming osteoarthritis. For the treatment of deforming osteoarthritis, all conditions have been created at the Yusupov Hospital:
- Chambers with a European level of comfort;
- Equipment from leading global manufacturers;
- Individual approach to the treatment of each patient;
- Use of modern medications and innovative surgical technologies.
At a young age, deforming osteoarthritis (ICD10 code from M15 to M19) more often develops in men who have sustained injuries to the musculoskeletal system. In old age, the disease mainly affects women. With deforming osteoarthritis, the knee and hip joints are primarily affected. The degree of deforming arthrosis increases depending on the severity of joint deformation.
Coxarthrosis [arthrosis of the hip joint]
ICD-10 International Classification of Diseases M00-M99 Diseases of the musculoskeletal system and connective tissue M00-M25 Arthropathy M15-M19 Arthrosis
M16
Coxarthrosis [arthrosis of the hip joint]
— M16.0 Primary coxarthrosis bilateral - M16.1 Other primary coxarthrosis - M16.2 Coxarthrosis as a result of dysplasia bilateral - M16.3 Other dysplastic coxarthrosis - M16.4 Post-traumatic coxarthrosis bilateral - M16.5 Other post-traumatic coxarthrosis - M16.6 Other secondary coxarthrosis bilateral - M16.7 Other not secondary coxarthrosis - M16.9 Coxarthrosis, unspecifiedFull interpretation of the ICD code M16: ICD code M16 / International Classification of Diseases / Diseases of the musculoskeletal system and connective tissue / Arthropathy / Arthrosis / Coxarthrosis [arthrosis of the hip joint]
Search
- M16.0Primary coxarthrosis bilateral
- M16.1 Other primary coxarthrosis
- M16.2 Coxarthrosis as a result of dysplasia, bilateral
- M16.3 Other dysplastic coxarthrosis
- M16.4 Post-traumatic coxarthrosis, bilateral
- M16.5 Other post-traumatic coxarthrosis
- M16.6 Other secondary coxarthrosis, bilateral
- M16.7 Other secondary coxarthrosis
- M16.9 Coxarthrosis, unspecified
Code M16 “Coxarthrosis [arthrosis of the hip joint]” is part of the alphanumeric code system of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10).
The subgroup of codes M16 belongs to the group of codes M15–M19 “Arthrosis”. This group is part of the code block M00–M25 “Arthropathy”. This block is included in Class XIII “Diseases of the musculoskeletal system and connective tissue”.
Mechanism of development of coxarthrosis
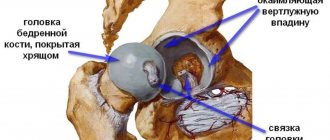
At the initial stage, the consistency of the joint fluid changes - it becomes viscous and thick, which leads to the gradual drying of the hyaline cartilage. Because of this, it gradually collapses and cracks appear on the surface. Due to the thinning and drying of cartilage tissue, pathological deformations begin in the hip joint. Further development of the pathology leads to rubbing and deformation of the bones, as the load on the bone tissue increases. At a severe stage, diagnostics reveals not only the destruction of cartilage and bone tissue, but also muscle atrophy.
Active substances related to code M16
Below is a list of active substances related to ICD-10 code M16 (names of pharmacological groups and a list of trade names associated with this code).
- Active ingredients
- Hyaluronic acid
Pharmacological groups: Correctors of bone and cartilage tissue metabolism, Regenerants and reparants - Glycosaminoglycan-peptide complex
Pharmacological groups: Regenerants and reparants, Correctors of bone and cartilage tissue metabolism - Glucosamine
Pharmacological group: Correctors of bone and cartilage tissue metabolism - Glucosamine + Ibuprofen + Chondroitin sulfate
Pharmacological groups: NSAIDs - Propionic acid derivatives in combination with other drugs, Correctors of bone and cartilage tissue metabolism in combination with other drugs - Glucosamine sulfate
Pharmacological group: Correctors of bone and cartilage tissue metabolism - Diclofenac
Pharmacological groups: Ophthalmic drugs, NSAIDs - Acetic acid derivatives and related compounds - Diclofenac + Lansoprazole
Pharmacological groups: Proton pump inhibitors in combination with other drugs, NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Diclofenac + Paracetamol
Pharmacological groups: Anilides in combination with other drugs, NSAIDs - Acetic acid derivatives and related compounds in combination with other drugs - Lidocaine + Tolperisone
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs - Tolperisone + Lidocaine
Pharmacological group: n-cholinergics (muscle relaxants) in combination with other drugs
Full Russian-language electronic version of the International Classification of Diseases, 10th revision, with changes and additions WHO 1990-2019. (current in 2021)
A temporary code for COVID-19 has been added to section U00-U49
- U07.1
Codes U00-U49 should be used to temporarily assign new diseases of unknown etiology. In emergency situations, codes are not always available in electronic systems. Category U07 specifications allow them to be used in every electronic system at any time on behalf of WHO immediately.
- Osteoarthrosis (polyarthrosis, coxarthrosis, gonarthrosis)
Causes of osteoarthritis of the hip joint
Healthy cartilage has the ability to regenerate, but daily stereotypic loads lead to constant wear and tear of certain areas of the articular surface. This leads to joint deformation, increased load on the ligaments and other pathological consequences. The causes of this condition can be divided into two categories: insufficient regeneration (for example, due to insufficient nutrition or excessive abrasion) and breakdown of cartilage tissue (aging, inflammatory processes). In most cases, both of these processes go hand in hand.
Among the common causes of osteoarthritis of the hip joint, one cannot fail to mention:
- congenital abnormalities of the structure of the joint or cartilage tissue (flat feet, excessive joint mobility, intrauterine hip dislocation);
- advanced age;
- menopause in women and endocrine disorders;
- overweight;
- professional or sports loads;
- hip injuries and other pathologies associated with subchondral bone defects;
- pre-existing arthritis and other inflammatory diseases;
- genetic predisposition, including to joint dysplasia;
- metabolic disorders (for example, diabetes mellitus);
- sedentary lifestyle and insufficient muscle mass;
- belonging to the Asian race;
- diet poor in vitamins C, D and K.
general information
Short description
Osteoarthritis (OA) is a chronic progressive degenerative joint disease characterized by degradation of articular cartilage with subsequent changes in the subchondral bone and the development of marginal osteophytes, leading to loss of cartilage and concomitant damage to other components of the joint (synovium, ligaments). Protocol code: HS-014 “Osteoarthrosis (polyarthrosis, coxarthrosis, gonarthrosis)” Profile: surgical Stage: hospital ICD-10 code(s): M15 Polyarthrosis M16 Coxarthrosis (arthrosis of the hip joint) M17 Gonarthrosis (arthrosis of the knee joint) M19 Other arthrosis
Cloud MIS "MedElement"
Clinic automation: fast and inexpensive!
- 290 clinics from 4 countries connected
- 1st place - 800 rubles / 4500 tenge per month.
- Registration + Cashier - 15,800 rubles / 79,000 tenge per year
Find out more+7 / +7 707 707 07 [email protected]
Cloud MIS "MedElement"
Clinic automation quickly and inexpensively!
290 clinics from 4 countries work with us- Connection of 1 workplace -
800 rub / 4500 tenge per month - Learn more about the system
+7 / +7 707 707 07 16 /
Treatment at the Energy of Health clinic
Only a doctor can decide how to treat coxarthrosis. The specialists of the Energy of Health clinic regularly improve their qualifications and hone their skills. This gives us the opportunity to quickly make the correct diagnosis and begin treatment.
We offer you modern drug treatment regimens for arthrosis of the hip joint, including intra-articular injections and punctures with the introduction of a synovial fluid analogue. If there are contraindications, the physiotherapist will select the optimal course of procedures. At your service:
- massage;
- physical therapy under the supervision of an instructor;
- manual therapy;
- electrophoresis;
- ultrasound treatment and other techniques.
Classification
Classification by Nasonov V.A., Astapenko M.G., 1989. — primary (idiopathic); - secondary. - polyarthrosis; - oligoarthrosis; - monoarthrosis; - in combination with osteoarthritis of the spine, spondyloarthrosis. — interphalangeal joints (Heberden’s nodes, Bouchard’s nodes); - hip joints (coxarthrosis); — knee joints (gonarthrosis); - other joints. Synovitis: - present; - absent. — functional ability is limited (FN-1); — ability to work is lost (FN-2); - needs outside care (FN-3) (FN - functional failure).
Non-drug methods for treating coxarthrosis
An effective method of treating coxarthrosis is manual therapy. Doctors most often use two types of effects on the joint: mobilization and manipulation. Mobilization is a gentle traction of the hip joint, spreading the ends of the bones that articulate with each other. Manipulation is carried out in one sharp and short movement. If the manipulation is carried out in a timely manner and in the right place, it immediately brings relief to the patient, reducing pain and restoring range of motion in the hip joint. This happens during the initial manifestations of the disease.
Rehabilitation specialists at the Yusupov Hospital use hardware traction (traction of the hip joint) in the treatment of coxarthrosis to separate the articular ends of bones and reduce the load on the cartilaginous surfaces. A course of traction therapy consists of 10-12 procedures, which are carried out daily or every other day in combination with massage and other therapeutic measures. A patient with coxarthrosis is recommended to undergo 2 such courses of treatment per year.
Postisometric relaxation (stretching muscles and ligaments) is a relatively new treatment method that involves active interaction between the patient and the doctor. During the procedure, the patient tenses and relaxes certain muscles, and the doctor, while relaxing the patient, “stretches” the muscles, tendons and joints. In the treatment of coxarthrosis, post-isometric relaxation is used to eliminate painful spasmodic muscle contractions and as a procedure preceding a session of manual therapy or joint traction. Postisometric relaxation is one of the most useful procedures in the treatment of coxarthrosis of stages I and II. The method has almost no contraindications.
Rehabilitation specialists at the Yusupov Hospital use therapeutic massage as an additional method of therapy for coxarthrosis of stages I and II. Massage has the following effects on the hip joint:
- Improves blood circulation;
- Accelerates the delivery of nutrients to cartilage;
- Increases the elasticity of the joint capsule and ligaments;
- Restores the function of the synovial membrane.
Rehabilitation specialists at the Yusupov Hospital use massage for coxarthrosis in combination with post-isometric relaxation, manual therapy or traction of the hip joint.
Diagnostics
Diagnostic criteria Complaints and anamnesis: 1. Pain during physical activity and/or at rest, at night, when palpating the joint. 2. Stiffness in the affected joint in the morning or occurring after any rest, not exceeding 30 minutes. 3. Limitation of joint mobility or a feeling of instability in it. Physical examination: painful points in the places where the tendons attach to the joint capsules, crepitus and cracking in the joint when moving. Clinical features of individual forms of OA OA of the hip joint (coxarthrosis) is one of the most common variants of the disease. OA develops with equal frequency in men and women, but in women it is much more severe. It is noted that if coxarthrosis develops before the age of 40, it is usually associated with joint dysplasia (congenital acetabular dysplasia). The main symptoms of OA are mechanical pain in the joint area; gait disturbance (limping) occurs early on. In some cases, pain initially appears in the knee joint, groin, buttock, thigh, and lower back. The pain syndrome appears when walking and subsides with rest. The first clinical symptoms (pain, limited range of motion) appear in the absence of radiological changes in the joint; they are caused by muscle spasm. With bilateral damage, patients with coxarthrosis develop a “duck gait.” OA of the knee joint (gonarthrosis). The knee joint is the second most common location of deforming OA. Gonarthrosis usually affects women, which is facilitated by obesity and poor circulation in the lower extremities. The first symptoms usually appear between 40 and 50 years of age. The most common etiological factors in the development of the disease are poor posture and frequent trauma. As a rule, gonarthrosis is bilateral, but the patient complains of pain in one joint for a long time. With long-term gonarthrosis, a “blockade” of the joint may periodically occur, associated with the appearance of a “joint mouse” in the articular cavity. Damage to the knee joint can be complicated by osteonecrosis of the femoral condyle, this is observed with varus deviation. Instrumental studies: X-ray picture of joint damage, confirming the diagnosis - narrowing of the joint space until it disappears, bone growths along the edges of the articular surfaces, grossly deformed articular ends. List of main diagnostic measures: 1. X-ray examination of the joint. 2. Computed tomography of joints. 3. Nuclear magnetic resonance of joints. 4. Ultrasound of internal organs.
Online consultation with a doctor
Consult an experienced specialist without leaving your home!
Health consultation from 2500 tenge / 430 rubles
Interpretation of analysis and research results
Second opinion regarding diagnosis, treatment
Choose a doctor
Symptoms
The main symptoms of coxarthrosis of the hip joint do not depend on the cause of development. Most patients note:
- limitation of movement: one of the earliest symptoms caused by thinning of the cartilage layer and increased friction of the articular surfaces of the bones; in the future, the appearance of cartilaginous growths further aggravates the problem;
- pain: friction of bones devoid of cartilage against each other, gradual involvement of all elements of the joint in the degenerative process, decreased blood supply to tissues cause pain that increases as the disease progresses; the pain is shooting in nature and often intensifies towards the end of the day;
- muscle spasm, which leads to increased pain and limited range of motion in the joint;
- decrease in leg length: this symptom appears in the later stages of the disease due to the narrowing of the joint space and the gradual grinding of the heads of the bones due to constant friction; the difference between the legs can reach 2 cm;
- lameness: associated with severe pain and limitation of movement, as well as shortening of the leg; is an unfavorable sign indicating serious damage to the articular apparatus.
Treatment
Treatment tactics Treatment goals: reduction of functional joint insufficiency, correction of therapy. Non-drug treatment Algorithm for the treatment of osteoarthritis. Stage I: - physiotherapy (thermal procedures, hydrotherapy); — physical therapy (the main task is to reduce the load on the joint and strengthen the muscles): correction of posture and length of the lower extremities, exercises with isometric loads, exercises for individual muscle groups; - local analgesics and NSAIDs (ointment, gel, cream). Drug treatment Algorithm for the treatment of osteoarthritis. Stage II: - systemic NSAIDs (non-steroidal anti-inflammatory drugs) when signs of manifest osteoarthritis occur and when signs of inflammation appear; - oral and rectal NSAIDs - ibuprofen, diclofenac, ketoprofen, lornoxicam, priroxicam, celecoxib; - chondroprotectors; - for persistent synovitis - intra-articular administration of glucocorticoids. Stage III: - if conservative treatment is ineffective - orthopedic surgery: hip or knee replacement, arthroscopy with abrasive chondroplasty. 1. Local analgesics (drugs with irritating and distracting effects) - finalgon. 2. Local NSAIDs - diclofenac, ibuprofen, ketoprofen, piroxicam. 3. Systemic NSAIDs - diclofenac (100–150 mg/day), ibuprofen (1200–2400 mg/day), ketoprofen (200–300 mg/day), naproxen (500–100 mg/day), piroxicam (20 mg/day), lornoxicam (8–16 mg/day). 4. Specific COX-2 inhibitors: celecoxib (200–400 mg/day). 1. Chondroitin sulfate (500 mg 2 times a day). 2. Hyaluronic acid derivatives for intra-articular administration (3 weekly intra-articular injections). Preventive measures: prevention of joint injuries, timely, complete treatment of arthritis. Further management: - elimination of mechanical factors (wearing orthopedic shoes, a corset or support belt, using a cane); - weight loss; - unloading of the affected joint. List of essential medications: 1. *Ibuprofen 200 mg, 400 mg tablet. 2. *Diclofenac sodium 25 mg, 100 mg, 150 mg tablet. 3. Diclofenac sodium, emulgel 1% for external use 4. Diclofenac potassium 12.5 mg tablet. 5. Ketoprofen solution for injection 100 mg/2 ml, amp. 6. Lornoxicam 4 mg, 8 mg tablet. 7. Celecoxib 100 mg, 200 mg caps. 8. Naproxen 250 mg tablet. 9. Piroxicam 10 mg tablet. 10. Chondroitin sulfate 5%, ointment 11. Phosphaden 0.05 g tablet, 2% solution for injection, amp. 12. Pentoxifylline 100 mg, dragee, solution for injection 100 mg/5 ml amp. 13. *Nadroparin calcium - solution for injection in pre-filled syringes 2850 IU anti-Xa/0.3 ml; 3800 IU anti-Xa/0.4 ml; 5700 IU anti-Xa/0.6 ml; 7600 IU anti-Xa/0.8 ml, 9500 IU anti-Xa/1.0 ml Indicators of treatment effectiveness: reduction in functional joint failure.
* – drugs included in the list of essential (vital) medicines.
Hospitalization
Indications for hospitalization: severe pain, lack of effect of outpatient therapy, synovitis of the joint. The required scope of examinations before planned hospitalization: 1. X-ray of the affected segment and symmetrical joint in 2 projections. 2. General blood test (6 parameters). 3. General urine analysis. 4. Determination of C-reactive protein. 5. Reaction of Wright and Heddelson during joint production. 6. ECG. 7. Examination of stool for worm eggs. 8. Microreaction.
Information
Sources and literature
- Protocols for the diagnosis and treatment of diseases of the Ministry of Health of the Republic of Kazakhstan (Order No. 764 of December 28, 2007) 1. Nasonova V.A., Osteoarthrosis. 2001; 2. Drozdov V.N., Osteoarthrosis, 2004; 3. Nasonova V.A., Muravyov Yu.V., Tsvetkova E.S., Belenkiy A.G., Osteoarthritis of the knee joint, 2003; 4. Nasonova V.A., Nasonov E.L., Alekseeva L.I., Muravyov Yu.V., Osteoarthrosis of the hip joint, 2004; 5. Nasonova V.A., Modern view of the problem of osteoarthritis, 2004; 6. Povoroznyuk V.V., Osteoarthrosis: modern principles of treatment, 2003.
Information
Stages and features of their manifestation
The classification of hip pathology includes four degrees of severity.
- Osteoarthritis of the first stage. In rare cases, it is diagnosed only on x-rays; pain at this stage is rare. The patient attributes them to fatigue.
- Second stage. Pain when moving begins to cause enough concern to see a doctor. The image shows a decrease in the interosseous space and significant growths on the head of the joint. These injuries cause constant pain, which radiates further into the legs and groin. A radiologist can diagnose DOA by identifying abnormal growths on the bone.
- Stage three deforming osteoarthritis of the hip joints can cause disability. Pronounced symptoms allow the doctor to make a diagnosis without an in-depth examination. X-ray images reveal the absence of a layer between the joints and large cyst-like formations are visible. When moving, the bones crunch and the affected area is deformed.
- At the fourth stage, the disease completely impairs mobility. Complete deformation of the joint. The patient becomes disabled.
Attached files
| 1. (HS-014-Osteoarthrosis__polyarthrosis,_coxarthrosis,_gonarthrosis.pdf) | read/download file |
Mobile application "MedElement"
- Professional medical reference books. Standards of treatment
- Communication with patients: online consultation, reviews, making an appointment
Download the application for ANDROID / for iOS
Mobile application "MedElement"
- Professional medical reference books
- Communication with patients: online consultation, reviews, making an appointment
Download the application for ANDROID / for iOS
Attention!
If you are not a medical professional:
- By self-medicating, you can cause irreparable harm to your health.
- The information posted on the MedElement website and in the mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Guide” cannot and should not replace a face-to-face consultation with a doctor. Be sure to contact a medical facility if you have any illnesses or symptoms that concern you.
- The choice of medications and their dosage must be discussed with a specialist. Only a doctor can prescribe the right medicine and its dosage, taking into account the disease and condition of the patient’s body.
- The MedElement website and mobile applications “MedElement”, “Lekar Pro”, “Dariger Pro”, “Diseases: Therapist’s Directory” are exclusively information and reference resources. The information posted on this site should not be used to unauthorizedly change doctor's orders.
- The editors of MedElement are not responsible for any personal injury or property damage resulting from the use of this site.
Hello, dear friends! Today we will understand the question of what code is coxarthrosis of the hip joint according to ICD 10, what class of diseases it belongs to.
Many people know that there is such a system as ICD 10, but not everyone knows why it is needed and what benefits the doctor and patient can get from it. This will be discussed further.
Prognosis and prevention
Osteoarthritis is a degenerative disease associated with stress, injury, and neglect of the body. It is difficult to diagnose in the early stages. Throughout your life, you need to use the maximum of available means and methods to extend the life of your joints.
Firstly, it is minimizing provoking factors. Deliberate exercise to avoid microtrauma. Caring for the musculoskeletal system during everyday activities.
Secondly, proper nutrition and maintaining your own weight within the normal range. Consumption of healthy foods, fruits, vegetables, foods rich in beneficial microelements will give the body the resources it needs to regenerate.
Thirdly, the development of your own body. Gymnastic exercises give flexibility and increase the resource of joints. A developed muscular frame takes on part of the load, allowing the bones to remain functional longer. Daily exercise keeps the body in good shape. The lungs work at full capacity, enriching every cell with oxygen. Even daily walking has a beneficial effect on joints.
When the body gives signals about violations, you should not ignore them.
By putting off a medical examination and consultation with a doctor, you can wait for serious complications. The article has been verified by the editors
What is ICD?
ICD - 10 or the International Classification of Diseases, Tenth Revision, is a document accepted throughout the global medical community.
It characterizes the level of development of healthcare, which determines the comparability of diseases and medical norms of pathological processes.
This classification quickly allows you to identify the disease by group, class, type, type, nature of the course, allows you to describe the pathological process or condition so that it is clear to all doctors in the world, and accordingly it would be possible to consult with colleagues from different countries about the choice of treatment method .
The World Health Organization makes changes to the ICD every 10 years and approves the new edition.
At the moment, ICD 10, that is, the tenth edition, is relevant. With the help of ICD 10, you can very conveniently systematize and save data on all currently known pathologies, which allows you to quickly resolve the issue of treatment with doctors from all over the world.
Also, this classification allows us to combine all methodological approaches to the preparation and selection of treatment tactics.
Therefore, ICD 10 today can be called the main document of the modern healthcare system.
Deforming osteoarthritis of the hip joint
Normally, the heads of the bones are covered with a layer of spongy tissue, which is capable of absorbing moisture in a calm state, and then, under load, releasing it, forming a lubricant. Joint lubrication ensures sliding inside the moving joint, and the cartilage itself additionally acts as a shock absorber. This joint function allows us to walk, run and jump without injury with every movement.
In osteoarthritis of the hip joint, the articular cartilage is primarily affected, the destruction of which causes changes in the synovial articular membrane, degenerative processes in the bone and ligament degeneration. Most often, this pathology occurs in a situation where the mechanical load on the cartilage exceeds its “endurance.” In this case, the lining of the joint seems to wear away, exposing the bones and causing them to rub against each other. Depletion of cartilage tissue leads to a narrowing of the lumen in the joint space, a decrease in the range of motion, and even the appearance of microcracks in the pelvic and femur bones. Therefore, among the complications of the disease, a femoral neck fracture is often encountered - a serious injury that requires long and expensive rehabilitation, and at the age of 60 can even pose a threat to life.
The loss of elasticity of cartilage and lack of gliding in the joint contributes to the formation of osteophytes - spike-shaped bone growths that appear at the site of microcracks. Although osteophytes are designed to compensate for the loss of cartilage tissue and increase the articular surface area, their appearance causes discomfort. They not only make movement difficult and lead to chronic inflammation of the tissues around the joint, but they can also break off with sudden movements, causing severe pain. Nodules can also form in the periarticular tissue.
The deformity can occur on one side, leading to noticeable shortening of the limb and lameness, or on both sides at the same time. The first condition is more typical for post-traumatic disorders, and the second for complex, for example, metabolic diseases that provoke degeneration of cartilage tissue.
Sometimes the disease even affects young people, especially men. In adulthood, it is 2 times more common in women whose bones rapidly lose calcium during menopause.
What place does coxarthrosis of the hip joint occupy in the international classification of diseases?
Deforming coxarthrosis of the hip joint is designated in the international classification of diseases. In order to understand why it is in a certain place in ICD 10, it is necessary to understand what kind of pathology it is. Coxarthrosis refers to pathologies of a dystrophic and degenerative nature that affect the largest joint of the human body.
The top of the head of the bone is covered with cartilage. As the joint moves, the cartilage contracts and releases joint fluid, which serves as a lubricant for the moving bones.
With rest, the cartilage straightens. In addition to lubrication, it also serves as a shock absorber during movement. As a result of coxarthrosis, the synovial fluid becomes thick and can no longer lubricate the entire surface of the cartilage.
It dries out and cracks. The bones begin to rub against each other and are destroyed. Primary coxarthrosis, both left- and right-sided, usually has an unknown etiology, and secondary coxarthrosis becomes a consequence of tumors, injuries, inflammation of the hip joint, necrosis of the femoral head, congenital dysplasia of the hip joints. The process The development of the pathology is irreversible, however, with timely detection of the disease, it is quite possible to delay its final stage and prevent complete destruction of the joint.
Accordingly, the lack of treatment quite quickly leads to a transition from one stage to another, causing disability, restriction of joint mobility, up to its complete immobility. The development of the disease is promoted by:
- hormonal imbalances in the body;
- violation of metabolic processes;
- physical inactivity;
- hip dysplasia;
- overweight;
- congenital malformations of bones and joints;
- infectious diseases, autoimmune processes.
Coxarthrosis is most often diagnosed in older people, especially women, but recently the trend is that the disease is gradually getting younger; its detection at 20-30 years of age does not come as much of a surprise to doctors.
If the initial (stages 1 and 2) of coxarthrosis can be dealt with with the help of exercise therapy, medications, physiotherapy, and folk remedies, then at stages 3–4 of the development of the pathology, partial or complete replacement of the hip joint is often required.
Drug treatment of coxarthrosis
With the help of drug therapy, rheumatologists at the Yusupov Hospital solve the following problems:
- Eliminate pain;
- Improves nutrition of articular cartilage and accelerates its recovery;
- Activate blood circulation in the area of the affected hip joint.
The goal of conservative treatment is to reduce pressure on the damaged articular head of the femur and increase the distance between it and the acetabulum, strengthen the muscles surrounding the diseased joint, and increase the mobility of the hip joint.
Rheumatologists at the Yusupov Hospital prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) to patients with coxarthrosis to relieve pain and inflammation. This group of drugs includes the following drugs:
- Diclofenac;
- Ketoprofen;
- Indomethacin;
- Butadion;
- Movalis;
- Nimulid.
NSAIDs are good at reducing inflammation in the joint and eliminating pain, but they do not treat coxarthrosis itself. Scientists have proven that non-steroidal anti-inflammatory drugs, when used for a long time, can aggravate the process of destruction of cartilage tissue. There are contraindications for their use, since the drugs have side effects.
Chondroprotectors - glucosamine and chondroitin sulfate - improve the structure of the tissue and stop the destruction of the hip joint in coxarthrosis. These are substances that nourish cartilage tissue and restore the structure of damaged cartilage of the hip joint due to coxarthrosis. Unlike non-steroidal anti-inflammatory drugs, chondroprotectors do not so much eliminate the symptoms of the disease as act on the “base” of the disease.
Their use helps restore the cartilaginous surfaces of the hip joint, improve the synthesis of joint fluid and normalize its properties. Chondroprotectors are indispensable in the treatment of the initial stage of coxarthrosis, but are little effective in the third stage of the disease, when the cartilage is almost completely destroyed. To achieve the maximum therapeutic effect, rheumatologists at the Yusupov Hospital prescribe chondroprotectors in courses over a long period of time.
Rheumatologists prescribe muscle relaxants (mydocalm, sirdalud) to eliminate painful muscle spasms that often accompany coxarthrosis. These drugs eliminate muscle pain and somewhat improve blood circulation in the area of the affected hip joint. Their use requires some caution. Often, muscle spasm is a protective reaction of the body, which protects the hip joints from further destruction. If you relieve the protective muscle tension with the help of muscle relaxants, but do not take measures to save the joint from excessive pressure, the hip joint subsequently begins to deteriorate at an accelerated pace. Rheumatologists at the Yusupov Hospital use muscle relaxants in combination with chondroprotectors and joint traction. They are not used as an independent method of treatment.
The use of medicinal ointments and creams does not cure coxarthrosis. Their use sometimes significantly improves the patient's condition. For coxarthrosis, ointments that warm or irritate the skin are successfully used:
- Menovazin;
- Espol;
- Gevkamen;
- Nicoflex cream;
- Finalgon.
The irritation of skin receptors that occurs when they are rubbed stimulates the production of endorphins - our internal painkillers, which reduce pain and partially eliminate painful spasms of the periarticular muscles. Warming ointments increase blood circulation in the tissues and muscles around the affected hip joint.
Intra-articular injections of drugs for coxarthrosis are used quite rarely, since even a healthy hip joint has a narrow joint space and a small articular cavity. When, due to coxarthrosis, the gap of the hip joint narrows, it is quite problematic to introduce the medicine directly into its cavity. There is a risk of damaging the vascular and nerve trunks located along the intended needle insertion. Therefore, doctors prefer to inject drugs not into the hip joint, but into the periarticular area. Pain syndrome is eliminated with the help of periarticular injections of Kenalog, Diprospan, Flosterone, and Hydrocortisone.
Chondroprotectors (alflutop, chondrolone or homeopathic Target T) are injected into the periarticular tissues. They are used in courses over two or three years. During one course of treatment, from 5 to 15 periarticular injections of chondroprotectors are performed. These medications act on the cause of the disease, improve the condition of cartilage tissue and normalize metabolism in the hip joint. Sometimes doctors use intra-articular injections of hyaluronic acid (an artificial joint lubricant) to treat coxarthrosis. For this purpose, the drugs Ostenil, Synvisc, Fermatron, Duralan and the new domestic drug Giastat are used. Hyaluronic acid preparations are injected through the groin, directly into the hip joint itself. They are really useful, but there is a circumstance that significantly limits their use in coxarthrosis: it is quite difficult to administer the medicine exactly into the cavity of the hip joint affected by the pathological process. For this reason, rheumatologists at the Yusupov Hospital administer hyaluronic acid preparations under direct control using an X-ray machine or tomograph.
ICD code for coxarthrosis
According to ICD 10, right- and left-sided coxarthrosis refers to pathologies of the osteoarticular apparatus, connective tissue and muscle structures, which are located in 13th place and include 22 classes of diseases.
Among them you can find 9 types of coxarthrosis. So, in order. Coxarthrosis is in class 13, block “arthrosis M15-M19”. It includes:
- M15 – polyarthrosis;
- M16 – coxarthrosis of the hip joint;
- M 17 – gonarthrosis (arthrosis of the knee joint);
- M18 – arthrosis of the first carpometacarpal joint;
- M19 – other arthrosis.
As we can see, coxarthrosis is numbered M 16.
Moreover, it also has its own classification depending on the etiology of the disease:
- M 16.0 – bilateral coxarthrosis, formed as a primary process.
- M 16.1 – other primary coxarthrosis.
- M 16.2 – bilateral dysplastic coxarthrosis.
- M 16.3 – other dysplastic coxarthrosis.
- M 16.4 – uncomplicated bilateral post-traumatic coxarthrosis.
- M 16.5 – other post-traumatic coxarthrosis.
- M 16.6 – secondary bilateral coxarthrosis of a different origin.
- M 16.7 – pathological processes of secondary etiology.
- M 16.8 – unspecified forms of coxarthrosis.
Physiotherapeutic treatment of coxarthrosis, diet and exercise therapy
Most physiotherapeutic procedures are unsuitable for the treatment of coxarthrosis. The hip joint lies deep, it is hidden under the thickness of the muscles, and physiotherapeutic procedures cannot radically affect the course of the disease. Physiotherapy can only bring some relief to the patient due to improved blood circulation and reflex analgesic effects.
With coxarthrosis, diseased joints lose moisture and become “dry”. Patients are advised to drink more water. To reduce the risk of edema in elderly patients, the liquid should be consumed in fractions. They are also prescribed treatment for the underlying disease that may be causing the swelling. If the patient is not prone to edema, he can drink up to two liters of non-carbonated purified water per day.
An important method of treating coxarthrosis is therapeutic exercises. Rehabilitation specialists at the Yusupov Hospital individually select for each patient those exercises that strengthen the muscles of the affected limb and the ligaments of the diseased joint, but do not force him to bend and unbend too much.
Instead of the usual fast dynamic exercises (active flexion-extension of the lower extremities), you need to do static exercises. You can lie on your stomach and slightly raise your leg, straightened at the knee, and keep it suspended. After 1-2 minutes, the patient will feel fatigue in the leg muscles, although the joints did not work in this case.
Also, the exercise therapy instructor suggests that patients very slowly raise their straightened leg to a height of 15-20 centimeters from the floor and slowly lower it. After 8-10 such slow exercises, the patient will feel tired. In case of coxarthrosis, loads on the hip joint and performing fast, energetic exercises with maximum amplitude are contraindicated. You should not swing your legs or actively squat, so as not to subject the hip joints to increased stress and to accelerate their destruction. When the first signs of coxarthrosis appear, make an appointment by phone with a rheumatologist at the Yusupov Hospital.