Last Updated on 06/23/2017 by Perelomanet
The paired flat part of the skull, the parietal bone, resembles a rectangle, curved on the inside, but looks convex and smooth on the outside. Located in the upper and lateral parts of the skull.
The most prominent part is the parietal tubercle. From the inside, this bone contains parts of the cerebral convolutions and arterial grooves that nourish the lining of the brain. The crown is a bony structure that is divided into four distinct edges:
- anterior - this edge is connected to the upper structure of the forehead;
- occipital – combined with the bone of the occipital part;
- lateral – combined with the temple bone;
- medial - an edge that is connected in the central region of the skull by a sagittal suture with the opposite parietal bone.
A fracture of one of the parts of the parietal bone is considered a very serious injury, since it can subsequently worsen the functioning of brain activity.
Types of parietal bone fractures
There are three main types of bone injuries:
- A linear fracture is a crack or separation in the area where the skull connects to the bones. In this case, the bone plate is not displaced. This type of injury is often diagnosed in children;
- comminuted damage - complete destruction of any area of the bone. Damage of this type is considered the most dangerous;
- Depressed fracture - with such an injury, the bone is pressed into the skull. The fracture can be either open or closed; sometimes this damage occurs with trauma to the aponeurosis.
A comminuted and depressed fracture poses a serious danger to the patient’s life, both to the brain and to its membranes. Trauma leads to deviations in the formation of normal life processes.
Such fractures in children often affect subsequent mental and physiological development. At a young age, due to the fact that the brain tissue is not fully matured, and during an injury it can be damaged, difficulties arise. The child may subsequently develop problems with psychological and physical health, with the development of the intracranial structure, and also often encounter difficulties on an emotional level.
Diagnosis of depressed skull fractures
Before developing treatment tactics, CELT specialists conduct a comprehensive diagnosis of the injury. It allows you to accurately determine its location, size and consequences to which it led. The optimal method is still radiography - projection craniography. It provides an overview of the damage from all sides and allows you to understand exactly how the fracture occurred, which is important when preparing for treatment.
In addition to radiography, computed tomography or magnetic resonance imaging is used to diagnose depressed skull fractures using the bone mode. It allows you to determine the condition of the subosseous space. Along with instrumental techniques, a neurological examination is carried out aimed at checking reflexes, assessing sensitivity and muscle strength.
Causes
The parietal bone of the skull is fractured as a result of:
- direct or indirect blow to the cranial area;
- falling from a hill;
- increased impact with a blunt object;
- gunshot wound;
- traffic accident;
- birth procedure;
- increased pressure on the skull.
Most often, a fracture of the parietal bone in a child occurs during play. Children are famous for their restlessness and therefore are often exposed to various injuries. During intense play, a child may fall on his own or, due to his carelessness, push something onto his head, which will ultimately cause an injury.
The discovery of an open fracture is characterized by a rupture of internal soft tissues, traumatic detachment of the surface layer of skin (scalped wound). In this case, there is a possibility of hematoma formation due to internal subcutaneous bleeding. The consequences of an open wound can be infections and bacteria that cause inflammation, and large blood loss, depending on the area of damage.
What causes depressed skull fractures?
A skull fracture is a traumatic disruption of the integrity of the skull, which poses a serious danger to human life. They account for about ten percent of all fractures and about a third of the total number of severe traumatic brain injuries. Most often they are diagnosed in young people leading an active lifestyle or in representatives of socially disadvantaged categories of citizens.
Depressed fractures occur when a person collides with an object whose area is smaller than the area of the skull. This can happen if a person falls or his head quickly approaches such an object. At the same time, experts identify a number of conditions that have a serious impact on the consequences of injury. These include the following:
- Head acceleration direction;
- The shape and material of production of the object that injured the skull;
- The presence of objects that soften the blow of a fracture;
- The difference in contacting areas upon impact;
- The hardness of the bone at the fracture site.
Symptoms
Fractures of the parietal bone of the skull are determined by the following characteristics:
- Strong headache;
- possible loss of consciousness;
- development of hematomas;
- the formation of wounds and abrasions in the injured area.
With more serious injuries of this type, the above symptoms are also accompanied by hemorrhage from the eyes, ears and nose. Blood can be seen flowing down the wall of the larynx. Such signs arise due to the fact that the dura mater of the brain is damaged at the junction of the bones. Bruising can also form in the eyeball.
Symptoms of cephalohematoma
Symptoms of cephalohematoma are especially pronounced 2-3 days after the birth of the child. The shape of the head becomes asymmetrical due to the formation of an elastic and soft formation. The outlines of the swelling coincide with the boundaries of the flat bones of the skull, since the periosteum is firmly attached to their edges. Typical localization of cephalohematoma is the parietal and occipital regions of the head. The skin over the formation is unchanged, elastic, and fluctuation is detected on palpation (fluid movement when pressed). A distinctive feature of kepholohematoma is a gradual increase in formation during the first 2-3 days of the baby’s life. The amount of blood under the periosteum can range from 5 to 150 ml. Under favorable conditions and with a small size, the cephalohematoma regresses on its own within a week after its formation.
With an isolated cephalohematoma, the general condition of the child is satisfactory. In the case of combined pathology, neurological symptoms appear. Most children experience depression of the central nervous system: a sluggish reaction to pathogens, a decrease in the severity of reflexes. Some newborns experience excessive excitation of the central nervous system, such as a hypertensive or hydrocephalic symptom complex.
Violation of the independent regression of cephalohematoma (with a large size of the formation, a blood clotting disorder in an infant) can cause various complications: anemia, resorption hyperbilirubinemia, ossification and infection of the hematoma.
With large cephalohematomas, rapid hemolysis of red blood cells occurs, which is accompanied by a yellowish tint of the skin and visible mucous membranes from the first days of life. This jaundice persists for 10 days or more, in contrast to physiological neonatal jaundice.
First aid
If a child falls or receives a blow to the head, but quickly calms down, this is a serious reason to seek medical help in a special institution in order to make sure that everything is okay. This will help eliminate unpleasant consequences if a fracture is still present. Call an ambulance or take him to the hospital yourself, the victim’s body must be in a horizontal position.
The faster treatment is provided, the fewer complications there will be and the faster the recovery period will pass. If help is not provided immediately, the child may fall into a coma.
Diagnosis of injury
First of all, after arriving at the hospital, the doctor conducts a thorough examination of the patient and asks what caused the injury and what the first symptoms were. This diagnostic method will help in the subsequent medical verdict of a specialist.
Next, the doctor directs the patient to an x-ray procedure, which is performed in two projections. If the injury is serious, then during diagnosis the body does not change its position, but only the X-ray machine tube moves.
Often, such damage is diagnosed using MRI and CT. These devices are the most informative and less dangerous than x-rays. But research with their help is also more difficult to carry out; the patient must be completely immobilized during the procedures, otherwise the results may be incorrect, and in the case of children this is not an easy task.
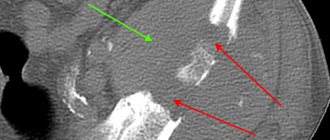
Tomography. Double fracture.
If an isolated linear injury is diagnosed, a lumbar puncture procedure is performed. This will help determine the presence of subarachnoid bleeding in the brain.
After a full examination and study of the results, the attending physician makes his verdict and prescribes the most appropriate method of treatment.
Treatment tactics
After diagnostic procedures, the doctor selects treatment methods that will be most effective in this case. If a mild fracture occurs, uncomplicated by cracks or injuries without displacement of bone fragments, then a conservative method of treatment is chosen. It is to ensure complete peace for the child. Every three hours, a cold special compress is applied to the injured area for an hour.
In case of severe pain, the patient is prescribed non-narcotic painkillers. In case of brain infection, the doctor prescribes antibiotics.
Treatment in a medical facility is prescribed if the patient periodically loses consciousness. In cases where serious signs have not been identified, the child is treated at home.
Surgery is indicated in more severe cases of injury, for example, if the fracture is splintered, a bruise is pressing on the brain or swelling forms in it, and also if there is a displacement of the bones, for example, to the left or down. In such cases, a craniotomy procedure is performed, which allows the removal of an unfavorable hematoma and fragments of crushed bone.
Full recovery from such an injury occurs after three or four months, and already in the third week, fibrous tissue fills the resulting damage and cracks.
Treatment
Once the fracture is confirmed, the specialist will prescribe treatment based on the extent of the damage.
- If there are no hematomas or damage to bone tissue, the child is prescribed painkillers and sent home.
- In case of a crack and mild brain damage, a supine regime and cool compresses every 3 hours for 60 minutes are prescribed.
- If an infection gets inside the brain, antibiotics are used.
- If there is a hematoma that puts pressure on the brain or splinter fractures, surgery will be prescribed. During the operation, craniotomy occurs and the hematoma is removed along with bone fragments.
The main goal of therapy is to reduce the risk of consequences. The resulting brain damage largely depends on how first aid was provided and after what time. Also, therapeutic actions are aimed at eliminating hypoxia and hypotension. To prevent aspiration of the respiratory tract, the arriving team of doctors should perform tracheal intubation to reduce the risk of death.
Consequences
If treatment for a parietal bone injury in a child is untimely or incorrect, the following complications may develop:
- epilepsy;
- violation of psychological health;
- development of meningitis;
- hydrocephalus;
- strabismus or impaired motor functions of the eyes;
- the occurrence of a brain abscess;
- nystagmus;
- impaired reflexes;
- problems with psychological or physical development.
In order to avoid such consequences, if you suspect this type of injury, you must seek help from qualified specialists.