Who is to blame for the lack of progress?
The incomplete functional restoration of the lower limb is groundlessly blamed on the surgeon who performed the operation incorrectly. Patients complain that their knee does not straighten like a healthy leg. Incomplete extension of the knee joint is a fairly common complaint among people.
Contracture of the knee joint - the leg cannot fully straighten.
There are also cases when, even with a well-planned and implemented system of restorative therapy, the recovery process is delayed or complicated by negative pathogenesis. As you understand, here we are most often talking about the individual factor.
Do not neglect the services of rehabilitation specialists when rehabilitating the operated limb. And do not violate the rehabilitation terms: as long as you were told to adhere to a special regime of physical activity, you are obliged to comply with it. Your future quality of life will depend on all this.
Surgical wounds after knee arthroscopy.
Rehabilitation at home and boarding house
After hip and leg replacement, the recovery period is best spent in a specialized center or private boarding house. Patients will be closely monitored by medical personnel.
All types of movements and increased physical activity are performed according to the recommendations of doctors. Treatments are carried out by qualified specialists, after consultation with a surgeon and kinesiotherapist. In medical centers and boarding houses for the elderly, unlike at home, there are special devices, apparatus, and simulators for improving motor skills. Mobility aids are provided: walkers, crutches, canes.
The advantage is that the services are provided in one place. At home, you will either have to invite massage therapists and physical education instructors to your home, paying for their services, or go to the clinic every day.
As a rule, one of the family members remains at home with the ward. It is difficult for him to combine different functions and provide versatile support. The boarding house uses an interdisciplinary approach, healing techniques are varied in a timely manner based on the results of weekly observations.
Postoperative problems and solutions
In the postoperative period, due to injury during the operation of periarticular and intraarticular structures, fluid accumulates in the knee and pain is felt. These are normal phenomena and are not considered complications if the accumulation of effusion, accompanied by swelling of the tissues around the patella, as well as the manifestation of painful signs, do not last longer than expected. These symptoms should subside after 3 days, and by the second week they usually disappear. In the early period, to eliminate swelling and pain, doctors perform drainage and antiseptic treatment of the wound. Additionally assigned:
- immobilization of the limb with orthopedic means;
- placing the leg in an elevated position when the patient is lying in bed;
- applying cold dry compresses;
- anti-inflammatory drugs;
- antibacterial drugs;
- painkillers.
Arthromot is a means for passive development of the knee joint.
Swelling that does not subside for a long time indicates the progression of inflammation, and, possibly, the emergence of a local infectious pathogenesis, which is fraught not only with a lack of effect in restoring mobility, but also with much more complex consequences. For example, if you have had an endoprosthesis installed, the infection leads to rejection and damage to the prosthetic structure, which requires repeated surgery (removal of the implant) and long-term antibiotic therapy. If severe swelling is associated with an excessive accumulation of synovial fluid and blood, you will need to perform a puncture of the joint to remove the pathological formation.
The temperature in the knee joint should gradually decrease; it is recommended to apply ice compresses for a week or two.
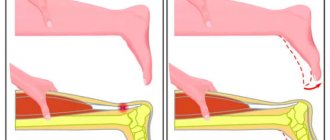
The range of movements should gradually increase, and by the end of the 6th week reach normal values. If the amplitude of knee flexion/extension is not restored, then it can be argued that physical rehabilitation is or was performed incorrectly. If the leg does not bend or straighten completely, then the reason for this is joint contracture, which has developed as a result of the formation of rough adhesions between the tendons and nearby tissues. An untreated problem is solved through manual redressing and long and intensive work on the development of a stiff joint, exercise therapy, mechanotherapy, physiotherapy, etc. In severe pathology, an operation is performed to mobilize muscles and excise scar adhesions, followed by rehabilitation.
Such simulators allow you to gradually, with minimal discomfort, increase the range of motion of the knee joint. The patient inflates the cuff around the knee with air and, due to the pressure applied, the leg straightens.
Regardless of the type of operation, the risk of the formation of pathological formations in the form of rough adhesions and scars is considerable. After surgery, the lower limb remains in a state of low motor activity. To counteract the development of a severe adhesive process, doctors recommend starting from the next day after the intervention a complex of physical therapy, which will not interfere with the healing of the knee, and at the same time will prevent contractures and muscle atrophy.
In advanced cases, surgeons are involved in solving the problem.
After surgery, in the long-term recovery period, the following excess may occur: the lateral ligament of the knee does not support, which is expressed by lateral instability of the joint, bowing of the leg during rotational movement. If reconstruction of a torn fibular or tibial collateral ligament (ACL) was performed, it is possible that, due to irrational loads, the integrity of the fragile ligamentous structure that stabilizes and strengthens the articular apparatus was again damaged. If you have this symptom, you should be examined by an orthopedic doctor! Only after identifying a reliable cause of instability, a specialist, having selected an effective set of therapeutic measures, will be able to direct therapy in the right direction.
If the operation to reconstruct the ligaments is carried out well, then they become no less strong than before the operation.
Muscular structures trigger the bony joint into working condition. Postoperative rehabilitation of the knee joint strengthens and increases the endurance of the muscular-ligamentous system.
The patient's condition after knee replacement
The condition after knee replacement almost directly depends on the general health of the patient, the severity of the injury for which the operation was performed, as well as other factors. In any case, the patient will feel pain in the knee area for some time. This is due to the fact that after an injury the joint becomes damaged. But if it is replaced during surgery, then the muscles and ligaments located nearby. retain their original condition. And since the knee was practically immobilized before the operation, the muscles atrophied a little. You can return them to full functionality with the help of special physical exercises. But before that, you first need to deal with the pain that occurs after knee replacement.
Principles of rehabilitation after knee surgery
Rehabilitation treatment includes:
- careful planning of rehabilitation taking into account the specific medical problem and body criteria;
- developed daily schedule, including medication, procedural, and physical rehabilitation;
- the principle of balance, gradualism and dosing of physical activity;
- careful control over the patient’s performance of all treatment and rehabilitation procedures.
Each individual patient needs his own recovery program after knee surgery, specially developed for him by a board of specialists (surgeon, rehabilitation specialist, neurologist, physiotherapist, exercise therapy methodologist, etc.). Therefore, there is no single rehabilitation scheme for all patients. Recovery goals:
- early activation of the patient;
- prevention of congestion in the respiratory system;
- stimulation of regional blood circulation and lymphatic drainage in the lower extremities;
- reduction in the secretion of pathological fluid in the knee;
- rapid elimination of pain syndrome;
- active prevention of muscle wasting, contractures and adhesions;
- stimulation of metabolic metabolism and tissue regeneration;
- preventing the emergence of an infectious environment in the operated tissues;
- restoration of lost limb functions.
Your doctor will tell you how to develop your knee after surgery. Don't self-medicate! Incompetent tactics will prevent a favorable prognosis. Take this fact into account if you don’t want your knee to bend and hurt after undergoing major surgery.
Support and consolidation of results.
In addition to regularly performing exercises aimed at maintaining the achieved results, it is important to comply with a number of conditions:
- Do not lift heavy objects, and monitor the load on the joint.
- Exclude active sports such as football, basketball, volleyball, running, skiing.
- Replace them with calmer ones - swimming, tennis, Nordic walking.
- For independent maintenance of physical fitness, exercise equipment is ideal, in particular, an exercise bike, step, and arthromot.
The prosthesis imposes a number of other restrictions:
- If there is metal in the implant, magnetic resonance imaging cannot be used for diagnosis.
- In the first months, you need to avoid exposure to high temperatures, including saunas.
- You cannot perform sudden movements, strikes, or swings with the operated leg.
- Control body weight.
- Check with your doctor regularly. Especially in case of pain, swelling, hematomas in the implant area, or any infectious diseases.
Physiotherapeutic procedures
You will be prescribed physiotherapeutic procedures:
- laser treatment;
- electromyostimulation;
- UHF treatment;
- extracorporeal shockwave therapy (shock wave therapy);
- ion-galvanization;
- magnetic therapy;
- hot paraffin treatment (only in the later stages!).
Electrical stimulation is one of the options for physiotherapy.
Exercise therapy and physiotherapy will help:
- relieving spasms from tense muscle structures and increasing the tone of weakened and atrophied muscles;
- activation of microcirculation and blood flow in the lower limb;
- stimulating metabolism in joint structures;
- relief of painful manifestations and swelling.
Elastic bandaging
For 6 weeks after surgery, there is a risk of blood clots and swelling. Therefore, a specialist prescribes elastic bandaging in the early period, and compression stockings in the later period. The degree of compression of these medical devices is selected by the orthopedist, taking into account the volume of intervention and the predisposition factor to thrombosis. Applying an elastic bandage and wearing compression garments prevents the development of deep vein thrombosis.
Bandages are used less and less; they hold up very poorly when moving. This type of compression knitwear is most often used.
The technique of how to bandage a leg will be taught to you in the hospital. First, the bandaging is carried out by a doctor, and when you return home you will have to do it yourself. Be attentive to everything the medical staff says and teaches you while you are still in the clinic or rehabilitation center.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
What Happens During the Early Recovery Period
After the end of the operation, 2-3 days pass before the drainage tube is removed. This is the early recovery period, during which:
- painkillers and antibacterial drugs are administered;
- an aseptic bandage is applied to the incision area;
- apply an ice pack;
- It is recommended to use a special bandage or elastic bandage for immobilization to prevent swelling.
Any load on the knee is contraindicated. At this stage of treatment for arthrosis or osteoarthritis, it is important to observe bed rest. The bed should be such that the operated leg is in a stable position. Loads on the limb must be strictly dosed - according to the recommendation of the attending physician.
Orthosis and crutches are mandatory companions for the patient in the early recovery period
Medication provision
No knee rehabilitation is complete without medication. After any type of orthopedic surgery, three main types of medications are prescribed:
- antibiotic against local infection;
- an anticoagulant that thins the blood and has an antithrombotic effect;
- non-steroidal anti-inflammatory drug.
It may be necessary to prescribe dietary supplements or products from a series of chondroprotectors to replenish articular tissues with valuable nutrients, which will help activate reparative and regenerative reactions.
Taking antibiotics is critically important; without this, very unpleasant consequences can occur in the form of an infectious complication.
Anti-pain medications should be used only as needed, and should not be overused if the discomfort in the knee is not severe. In the first 3 days, in order to avoid frequent use of harmful medications, doctors advise applying an ice bag to the knee joint every 30-40 minutes. Cold dry compresses are quite effective in soothing pain and reducing swelling. Drugs from the NSAID category should not be used immediately before exercise, so that you can feel your leg well during training. If the pain is dulled by medication, there is a danger of making the wrong movement and causing unwanted injury to the still vulnerable limb.
Is it painful to work out an operated knee without prior anesthesia? Of course, what to hide, at first it will not be easy, what to do exercises, what to move around. But there is no escape from pain; this is a normal reaction of the body to temporary intervention. Every day you will feel better and better, and after about 7-10 days the unpleasant sensations will stop bringing you such suffering. The main thing is don't give up! Do not stop following the instructions given by the specialist. Naturally, immediately inform your supervising doctor or physical therapy trainer about all your sensations, especially if the unpleasant symptoms begin to intensify.
Reasons for performing knee replacement
When knee pain appears, it is always, at a minimum, unpleasant.
At first, painkillers and massage may still help. But when the pain becomes unbearable, the only option to get rid of it is knee replacement. This surgery removes part of the joint and replaces it with a polymer or metal process. But not everyone knows what to do after knee replacement surgery and how to get rid of subsequent pain. Many forums have advice on what to do after endoprosthetics. But not all of this advice can be trusted. Most often they are given by people who have nothing to do with medicine. But endoprosthetics is a medical intervention, so only specialists can advise anything. Before the operation, the patient must be examined for sensitivity to anesthesia and the presence of possible allergic reactions. The operation itself lasts only about 2 hours. But after it comes a long period of rehabilitation. and here you need to be very attentive to your body and try to follow what the doctors recommend.
When are surgical sutures removed?
Stitches on the knee after surgery are usually removed on the 10th day. During this time, the final fusion of the wound edges, fixed with surgical sutures, should occur. If the incision is minor and has healed quickly, your stitches will be removed on the 7th day. In general, the ability to regenerate soft tissues that were dissected at the time of surgery varies from person to person. In elderly patients or people suffering from diabetes, final healing may take place only on days 12-14.
Judging by the scars in this patient, partial replacement and arthroscopy were performed on the left knee joint. The seams look good.
Recovery at home
If you decide that the recovery period after hip or knee replacement will take place at home, you need to prepare your apartment.
In the bathroom, handrails are installed for support during bathing, a bench is installed, and an anti-slip mat is placed. When taking hygiene procedures, relatives need to accompany the ward. Teach him to get in and out of the bathtub, holding the handrail tightly with his hands.
You may also be interested in the article: How to obtain patronage for an elderly person
Wires, carpets, and other obstacles are removed from the path of the household. Increase the height of a kitchen chair with a folded blanket or purchase a bar stool. Raise the bed, placing the second mattress. It is placed in the room in such a way that it is convenient to approach and lie down.
A bedside table or small table is placed next to the bed. It contains essential items:
- glasses;
- cellular telephone;
- phone charger;
- a bottle of water;
- flashlight;
- table lamp.
The lighting in the apartment is made optimal: so that the light does not dazzle and is not dim. Otherwise, a person will not be able to see the obstacle on the way and get around it. Discuss with your doctor what exercise equipment should be used to develop joints. Devices can not only be purchased. There are companies that provide devices for rent.
The recovery period of a joint after prosthetics is easier and faster in people with normal weight. Therefore, it is worth fighting extra pounds, eating healthy foods, and sticking to a diet. It is useful to introduce foods rich in calcium, protein, collagen into the diet: milk, fish, meat, jellied meat, fruit jelly.
Shoes for a relative with a prosthetic joint are chosen to be comfortable, preferably orthopedic, without laces. Purchase crutches or a walker with four legs for walking. They must have tips made of non-slip materials. Normally, a person starts walking with a cane 2 months after installation of the prosthesis.
Elderly people need more time to adapt to the joint.
Patients begin to walk without a cane after six months. The mode of walking in the fresh air is: several times a day for 30 minutes. A limb with a prosthesis begins to be used as a support when walking after 2 months.
You should avoid physical activity and do not carry heavy objects. If redness and swelling in the joint area or fever appear, you should immediately consult your doctor.
Exercise therapy for the knee after surgery
Only with a comprehensive combination of exercise therapy with other therapeutic and health tactics prescribed by the doctor will you achieve results in normalizing the motor-support potential of the leg.
How long recovery lasts was indicated in previous chapters. Let's repeat, 2-6 months. The duration of the recovery process is influenced by 3 criteria: surgical tactics, the degree of surgical aggression and the personal characteristics of the patient.
The fundamental goals of exercise therapy after knee replacement, arthroscopy to restore ligaments, knee meniscectomy and other surgical treatment methods are to increase muscle tone and endurance, and develop the knee until the most complete recovery possible. A competent physical regimen in stages can be recommended by a highly competent doctor - the operating orthopedic surgeon, rehabilitation specialist or exercise therapy specialist.
Orthosis training.
Possible consequences after arthroscopy
Arthroscopy is considered a modern method for diagnosing and treating joints. This technique is one of the few where the risks of complications are reduced to almost a minimum. But still, like any operation, surgery on the knee joint has certain risks: Infectious complications. Damage to articular cartilage. Thrombosis of blood vessels. Bleeding Such consequences occur infrequently, in approximately 0.1% of cases. To avoid complications, we strongly advise you to contact only trusted medical centers where real specialists work. Monitor your health carefully after surgery. If severe pain, increasing swelling, shortness of breath and other worrying signs appear, consult a doctor immediately.
How to develop a knee after surgery: methods
Immediately after 12-24 hours after surgery, for 3-7 days, you will be advised to perform a light form of exercise in a lying position. The frequency of repetitions and the daily number of sessions is determined by a specialist.
- Carefully lift the problematic leg off the bed, lifting it 20 cm from the surface. The healthy leg is bent at the knee at this time. Hold the position of the raised leg for 5 seconds, then carefully return the limb to its original position.
Work smoothly.
- Slightly bend both legs (support on the heels), tense the thigh muscles. On the count of ten, relax.
Arms along the body, torso relaxed.
- Perform an isometric contraction of the gluteal muscles while holding the tension for 5-8 seconds.
Do this until you feel a slight burning sensation.
- Lying on your back, placing a cushion made of a towel under your foot, apply pressure to it, trying to bend your leg. After 5 seconds, relax. The ligaments of the popliteal zone and the muscle structures of the lower leg will be strained.
The main thing is not the effort, but the smoothness of the increase in load.
- Legs lie flat on the bed.
Make movements with your feet towards and away from you, without lifting your heel off the surface. It is useful to alternately spread your legs to the sides, sliding along the sheet. Do it very slowly.
Gentle exercises are gradually supplemented with more complex exercises. Let's give examples of some of them.
- Stand against a wall or near a chair to secure yourself.
Slowly raise the affected limb straight forward. Having reached an angle of 45 degrees, hold your straight leg on the weight for 5 seconds, and also smoothly return it to the starting position. Don't forget about the hand rest.
- Perform a similar task as the one described above, but only with the foot facing outward.
- Holding the back of the chair, move the limb to the side (without jerking!), lifting it a short distance.
Hold for a few seconds and return to IP. Keep your balance. - Lie on your back and place a cushion under your operated knee.
With support on the roller, straighten your leg. Hold the position of the straightened leg for about five seconds, then slowly return to the original position. Smooth execution is the key to avoiding injury.
After 2-3 weeks, they move on to active training, where the following type of classes will already be present:
- half squats near a chair (the angle of bending of the knees does not exceed 90 degrees);
Try to rest on the entire area of your foot. - stretching exercises, for example, bending the leg with grabbing the foot with the hand and pulling it towards the buttocks;
If you move your pelvis forward, the stretching effect will increase. - performing resistance tasks using a rehabilitation expander or rubber band;
You can come up with a lot of exercises with a tourniquet. - stepping (front and side) onto the step platform with the body weight transferred to the leg that was operated on and with its further straightening;
Alternate legs while performing this exercise. - exercise on an exercise bike, using a light pedal resistance mode, gradually increasing it to medium, heavy.
This is the best equipment for rehabilitation. - walking on a treadmill, start at a slow pace and walk for 10 minutes, then gradually increase speed and time;
- aqua gymnastics and swimming in the pool.
We recommend practicing in the pool for life.
When performing physical tasks, listen to your own feelings: you must control the threshold of acceptable pain, not allowing it to intensify. Overloading is unacceptable! Unoptimized loads will cause painful swelling; how long it lasts depends on the degree of damage caused to vulnerable knee structures. But the saddest thing is that swelling and pain will slow down the recovery process, interfere with the normal development of the joint, and increase the time until your final recovery.
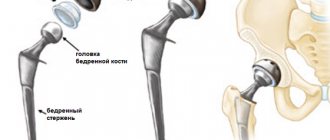
Joint replacement surgery
Joint endoprosthetics is a complex operation in which a prosthesis is inserted in place of a damaged joint. For this purpose, a metal, ceramic or high-quality plastic implant is used. The endoprosthesis is fixed, depending on the indications, using a cemented or cementless method.
Prosthetics may be prescribed in the following cases:
- Arthritis or arthrosis in the final stages.
- Injuries for which other methods of restoring mobility are not applicable.
- For dysplasia - congenital or acquired abnormalities of the joints.
- Tumors in the head and neck of the femur.
- With necrosis of cartilage and bone tissue, due to impaired blood supply in the area of deformation.
- Complications of joints due to obesity.
The operation can be performed on the knee, hip, shoulder, ankle, or elbow joints.
Please note that in the presence of the following diseases, surgery is contraindicated:
- Vein thrombosis;
- Blood clotting disorder;
- Tuberculosis;
- Infectious skin lesions;
- Diabetes;
- Kidney failure, etc.
In some cases, arthroscopy is performed before implantation - an operation with minimal intervention (through two or three punctures), which allows you to clarify the diagnosis and also prepare the joint for endoprosthetics. You can read more about arthroscopy here -. The success of the surgical procedures depends on postoperative rehabilitation. Therefore, it is very important to take this seriously and responsibly to return all functions.