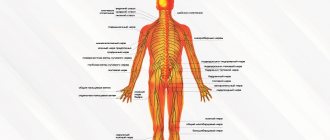
Radiculopathy (radicular syndrome) is a neurological syndrome caused by irritation of the spinal roots. Each root corresponds to the body of its vertebra and is located at the same level with it. It passes through the narrow intervertebral foramen and is surrounded by muscles, ligaments and choroid plexuses. Problems with any of these formations can cause irritation and/or compression of the root.
Thus, the origin of radiculopathy and the occurrence of pain is determined by the position of the roots.
Causes
Possible causes of radicular syndrome:
- mechanical injuries
- weak back muscles
- metabolic disorders
- hormonal disorders
- age-related degenerative changes
- chronic inflammatory process
- consequences of surgical interventions
- postural disorders (scoliosis, etc.)
- heavy physical (dynamic and static) loads
- gravity loads
- spinal abnormalities
- tumor processes
- narrowing of the spinal canal (due to displacement of the vertebrae)
- narrowing of the foraminal (intervertebral) foramina
- protrusion and herniation of intervertebral discs
The development of degenerative-dystrophic changes in intervertebral discs occurs over time as a result of a combination of factors. Changes in the intervertebral discs are manifested by thinning and loss of elasticity. In the absence of adequate treatment, their destruction occurs.
Thus, the conditions for disc protrusion are created. The process is carried out in the thinnest area of the outer fibrous ring.
When the fibrous membrane ruptures, the core of the disc protrudes.
The initial stage is characterized by the formation of intervertebral disc protrusion. In this case, rupture of the fibrous ring does not occur.
Both in the case of rupture of the fibrous ring, and in the case of protrusion formation, when the ring remains intact, the vertebral disc acts on the nerve roots, which are located on the sides of the spinal column. At the initial stage of the process, irritation affects only the membranes. Subsequently, if the process is not stopped, compression of the roots occurs. This process is called discogenic radiculopathy.
Radicular syndrome occurs in two stages:
- at the first, neurological stage, there is an increase in sensitivity, sharp and unexpected acute pain, characteristic muscle tension, pain in the paravertebral points when pressed
- in the second, neurotic stage, there is a decrease in sensitivity in the area of innervation of nerve bundles formed from damaged roots; During a medical examination, the extinction of the periosteal reflex is revealed and partial malnutrition is diagnosed. The muscle tension and intense pain characteristic of the first stage are preserved.
What is lumbosacral radiculopathy?
Radiculopathy (or, in other words, radiculitis) is a disease of the human peripheral nervous system that occurs against the background of inflammation, pinching, irritation or damage to the spinal nerve roots.
Clinical picture of the disease
The main symptom that provokes a person to take active diagnostic and therapeutic actions is pain. At the moment when the intervertebral hernia pinches the nerve roots of the spinal column, the so-called “lumbago” occurs .
Shooting pains are sharp, sharp, burning in nature . They appear when the ligamentous apparatus is irritated, and the muscles of the back and pelvis are very tense. Such pain can radiate to the back of the thigh, and also appear in the buttocks and popliteal areas. The patient tries to bend his leg at the knee in order to somehow relieve the pain.
When moving, the pain intensifies. In advanced cases, paresthesia, paresis, numbness, and a sensation of “pins and needles” in the affected area may occur . It may be difficult for the patient to move his legs or lift them from the bed.
Radiculopathy develops as a result of pinched nerve root in the lumbar spine
If the sciatic nerve is affected, the patient may experience pain in the back of the leg. The skin of the injured leg becomes dry, cold, and cyanosis appears.
Hernial protrusions can compress blood vessels, which will lead to a decrease in blood flow in the veins and arteries. This in turn will lead to poor circulation and increase the risk of infarction of part of the spinal cord.
Prevalence of the disease
Radiculitis is considered one of the most common diseases of the spinal column. Pathology most often develops in men and women after 40 years. The risk of developing the disease increases in those who constantly experience dynamic or static stress .
Symptoms
Each type of radiculopathy is characterized by the presence of a specific set of symptoms.
The general symptom is pain of varying severity. The pain can range from not too intense to quite significant. Acute pain often limits the mobility of the limbs and body and makes it impossible to lead a normal lifestyle, which affects the patient's quality of life.
Symptoms of cervical radiculopathy
Most often, acute pain occurs in the morning. It could be:
- pain in the neck
- headache (sometimes very intense)
- shoulder pain
- arm pain
- soreness and/or stiffness of the neck muscles
- paresthesia (impaired sensitivity, accompanied by a feeling of burning, tingling, numbness, coldness)
- metabolic disorders (dry skin, peeling, coldness of the skin when touching the affected area)
Important! If you find yourself with similar symptoms, treatment should be started without delay. You should not rely on “home” methods. They can only give a temporary effect and will not eliminate the cause of the disease.
Only a qualified neurologist will accurately determine the type of disease, prescribe an examination and adequate treatment.
Symptoms of thoracic radiculopathy
Along with the general symptoms characteristic of all types of radiculopathy, the following are observed in the chest form:
- girdle pain, pain between the shoulder blades, behind the sternum and in the area of the lower ribs
- pain radiating to the shoulder and armpit
- pain radiating to the middle finger
- triceps weakness
- During a medical examination, a decrease in the tricepital reflex is detected
It is difficult to diagnose the disease yourself. It should be borne in mind that the symptoms of thoracic radiculopathy resemble the symptoms of angina pectoris and other dangerous diseases.
Self-treatment can cause irreparable harm!
Symptoms of lumbosacral radiculopathy
Lumbosacral neurological syndrome is characterized (along with similar symptoms in other types of radiculopathy):
- intense pain in the foot, hip and buttock
- acute pain in the lower back, radiating to the limbs
- impaired motor function due to awkward bending or sudden movement
- loss of sensation in the lower limb, weakening of the muscles of the lower limbs
Chronic radiculopathy: new treatment options
Danilov A.B., Zharkova T.R.
Nerve root compression (radiculopathy) accounts for 8 to 10% of other causes of back pain [1-4,9]. Up to 90% of radiculopathies are caused by herniated intervertebral discs, and in more than 80% of cases, pathology is detected in the lumbar region. In 48% of cases, hernias are localized at the level of L5-S1 of the lumbosacral region, in 46% of cases - at the level of L4-L5; the remaining 6% at other levels or at several levels of the lumbosacral region. In 80% of patients, pain goes away under the influence of treatment in a fairly short period of time - from several weeks to a month, but in the remaining 20% of patients it becomes chronic and relapsing [14]. This disease most often occurs between the ages of 45 and 64 years.
From the point of view of pain mechanisms, radiculopathy is today considered as a mixed pain syndrome, where both nociceptive and neuropathic components are present [2,5,8]. This approach allows for differentiated pharmacotherapy of pain depending on the severity of a particular component. For the treatment of the nociceptive component, it is recommended to use simple analgesics or nonsteroidal anti-inflammatory drugs (NSAIDs), which are known to relieve nociceptive pain well. In the pharmacotherapy of neuropathic pain, anticonvulsants, antidepressants and opioid analgesics are most often used [2]. Anticonvulsants are more often used to relieve neuropathic pain of a burning and “shooting” nature. One of these anticonvulsants, the most recognized and tested in the world, is gabapentin [6,12,13,16]. The mechanism of its action is associated with the influence on the central mechanisms of pain at the level of the posterior horn. Acting on a special alpha-2 subunit of calcium channels on the presynaptic membrane in the terminals of a sensory neuron, gabapentin blocks the entry of calcium into the cell and thereby impedes the release of pain mediators (glutamate, substance P) into the synaptic cleft. This disrupts the transmission of pain signals from the peripheral neuron to the central one. As a result, there is a decrease in central sensitization, an improvement in the neurotransmitter balance towards increased analgesic GABAergic effects and a reduction in the effects of glutamate, the main neurotransmitter of pain [16].
In order to differentiate the treatment of pain in radiculopathy, it is very important to assess the representation of nociceptive and neuropathic pain mechanisms in each specific case. A number of questionnaires have been developed to assess the reliability of the presence of neuropathic pain. The DN4 questionnaire consists of 10 items regarding the characteristic clinical characteristics of neuropathic pain [7]. As a result of the questionnaire and neurological analysis, the total score is determined (from 0 to 10). Pain is assessed as neuropathic with a score of at least 4. The PainDETECT questionnaire combines a diagram of the distribution of pain disorders in the form of a picture with a VAS scale and a questionnaire aimed at identifying spontaneous and evoked symptoms of neuropathic pain [11]. Also, using the drawing, the nature of the pain is assessed. The questionnaire most fully reflects all possible pain parameters and allows you to visually monitor the dynamics of the pain syndrome. A score greater than 19 indicates that the patient likely has a neuropathic component of pain. From 13 to 18 points - the indications are ambiguous, but a pain component may occur.
The purpose of this study was to evaluate the pain syndrome in chronic radiculopathy from the point of view of the severity of the neuropathic component of pain and to evaluate the clinical effectiveness of the drug Tebantin (gabapentin) for targeted therapy of this component.
Research material
The group of patients consisted of 37 people with chronic lumbosacral radiculopathy (women - 59%, men - 41%). Inclusion criteria were: chronic pain syndrome due to discogenic radiculopathy L4-L5, L5-S1 (lasting at least 3 months). Each patient was informed about the purpose of taking the drug, possible side effects of therapy, and signed an informed consent. The average age of patients receiving therapy was 47.62±13.36 years.
Research methods
Clinical and neurological examination included collection of anamnesis of the disease, general somatic and neurological examination. To confirm the presence of intervertebral disc herniation at the L4-L5 and/or L5-S1 level, all patients underwent magnetic resonance imaging.
For each patient, a clinical questionnaire was filled out, including a passport part, a description of the subjective characteristics (descriptors) of the pain syndrome, the intensity of each descriptor was assessed on a visual analogue scale, the localization of pain, the duration of the pain syndrome, the number of exacerbations in the history, the course of the disease, provoking factors and communication with physical activity, accompanying symptoms, pain relief measures, as well as complaints during the interictal period and concomitant diseases. The localization and nature of sensory disorders were assessed in the neurological status. The presence or absence of phenomena of stimulus-dependent pain symptoms was also taken into account: allodynia, hyperalgesia, paresthesia and dysesthesia. Sensory disorders were recorded on a picture in the patient's questionnaire. Tendon reflexes and strength in the limbs were assessed. According to Khabirov’s questionnaire, the index of muscular-tonic syndrome was calculated [4].
Psychometric testing included an assessment of the severity of depression using the Beck Questionnaire, an assessment of the level of reactive and personal anxiety according to Spielberger, and an assessment of the quality of life using the SF36 questionnaire.
Treatment was carried out according to the following scheme. Tebantin monotherapy at a dose of 1800 mg per day (600 mg 3 times) for 6 weeks with preliminary titration: on the first day - 300 mg/day; on the 2nd - 600, on the 3rd - 900, on the 4th-6th - 1200, on the 7th-10th - 1500 and from the 11th day - 1800 mg/day. in three doses of 600 mg. The intensity of the pain syndrome was assessed on a visual analogue scale (from 0 to 10) at each week of treatment, as well as the reliability of the presence of a neuropathic component of the pain syndrome was assessed using the DN4 and PainDetect questionnaires before and after treatment.
results
The average duration of the disease in the group was 3.4±3.9 years and ranged from 6 months to 18 years. The average age of onset of the disease was 44.1±12.7, in men the pain syndrome was first detected at the age of 40.3±11.5 years, in women - at the age of 46.6±13.1 years. The number of exacerbations in the group examined during the period of the disease was 2.9±2.3.
Four types of pain syndrome were identified among patients. Continuous pain, slightly varying in intensity, was noted in 8 patients (21.6%). Continuous pain with periodic, rare attacks was detected in 6 patients (16.2%). 9 patients (24.4%) characterized the course of their pain syndrome as attacks of pain without pain between them. Most often, 14 patients (37.8%) experienced frequent attacks of pain, accompanied by pain in the intervals between them.
All examined patients noted the occurrence of pain attacks at different times of the day. 7 patients (19%) indicated that pain attacks occur exclusively at night, 18 patients (49%) complained of pain that occurs only during the day, and 12 patients (32%) noted the occurrence of pain both during the day and during the day. at night.
A significant group of patients - 26 people (70.2%) indicated that physical activity increases the severity of pain. 4 patients (10.8%) considered hypothermia to be a factor provoking pain. 16 patients (43.2%) noted pain when walking, 11 people (29.8%) - while sitting.
According to clinical neurological examination and based on subjective complaints of patients, it was revealed: 23 patients (62%) complained of shooting pain, 20 patients (54%) had burning pain, 24 patients (65%) had compressive pain, 12 patients had aching pain. (62%), allodynia was detected in 16 (43.2%), paresthesia - in 29 patients (78%).
Table 1 shows the characteristics of the pain syndrome before and after treatment with Tebantin. There was a significant decrease in the intensity of burning, squeezing, pressing, aching pain, pain like electric shocks, and a significant decrease in the frequency of burning pain during treatment. A decrease in the intensity of allodynia, frequency and intensity of paresthesia was noted.
26 patients (70%) complained of numbness. Hypalgesia was detected in 23 patients (62%), 11 patients had a decrease in pain sensitivity in the zone of innervation of the L5-S1 root, in 11 patients - in the zone of innervation of the L4-L5 root, in 1 patient - in the zone of innervation of the L4-L5 and L5 roots -S1. Hyperalgesia was observed in 9 patients (24%), in 4 people - in the zone of innervation of the L5-S1 root, in 5 - in the zone of innervation of the L4-L5 root.
A positive Lasegue test was detected in 67% of patients, a Lasegue cross-test was detected in 40%. Table 2 shows the data of the neurological examination of patients before and after treatment. There was a significant decrease in the frequency of hyperesthesia, the frequency of occurrence of the Lasègue test and the cross-Lasègue test during treatment.
A decrease in the knee reflex was noted in 6 patients (16.2%), the knee reflex was absent in 3 patients (8%). A decrease in the Achilles reflex was detected in 5 patients (13.5%), its absence in 25 patients (67.5%).
Among the examined group of patients, an analysis of the tension of the multifidus muscles of the back and the erector spinae muscle was carried out. The muscles were palpated at the lumbar level with the patient tilted forward by 10-15°. During palpation, the severity of spontaneous pain, tone, muscle soreness, duration of pain and the degree of pain irradiation during palpation were assessed. According to Khabirov's questionnaire, the index of muscular-tonic syndrome was calculated. 12 patients (32.4%) had the first degree of muscular-tonic syndrome, and 25 patients (67.6%) had the second degree of muscular-tonic syndrome. No pronounced manifestations of muscular-tonic syndrome were found in patients with chronic pain due to lumbosacral radiculopathy.
According to the DN4 questionnaire, the average score was 5.45±1.57, 90% of patients were ?4; according to PainDETECT - 13.78±3.10, in 65% of patients ?13 (Fig. 1). The severity of pain according to VAS among patients in the examined group was 7.45±1.83. The dynamics of VAS during treatment with Tebantin by week are shown in Figure 2. A significant decrease in pain according to VAS was noted already in the 3rd week of treatment.
The dynamics of clinical and psychological characteristics of patients before and after treatment with Tebantin are presented in Table 3.
There was a significant decrease in the severity of depression and a significant improvement in the quality of life of patients during treatment.
Tolerability of the drug in most patients was satisfactory; 5 patients experienced mild drowsiness and slight dizziness during the first 4-5 days of use.
To analyze predictors of treatment effectiveness, two polar groups of patients were assessed: with low treatment effectiveness and high treatment effectiveness relative to VAS data (Table 4).
Treatment with Tebantin was most effective in patients with a longer disease duration and a greater history of exacerbations. In patients in this group, pain more often occurred at night; along the way, these were frequent attacks of pain, accompanied by painful intervals between them. Patients with higher treatment effectiveness initially significantly more often complained of shooting, burning pain; they more often had symptoms such as allodynia, paresthesia, numbness, and a positive Lasegue symptom. More effective treatment was observed in patients with initially higher scores according to the DN4 and PainDETECT questionnaires.
Discussion
Currently, several mechanisms of pain formation in compression radiculopathy are being considered [10]. In addition to direct mechanical compression of the root, damage to the nociceptors of the intervertebral disc itself can be a source of pain. In addition, the inflammatory process plays a certain role, when inflammatory mediators, locally acting on nerve endings in tissues, are also involved in the generation of pain. Thus, pain in radiculopathy is considered to be mixed, with nociceptive and neuropathic components present [8,10]. Large epidemiological studies indicate that in 20-35% of patients with discogenic radiculopathy, the neuropathic component predominates [10]. The cause of the formation of the neuropathic component may be mechanical compression of the nerve root (mechanical neuropathy) and/or its irritation under the influence of inflammatory mediators (inflammatory neuropathy) [10]. Specific characteristics of the neuropathic component in back pain are complaints of shooting, deep excruciating, pulling, aching, boring pain, burning, allodynia, Lasegue's symptom, painful numbness [15].
According to our study, the neuropathic component was identified in 90% of patients according to the DN4 questionnaire and in 65% of patients according to the PainDETECT questionnaire, which confirms the data that the pain syndrome in radiculopathy is mixed, with the leading role of the neuropathic component. It should be noted that in our study, the DN4 questionnaire turned out to be more informative and sensitive in diagnosing the neuropathic component of pain than the PainDETECT questionnaire.
The use of the drug Tebantin in our study was aimed at clarifying the mechanisms of pain in radiculopathy and the possibility of targeted therapeutic effects on it.
The results of the work showed the high effectiveness of gabapentin (Tebantine) in reducing the neuropathic component of pain. This, on the one hand, indicates that the neuropathic component plays a significant role in the formation of pain in radiculopathy, and on the other hand, indicates the possibility of effectively influencing this component with the help of gabapentin (Tebantin). It should be emphasized that as a result of pain reduction, a significant improvement in psychological status was noted (decreased depression and anxiety).
Thus, the diagnosis of the neuropathic component in back pain is important from the point of view of differentiated pharmacotherapy. The drug Tebantin has a clear positive effect predominantly on the neuropathic component in the structure of mixed pain syndrome in chronic radiculopathy and to a lesser extent affects the characteristics of the nociceptive component.
The results of the study allow us to conclude that it is advisable to clarify the severity of the nociceptive and neuropathic components in back pain in order to select an adequate drug from the group of NSAIDs to influence the nociceptive component and gabapentin to treat the neuropathic component. It is likely that in most cases of chronic radiculopathy, simultaneous administration of NSAIDs and gabapentin in an adequate ratio is necessary to influence both components of the pain syndrome, which can positively affect the effectiveness and timing of pharmacotherapy and rehabilitation.
Literature
1. Pain syndromes in neurological practice//Ed. Veina A.M. - M.: MEDpress-inform, 2001. 2. Danilov A.B., Davydov O.S. Neuropathic pain, 2007 3. Podchufarova E.V., Chronic back pain: pathogenesis, diagnosis, treatment.// RMZh.- 2003. - T. 11.- No. 25.- P. 32-37 4. Khabirov F.A. . Guide to clinical spinal neurology. Kazan, 2006. 5. Baron R., Binder A. How neuropathic is sciatica? The mixed pain concept. Orthopade., 2004 May; 33(5):568-75. 6. Birklein F. Mechanism-based treatment principles of neuropathic pain. Fortschr Neurol Psychiatr., 2002 Feb; 70(2):88-94. 7. Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, Cunin G, Fermanian J, Ginies P, Grun-Overdyking A, Jafari-Schluep H, Lanteri-Minet M, Laurent B, Mick G, Serrie A, Valade D, Vicaut E. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005 Mar; 114(1-2):29-36. 8. Brisby H. Pathology and possible mechanisms of nervous system response to disc degeneration. J Bone Joint Surg Am. 2006 Apr; 88 Suppl 2:68-71. 9. Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976). 1987 Apr; 12(3):264-8. 10. Freynhagen R, Baron R. The evaluation of neuropathic components in low back pain. Curr Pain Headache Rep. 2009 Jun; 13(3):185-90. 11. Freynhagen R, Baron R, Gockel U, Tolle TR. painDETECT: a new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin. 2006 Oct; 22(10):1911-20. 12. Hansson P., Fields H., Hill R., Marchettini P., eds. Neuropathic Pain: Pathophysiology and Treatment, Progress in Pain Research and Management. Vol. 21. Seattle, WA: IASP Press; 2001: 151-167. 13. Junker U., Brunnmuller U. Efficacy and tolerability of gabapentin in the treatment of patients with neuropathic pain. Results of an observational study involving 5620 patients. MMW Fortschr Med., 2003; 145:37. 14. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA; Comprehensive review of epidemiology, scope, and impact of spinal pain. 2009 Jul-Aug;12(4):E35-70. 2005 Mar; 114(1-2):29-36. 15. Oostdam EM, Duivenvoorden HJ Description of pain and the degree to which the complaints fit the organic diagnosis of low back pain. Pain. 1984 Jan; 18(1):71-82. 16. Wiffen PJ, Collins S. Anticonvulsant drugs for acute and chronic pain (Review). The Cochrane Collaboration, 2008; 1-35. Key words of the article: Chronic, radiculopathy, new, possibilities, therapies
Source RMJ January 26, 2010, volume 18, no. special
Diagnostics
To make an accurate diagnosis and prescribe adequate treatment, a neurologist at the initial appointment conducts a neurological examination and determines the nature, duration and intensity of pain, as well as the nature of sensory and motor disorders. If necessary, additional instrumental studies may be prescribed in our clinic (X-ray examination, which helps determine the degree of deformation and degenerative changes, signs of instability and displacement of the vertebrae) or in diagnostic centers of the city (magnetic resonance imaging, computed tomography, electromyography, etc. .)
Preventive measures
Knowing what lumbar radiculitis is, you can draw up a plan of preventive measures. An important condition for preventing the disease and its exacerbations will be adequate physical activity on the spine. Considering all the exogenous and endogenous factors that provoke the disease, they need to be excluded as much as possible from everyday life.
A person diagnosed with lumbosacral radiculitis must perform a set of special exercises every day and periodically visit the pool. The sleeping mattress should be of medium hardness, comfortable for the back.
Treatment of radiculopathy
The beginning of treatment is complete rest and the use of various local remedies.
Since the effectiveness of treatment depends on establishing an accurate diagnosis and clarifying the cause that caused compression of the nerve roots, contacting a qualified neurologist is a priority. In some cases, the severity of the consequences will be less after quick help, which can be provided by an osteopath using manual or traction therapy (traction).
The next stage of treatment is pain relief. For this purpose, various medications are used, which can be prescribed in the form of injections, including intravenously, drips in the comfortable conditions of a day hospital.
The third stage is a recovery course, which starts the processes of physiological restoration of nerves, spinal roots and cartilage tissue of the intervertebral discs.
Patients are recommended massage, physiotherapy, and reflexology.
Qualified neurologists at our clinic, who have extensive experience in the treatment of radiculopathies, will give you individual advice and develop an individual treatment plan for you with subsequent rehabilitation.
Prevention and recommendations
Recommendations are general in nature and cannot be used for self-medication.
Psychotherapy, massage, physical therapy, swimming, physiotherapeutic procedures, sanatorium treatment (balneological resorts) are indicated. Galvanization, phonophoresis, amplipulse therapy, magnetotherapy, laser therapy, laser magnetic therapy give good results.
For follow-up treatment and prevention of recurrent attacks, radon, mineral and pearl baths are prescribed.
There are currently many modern and effective methods. Only a qualified neurologist can determine the advisability of prescribing them.
Don't risk your health!
FAQ
Is it possible to warm the lower back with a heating pad if you have radiculitis?
During an exacerbation of radiculopathy, it is recommended to keep the lower back warm. However, warming with a heating pad, a “blue lamp”, heated salt or sand is not recommended. This may increase swelling of the roots and lead to increased pain. You can use special belts, including those made of dog hair, etc.
I have a stomach ulcer. What painkillers can I take for sciatica?
Many drugs used for exacerbation of radiculopathy are not recommended for patients with a history of gastric and duodenal ulcers. Only a doctor can prescribe adequate treatment after examination. Don't self-medicate!
An MRI of my spine revealed a herniated disc. Should I delete it?
Indications for surgery to remove a herniated disc can be determined by a doctor during a consultation. Hernias most often do not require surgical intervention. It is necessary to observe a special protective regime, carry out preventive treatment and engage in physical therapy.
Why is it important to treat sciatica?
If radiculitis is not treated in time, it can develop into a chronic form. Then any, even minor, negative impacts (a cold back, lifting a heavy load), as well as an infection, careless movement, or even nervous stress, can trigger an attack of radiculitis. But what is even more dangerous is that the further development of the disease that causes radiculitis (osteochondrosis, spinal stenosis, etc.) can lead to very serious consequences, including disability. Thus, complete prolapse of a disc herniation in the cauda equina region (lower part of the lumbar spine) leads to paralysis of the legs and feet, dysfunction of the pelvic organs.
Muscle spasms, which are also often the cause of radiculitis, can also cause serious consequences. They impair the nutrition of the joints of the spine, which leads to its destruction, and therefore also require treatment. If an acute attack of radiculitis continues for several days, and the pain is accompanied by sensations of numbness, burning, and sipping in the limbs, you should immediately consult a doctor.
The diagnosis of radiculitis is made by a neurologist based on a detailed examination of the patient.
Treatment stories
Case No. 1
Patient S., 25 years old, after skiing and falling, felt a sharp pain in the lower back and numbness in the right foot. Started taking painkillers. However, due to the appearance of abdominal pain and heartburn, I was forced to give them up. On the second day I went to see a neurologist at the EXPERT Polyclinic. The patient was prescribed treatment and consultation with a gastroenterologist. The patient underwent a course of intramuscular and intravenous drip injections at the day hospital of the EXPERT Polyclinic. The pain syndrome has completely regressed, the numbness in the right foot has disappeared. Patient S. was consulted by a gastroenterologist. She underwent fibrogastroduodenoscopy (FGDS), which revealed an acute ulcer of the duodenal bulb. A gastroenterologist prescribed treatment for this issue.
Rehabilitation period
The recovery period after discectomy for lumbosacral radiculitis includes three periods. In the first week, the patient can gradually rise in bed, but it is strictly forbidden to sit. The duration of stay in a vertical position should not exceed 15 minutes. In addition, you should not lie on your stomach. You should always wear a corset for the lumbosacral region.
The patient spends the entire first week in the hospital. He may be prescribed antibacterial drugs, NSAIDs, hormonal and other drugs. On days 7-9, the sutures are removed and the patient is discharged home. Its transportation is carried out in a lying position.
In the first month, it is especially important to follow all doctor’s instructions. In order to support the lumbosacral region, the person continues to wear a special corset. Simple exercises are performed daily. Walking and being in nature is important. Usually, after 1.5-2 months, the sick leave is closed and the person returns to “normal” life, taking into account medical recommendations.