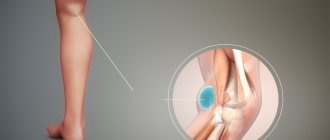
Inflammations localized in the joint of the lower extremities can provoke the formation of a neoplasm in the popliteal tissues, which is commonly called a Baker's cyst. Clinical manifestations of the neoplasm can be traced only after the cyst reaches a certain size, at which nerves and blood vessels are compressed.
Identification and approval of the diagnosis is carried out based on the results of laboratory and instrumental studies. Often the pathology is recorded in the fair sex, but it can also be observed in men.
What's happened
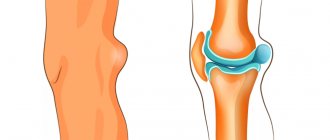
A ganglion cyst is a benign tumor-like formation that occurs near tendons or joints. Most often, an oval or round hygroma with synovial fluid inside is observed.
The disease is considered occupational, since the pathology in most cases affects laundresses and pianists who constantly overload their wrists. The resulting defect significantly impairs the functionality of the affected joint.
Small formations resemble peas, while large formations can reach 2.5 cm in diameter. The walls of the capsule consist of dense connective tissue, and the cavity itself is filled with a viscous serous fluid with mucous impurities.
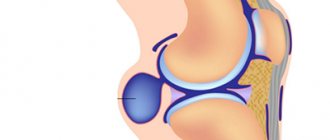
Pathogenesis of Baker's cyst
The pathogenesis of Baker's cyst under the knee is based on the non-standard anatomical location of the articular tissues, as well as the popliteal fossa.
Statistics show that in more than 40% of cases, when examining healthy people of different ages and genders, there is an intertendinous mucous bursa between the tendons of their muscular frame of the knee joint, which is not a pathology, but is considered an acceptable deviation from the norm.
The progression of joint inflammation and the formation of fluid in the joint tissues lead to an increase in the size of the cyst. The presence of a valve mechanism allows liquid to leak into its cavity, but does not allow reverse flow to occur.
Classification
Cystic defect is divided into single-chamber and multi-chamber. The first type is not elastic, while the second formations are capable of penetrating into tissue structures. Pathological formation is also divided depending on the location.
Dimensions for surgery to remove Baker's cyst of the knee joint
Not all patients require removal of a knee cyst.
A ganglion cyst on the head is caused by damage to the skull, resulting in the accumulation of cerebrospinal fluid. If the disease is not eliminated within the first two weeks, the pathological process becomes chronic.
Damage to the wrist or the back of the cyst is most often observed. Often defects occur on the fingers. Such formations cause pronounced discomfort and disrupt the functionality of the affected area.
If the wrist is affected, the joints become more difficult to bend and straighten. In most cases, hygromas on the hands compress the nerve endings, which causes intolerable pain. Therefore, they resort to immediate surgical removal.
If a benign cyst affects the wrist joint, then unpleasant symptoms occur when the hygroma reaches a large size. In this case, the defect compresses the blood vessels, impairing the functionality of the upper limb.
It is extremely rare that a ganglion tumor affects the foot in the ankle area. This type of pathology causes a lot of trouble - from severe pain to damage to the feet and deterioration in nutrition of the lower leg.
Cyst surgery on the coccyx
Surgery to remove a coccyx cyst is the most effective way to get rid of the disease.
The knee joint is affected by the accumulation of serous fluid in the synovial bursa. Because of this, the disease often affects athletes and people whose activities involve standing for long periods of time.
A tendon cyst is formed from the synovial membrane after various injuries. This lump is characterized by constant pain and therefore requires immediate surgical removal.
Epidemiology/Etiology
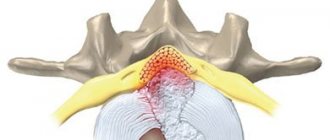
A Baker's cyst or popliteal cyst forms when there is an underlying problem with the knee joint, accompanied by an inflammatory reaction, which occurs as a result of the formation of intra-articular bodies in the presence of osteoarthritis, rheumatoid arthritis, rupture of the anterior cruciate ligament or meniscus, or because As a result of knee arthroplasty, particles appear, mainly from the polyethylene liner.
- A primary cyst is a formation not associated with pathology of the knee joint.
- A secondary cyst is a stretch of the synovial bursa located between the tendons of the gastrocnemius and semimembranosus muscles. The fluid enters through the channel through which the normal bursa is connected to the joint. This is the most common occurrence.
A cyst can vary in size from very small (asymptomatic) to large, but variation in size is very common. Especially in small cysts, there may be a septum separating the semimembranosus and gastrocnemius components. It can function as a valve, allowing fluid to enter the popliteal cyst and not leave it.
There are differences between popliteal cysts in children and adults. In children, these are cystic masses filled with gelatinous material that develop in the popliteal fossa. They are usually asymptomatic and are not associated with intra-articular pathology. Spontaneous resolution often occurs, although the process may take several years. In adults, Baker's cyst often occurs in combination with other intra-articular pathologies and inflammatory conditions.
Causes
The exact causes of these defects have not yet been established. There is a high probability that the tumor appears due to inflammatory processes in the joints or tendons. This condition occurs with various forms of arthritis, tears and injuries.
The risk group includes professional athletes and young people whose work involves constant excessive stress on the wrists or legs. Most often, salespeople, pianists, programmers or laundresses suffer from ganglion cysts.
With physical inactivity, the spinal cord of the cervical spine is often affected. It is also worth highlighting a genetic predisposition, so in most cases the lump appears in close relatives.
Symptoms
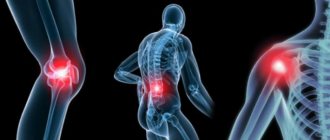
Baker's cyst is a dense, elastic, movable upon palpation and space-occupying formation in the popliteal region. Often it does not manifest itself in any way for many years. Its dimensions usually do not exceed 3 cm, as a result of which the pathology may not always be noticeable visually. The first symptoms are discomfort in the popliteal region; the onset of pain usually occurs after exercise. There may also be cramps, tingling, and numbness in the lower leg. With further growth, it can compress adjacent vessels (popliteal vein) and nerves, leading to disruption of blood flow and innervation of the leg, edema, and thrombosis of the veins of the lower extremity (one of the most dangerous complications). Complicated forms of this disease are cyst dissection or rupture, characterized by acute pain and requiring emergency treatment. That is why you should not underestimate this problem and delay treatment even in the absence of severe symptoms. Dealing with complications of the disease will take much more effort and time.
Clinical manifestations
The symptoms of the pathology depend on the diameter of the hygroma. Minor defects are asymptomatic, causing only aesthetic discomfort. As the pathogenic process progresses, the synovial bursa stretches excessively, causing severe pain.
Complications after removal of a dental cyst
Compliance with the rules and recommendations during the rehabilitation period after removal of a dental cyst helps prevent the development of a number of complications.
When small blood vessels or nerve fibers are compressed, the patient notices the following symptoms:
- Tingling or numbness of the skin.
- Neurological pain.
- Stagnation phenomena.
If the knee joint is affected, then walking and running cause discomfort. In advanced cases, venous outflow is disrupted, causing swelling of the affected area, blue discoloration of the epidermis, and limited mobility of the limb.
Clinically Relevant Anatomy
A Baker's cyst is an enlarged bursa located between the medial head of the gastrocnemius muscle and the capsular counterpart of the semimembranosus muscle, the oblique popliteal ligament.
For the formation of a cyst, two conditions must be met - anatomical connection and chronic joint effusion. Joint effusion in the knee can fill the gastrocnemius and semimembranosus bursae with synovial fluid and, if fluid drainage is obstructed by a unidirectional mechanism, the gastrocnemius and semimembranosus bursa enlarges, creating a pseudocystic cavity called a Baker's cyst.
Diagnostics
If you suspect a ganglion cyst, you should visit a traumatologist. The doctor must examine the patient’s complaints, conduct an external examination and palpate the defect.
To confirm the diagnosis, radiography, ultrasound, computed tomography or magnetic resonance imaging are performed.
To clarify the type of pathology, it is necessary to do a puncture with a biopsy for subsequent histological examination. If more severe diseases are excluded, and laboratory testing of the biological material taken does not reveal a pathological increase in bacteria, then a diagnosis of “ganglionic cyst” is made.
Treatment
The treatment option is selected based on the size of the tumor. Small cysts cannot be removed surgically. Moreover, such bumps tend to resolve on their own, so conservative treatment is often sufficient to achieve the desired effect.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
For this, various physiotherapeutic procedures are used in the form of electrophoresis and warming manipulations. However, after such therapy, the ganglion cyst often returns.
They also resort to professional massage. This procedure helps to normalize the outflow of synovial fluid from the capsule into the joint space.
Often a puncture is performed when the lump is punctured and the liquid contents are pumped out. After this, a sclerosing drug is administered, which glues the walls of the cyst and protects against relapse.
However, most often they resort to standard surgical intervention. Surgical excision is performed in cases of constant pain, limited joint mobility, and a rapid increase in formation.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
To speed up healing, after removal, the affected area should be immobilized for several days. Most often, the sutures are removed a week after resection of the ganglion cyst.
If after the operation swelling, hyperemia appears, pus or ichor leaks out, then the likelihood of divergence of the incision boundaries increases due to the cutting of the skin with sutures.
In this situation, it is necessary to perform another surgical procedure to eliminate dead tissue structures and eliminate the source of the inflammatory process. After a few weeks, performance is restored.
What are the consequences of the disease?
If the hernia is not treated, it leads to thinning of the popliteal bursa, where the synovial fluid is collected. As a result, the capsule may rupture, and all the fluid begins to spread throughout the calf muscle. This complication is accompanied by severe swelling of the lower leg, redness of the popliteal cavity, increased temperature and the occurrence of acute pain in the joints.
Another rather dangerous complication is when the capsule does not rupture, but rapidly increases in size and begins to put pressure on the walls of blood vessels. This leads to their inflammation and the appearance of thrombophlebitis, varicose veins and thrombosis. It is worth noting that thrombosis is a fatal disease. A blood clot that breaks off can cause a stroke or block a pulmonary artery.
Forecast
If you promptly seek help from a specialist and promptly remove the lump, then the prognosis for such a ganglion cyst is favorable. In this case, after the rehabilitation period, it is possible to fully restore performance.
However, if left untreated, a ganglion cyst can grow to a large size. Significant neoplasms disrupt the functionality of the affected joint, limiting its motor properties.
In addition, such formations often compress nerve fibers and blood vessels, impairing the nutrition of the limb, causing severe pain and congestion. Such defects require immediate surgical excision.
Self-opening or accidental damage to the cavity allows serous contents to leak out. This process is dangerous due to the development of an inflammatory process.
If an infection gets into the wound, suppuration begins, which can cause blood poisoning. Therefore, here the prognosis is no longer so favorable and everything depends on the time of assistance.
Possible complications if Baker's cyst is left untreated
Uncontrolled development of a popliteal Baker's cyst can cause a large number of complications, the most likely of which are:
- development of an infectious disease;
- rupture of the cyst membrane;
- forceful effect on the neurovascular bundle, leading to thrombophlebitis.
In rare cases, untreated Baker's cyst under the knee can cause compression of the popliteal vein or even an artery. If a complication of this type is detected, urgent hospitalization and surgical intervention are indicated.
Prevention
All prevention of ganglion cysts comes down to avoiding damage to joints and tendons. This is especially true for people whose activities involve constant monotonous movements.
Athletes, pianists, salespeople, and hairdressers should rest regularly so that their joints are not overloaded. In addition, it is important to treat bursitis and other inflammatory pathologies in a timely manner to prevent the disease from becoming chronic.
A ganglion cyst often occurs near a joint or tendon. The wrist is most often affected.
A benign neoplasm does not threaten the patient’s health and does not degenerate into a cancerous tumor, but it can cause severe discomfort, therefore, if a strange lump appears on the body, you should immediately visit a traumatologist.
Links[edit]
- "National Library of Medicine - Medical Subject Headings (MeSH) - Ganglion Cyst". Archived from the original on March 10, 2016. Retrieved August 27, 2013.
- ^ a b
"E-hand.com Electronic textbook on hand surgery". American Society for Surgery of the Hand assh.com. Archived from the original on March 9, 2014. Retrieved April 12, 2014. - ^ a b c d e f g h i j k l m
"Ganglion cyst of the wrist and hand - OrthoInfo".
orthoinfo.aaos.org
. March 2013. Archived from the original on July 6, 2021. Retrieved June 10, 2017. - ^ B s d e g h i J k
Ferry , Fred F. (2014).
Ferri's Clinical Advisor e-book, 2015: 5 books in 1
. Elsevier Health Sciences. item 472. ISBN. 9780323084307. Archived from the original on September 10, 2021. - ^ a b
Cooney, William P. (2011).
Wrist: diagnosis and surgical treatment
. Lippincott Williams and Wilkins. item 1089. ISBN 9781451148268. Archived from the original on September 10, 2021. - ^ a b c d e
Craig A. Camasta, DPM (1993). "Excision of a ganglion cyst" (PDF). Institute of Podiatry. Archived (PDF) from the original on 11/01/2013. - Stretanski, Michael F. (2020-01-01), Frontera, Walter R.; Silver, Julie K.; Rizzo, Thomas D. (ed.), "Chapter 32 - Ganglia of the Hand and Wrist", Essentials of Physical Medicine and Rehabilitation (Fourth Edition)
, Philadelphia: Content Repository Only!, pp. 169–173, ISBN 978-0-323- 54947-9, received 2020-10-24 - Fess, Elaine Ewing; Gettle, Karan S.; Philips, Cynthia A.; Janson, J. Robin, eds. (2005-01-01), "Chapter 17 - Splinting for Work, Sports and the Performing Arts", Hand and Upper Extremity Splinting (Third Edition)
, St. Louis: Mosby, pp. 456-479,. Doi: 10.1016/b978-080167522-5.50022-8, ISBN 978-0-8016-7522-5, received 2020-10-24 - ^ a b c d e f g h
Buddy, Julie;
Wollman, Jackie (01/01/2014), Cooper, Cynthia (ed.), "36 - Ganglia and Tumors of the Hand and Wrist", Essentials of Hand Therapy (Second Edition)
, St. Louis: Mosby, pp. 500 -507, DOI: 10.1016 /b978-0-323-09104-6.00036-5, ISBN 978-0-323-09104-6, received 2020-10-24 - ^ a b
McNabb, J. W. (2005).
A practical guide to joint and soft tissue injection and suction
. Lippincott Williams and Wilkins. pp. 62–65. ISBN 9780781753630. - "Ganglion cysts". British Society for Surgery of the Hand
. BSS. Archived from the original on April 7, 2021. Retrieved April 6, 2017. - Kirk Watson, H.; Sorel, Jonathan (01/01/2010), Slutsky, David J. (Editor), "CHAPTER 45 - Dorsal Carpal Syndrome and Rotational Subluxation of the Scaphoid", Principles and Practice of Wrist Surgery
, Philadelphia: W. B. Saunders, pp. 487– 491, ISBN 978-1-4160-5646-1, received 2020-10-24 - ^ a b c d
Cooper, Cynthia (01/01/2007), Cooper, Cynthia (ed.), "Chapter 21 - Ganglion Cysts and Other Common Tumors of the Hand and Wrist",
Fundamentals of Hand Therapy
, St. Louis: Mosby., pp. 412-420, DOI: 10.1016/b0-32-303386-5/50024-2, ISBN 978-0-323-03386-2, received 2020-10-24 - Duncan J. M. Macdonald; and others. (August 2007). "Differential diagnosis of foot tumors: 101 surgical cases in North Glasgow over 4 years". Annals of the Royal College of Surgeons of England
.
89
(3):272–275. DOI: 10.1308/003588407×168235. PMC 1964714. PMID 17394713. - John Arthur Jacobson (2007). Fundamentals of Musculoskeletal Ultrasound
. Elsevier Health Sciences. ISBN 978-1416035930. Archived from the original on July 4, 2014. - Rent CF. Ultrasound of the shoulder. Master Medical Books, 2013. Sample chapter on the acromioclavicular joint ganglion available. Archived May 18, 2014, at the Wayback Machine.
- Muir B, Kisel JA, Yedon DF (December 2011). "Intraosseous ganglion cyst of the humeral head in a competitive flatwater rower: a case report". J Can Chiropr Assoc
.
55
(4):294–301. PMC 3222705. PMID 22131566. (including MRI images) - Jae Jeong Park; and others. (2010). "Case Report: Intramuscular ganglion cyst of the Gastrocnemius muscle". Korean Journal of Dermatology
. Archived June 17, 2013. - Park S, Jin W, Chun YS, Park SY, Kim HC, Kim GY, Park JS, Ryu KN (October 2009). "Ruptured intramuscular ganglion cyst in the medial gastrocnemius muscle: sonographic appearance." Journal of Clinical Ultrasound
.
37
(8):478–81. DOI: 10.1002/jcu.20609. PMID 19618443. S2CID 20586520. - Robert J. Spinner; and others. (2012). "Re: Pure peroneal intraneural ganglion cyst: 20/20 hindsight" (PDF). Turkish neurosurgery. pp. 527–528. Archived (PDF) from the original on 2013-10-14.
- ^ a b
Sang Woo Kim;
and others. (April 2011). "Ganglion cyst in the second lumbar intervertebral foramen". J Korean Neurosurg Soc
.
49
(4): 237–240. DOI: 10.3340/jkns.2011.49.4.237. PMC 3098430. PMID 21607185. (original source cites eight additional references per paragraph cited) - RJ Spinner; and others. (2012-08-29). "Evidence that adventitial cysts, similar to intraneural ganglion cysts, are also connected by joints." Clin. Anat
.
26
(2): 267–81. DOI: 10.1002/ca.22152. PMID 22933403. S2CID 37986961. - Field, Larry D. (2003). MasterCases: Shoulder and Elbow Surgery
. Time. item 241. ISBN. 9780865778733. - Jump up
↑ Ribes, Ramón (2010).
Musculoskeletal Imaging Study
. Springer. p. 197. ISBN 9783540880004. - ^ B Pocket guide to the diagnosis of the musculoskeletal system
. Springer. 2005. p. 63. ISBN 9781597450096. - ^ a b c Gale's Encyclopedia of Surgery: A Guide for Patients and Caregivers, Volume 1
. Gail. 2003. P. 560. ISBN 9780787677213. - ^ a b
"Clinical Treatments for Carpal Ganglia" (PDF).
ROYAL AUSTRALASIAN COLLEGE OF SURGEONS
. Archived from the original (PDF) on March 27, 2021. - Bismil MSK, Bismil QMK. Wide Awake Approach to the Hand and Wrist Ganglia: Ten Years of Experience, Technical Advice, and Review of Gross Pathology and Outcomes in 300 Cases. OA Case Reports 2013, November 15; 2 (13): 129.
- Dacombe, P.J.; Robinson, J (27 March 2012). "Falling down the stairs: the 'Bible Hit' equivalent for knee ACL ganglion cyst". BMJ Case Reports
.
2012
: bcr0120125591. DOI: 10.1136/bcr.01.2012.5591. PMC 3316796. PMID 22605799. - Hammond, Claudia. "Should you hit the" biblical bump "?" . Retrieved August 9, 2021.
- Camasta, Craig A., DPM, Hygroma Excision
Archived 2013-11-01 at the Wayback Machine, podiatryinstitute.com, updated 1993, 1993 33 PDF, pp 181-5 - Gallego S, Mathoulin C (2010). "Arthroscopic resection of dorsal wrist ganglia: 114 cases with a minimum follow-up of 2 years." Arthroscopy
.
26
(12): 1675–1682. DOI: 10.1016/j.arthro.2010.05.008. PMID 20952152. - Lidder S, Ranawat W, Arens R (2009). “Surgical removal of wrist ganglia; a review of the literature and a nine-year retrospective study of relapse and patient satisfaction." Orthop Ed
.
1
(1): e5. DOI: 10.4081/or.2009.e5. PMC 3143961. PMID 21808669. - Dias JJ, Dhukaram V, Kumar P (October 2007). "Natural history of untreated dorsal carpal ganglia and patient reported outcome 6 years after intervention." Journal of Hand Surgery, European Volume
.
32
(5):502–8. DOI: 10.1016/J.JHSE.2007.05.007. PMID 17950209. S2CID 21853864. - Dias J, Buch K (April 2003). “Palmar carpal ganglion: does intervention improve outcome? A prospective study of the natural history of the disease and patient-reported treatment outcomes.” J Hand Surg Br Vol
.
28
(2): 172–6. DOI: 10.1016/s0266-7681(02)00365-0. PMID 12631492. S2CID 44865301. - J. C. Segen (1992). Dictionary of Modern Medicine
. ISBN 9781850703211. Archived from the original on September 10, 2021. (see entry on aneurysmal bone cyst, which "like pyogenic granuloma and ganglion cyst, a misnomer that has withstood the sands of time and a hint of logic") - "Etymology of the Greek word ganglion (γάγγλιον)". Archived 10/06/2013.
- See Hippocrates' "On the Joints" (Part 40) on Wikisource.
- "Ganglia". Archived from the original on April 15, 2009. Retrieved May 27, 2009.
- Hammond, Claudia. "Should you hit the" biblical bump "?" . Retrieved November 24, 2021.