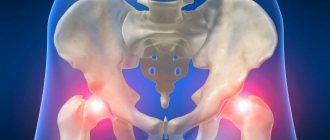
Thomas Test - Hip Flexor Assessment The Thomas Test, also known as the iliopsoas test, is used to evaluate the elasticity of the hip flexors, which include the rectus femoris, pectineus, gracilis, tensor fasciae lata, and sartorius muscles. Restricted range of motion in the hip joint can lead to low back pain, hip osteoarthritis, and patellofemoral pain syndrome.
Thigh scarecrow
Too often we have to explain to patients that their pain, dysfunction, or poor performance in whatever movement they perform is caused by the great hip bugbear—tight hip flexors. The origin of this idea is unknown, but may have originated with the theory of the lower cross syndrome. She states that when the hip flexors and psoas muscles are tight and the gluteal and abdominal muscles are relaxed, the pelvis tilts forward, which leads to dysfunction. In fact, this theory perceives the body as a puppet, in which the position of the pelvis depends on which strings we pull or which muscles we strain.
Why are they tense?
Most experts, including those sincerely respected by Lehman, are convinced that the hip flexors are tight due to a sedentary lifestyle - a sign of our age. If we sit at a desk for 8 hours a day, our hips will be constantly flexed, and our hip flexors will be tense, contracted, and then difficult to stretch. Despite the attractiveness of this theory, Lehman refuses to believe in it. He has been dealing with this theory for 15 years and is convinced that its conclusions are not based on anything.
Can prolonged sitting tighten and shorten the hip flexors? No way. And that's why.
- Even if you sit for 8 hours a day without a break, this is not enough for the muscles to become shorter. Shortening occurs when you are in a cast for a really long time, not hours, but days and weeks, and your muscles are shortened and immobile. A sitting person stands up during the day, interrupting this muscle shortening.
- Even if those 8 hours are so terrible, you nullify their effect when you sleep for 8 hours with your legs extended or do something standing. On the other hand, why don't we shorten our thigh muscles if we sleep with our legs bent in the fetal position? Has anyone told their patients that it is harmful to sleep on your side with your knees bent? What about embryos that spend 9 months in a curled up state? Maybe they also have difficulty straightening their legs?
- The way we sit is often contrasted with other cultures that sit differently. In some countries, it is customary to sit in a deep squat, that is, squatting. I wonder how their hip flexors are? Do these people realize the danger of redundancy they are exposed to? Perhaps they should be warned.
Patient examination
History taking
When collecting anamnesis, it is important to conduct a thorough interview with the patient, pay attention to the “red flags” and identify exactly how the symptoms of the disease affected the person’s performance. The following questions will help determine whether a patient has pelvic dysfunction.
- How often do you pee? (normally – every 2-4 hours, or 6-8 times a day).
- Have you experienced urine leakage when coughing, sneezing, laughing, or exercising?
- Has urine leaked during a sudden strong urge to urinate?
- Have you ever been unable to go to the toilet on time?
- Have you ever found yourself in situations where you couldn't control your bowels?
The best place to start assessing pain is by completing the Oswestry Low Back Pain Disability Index questionnaire. The choice of treatment strategy will depend on the number of points scored.
Physical examination
- Posture assessment.
- Palpation.
- Neurological examination.
- Range of active movements in the lower back and hip joints.
- Assessment of joint mobility of the lumbar spine.
- Make sure that the cause of the pain does not lie in the hip joint. To do this, perform a hip quadrant test (hip flexion with abduction and adduction) and a FABER test (flexion, abduction and external rotation). The cross-sectional study by Dufour et al supports previous research suggesting that the FABER test can be used to identify pelvic floor weakness, which in turn is one of the parameters of low back pain.
- Assessment of the sacroiliac joints (Gaenslen test).
The majority of patients with low back pain and pelvic floor incompetence will likely require core stabilization exercises. The decision to perform a full pelvic floor examination depends on the patient's initial complaints.
A complete pelvic floor examination includes:
- Vaginal palpation is a qualitative assessment of the correctness of muscle contraction. Digital examination allows us to better understand the relationship between lumbopelvic pain and the condition of MTD. Most often, manual examination reveals their soreness, followed by weakness.
- Transabdominal ultrasound to assess the quality of voluntary and involuntary activation of the MTD and transverse abdominis muscles.
- Assessment of MTD force should be performed using a perineometer and/or an electromyograph (EMG) needle to obtain quantitative data on muscle contractions.
The Tight Hip Flexor Theory Has Implications
If you subscribe to the tight hip flexor theory, then your ideas about muscle function and movement must be formed in a certain way.
Incorrect application of the law of mutual inhibition
Many therapists refer to Sherrington's law of reciprocal (conjugate) muscle innervation, or the law of reciprocal suppression. According to him, muscle contraction is accompanied by relaxation of its antagonists. Therefore, tight and shortened hip flexors should suppress gluteus maximus activity. However, we cannot agree with this for two reasons.
A). Reciprocal innervation requires that the signal that contracts a muscle be associated with the relaxation of its antagonist. The assumption that shortening of the hip flexors is caused by prolonged sitting implies that it is a passive process not associated with tonic contraction of the flexor muscles. If there is no nerve impulse that contracts the muscle, there is no associated innervation.
B). Even if a nerve impulse is sent to the muscle, it may not be sufficient to noticeably suppress the antagonist. This mechanism differs from the mechanism of mutual innervation. An overview of the article devoted to this problem and its full text can be read here. Reflex inhibition when walking usually occurs at the reflex level, and not at the volitional level. Greg Lehman isn't even sure if anyone has specifically tested the strength of a "suppressed" muscle, because as soon as we try to do this, the antagonist immediately turns into an agonist. In addition, muscle contraction occurs during many activities. We contract muscles (such as the hamstrings and quadriceps) to provide joint stability and control movement. If mutual inhibition worked with tight or overactive hip flexors, it would be difficult to achieve joint stability during co-contraction. According to Lehman, there is little evidence that reciprocal innervation causes weakness. If someone thinks differently, he is ready to listen to counter-arguments. Lehman cites two articles, one on the effects of stretching on reciprocal inhibition and the other on neuromuscular adaptations to stretching, that support his point.
Tight hip flexors need relaxation
Greg Lehman himself has had his hip flexors pulled several times. This procedure literally penetrated to the intestines: both the intestines and the omentum were compressed, the abdominal muscles contracted, but the lumbar muscles, at least the deep ones, did not relax. And how could 3 minutes of lower back relaxation affect the consequences of many years of sitting for 8 hours a day? Mechanically? Through a neural mechanism? Nobody believes this. One can imagine the consequences of trying to stretch the psoas muscle by considering the limits of stretching as long-term muscle stiffness and, therefore, resting length changes. A short post about stretching and muscles here.
Believing in tight hip muscles can lead to hyperextension
Anyone who believes in the theory of lower cross syndrome will look for and find this syndrome, and having found it, will want to correct it, that is, stretch the hip flexors. However, stretching them can be harmful to both athletes and patients. This is like forcefully twisting your shoulder, abducting and supinating it. What happens in this case to the anterior capsule? Is it an adaptation or a stress that you want to subject everyone to?
Why do you want to extend your hips? How necessary is this?
We only need 10-15 degrees for walking and about the same for running. Consequently, the importance of hip stretching is overrated. You don't even use your glutes to stretch your hip when you walk or run. By the time your foot is behind you touching the ground and begins to move out of neutral, your glutes have already switched off. This is the extensor paradox.
Clinical Implications Warning: Hip extension during running is associated with anterior pelvic tilt.
Some experts believe that limited hip extension when running increases lumbar lordosis and can cause injury. Lehman has something to object to.
- No one has actually tested whether this situation leads to injury and reduces performance. These are just assumptions.
- Tests to assess the elasticity of the hip flexors (the Thomas test, for example) do not correlate with quantitative indicators of extension during running. This means that you are not required to fully extend your hip while running. This causes the pelvis to tilt forward, not because the hip flexors are tight. The degree of hip extension does not correlate with the degree of flexion. This is a perfect example of how the results of quasi-static and dynamic tests are not always the same. Hip flexion may be limited by movement rather than physical limitations identified during the Thomas test.
- The pelvis tilts forward not because tense muscles are pulling it into a new position. Rather, the tilt occurs because the hip must move backward, and this can be done in two ways: by extending the hips or by tilting the pelvis. Some people prefer to tilt their pelvis more, so they don't need to extend their hip.
Clinical picture
Experience has shown that a patient with low back pain as well as MTD failure will have the following characteristics:
- Middle-aged or older women.
- A history of natural childbirth (and the number of births proportionally increases the likelihood of problems with the pelvic floor).
- Obesity.
- Lumbar-pelvic pain.
- Urinary or fecal incontinence.
- Chronic constipation.
- Chronic pelvic pain.
- Dyspareunia (pain before, during and after sexual intercourse).
Many women with pelvic neuromuscular dysfunction experience posterior pelvic tilt and flattened lumbar lordosis. Some studies suggest that pain in the sacroiliac region may impair motor control of MTD.
Men can also experience pelvic floor incompetence, but due to purely anatomical features, such cases are much less common. The male pelvis is much more “densely packed”, which ensures the “flowing” of muscle excitation (irradiation phenomenon) and rapid recruitment of muscle fibers.
Final Thoughts
- According to Lehman, the diagnosis of shortened hip flexors is overused. The Thomas test may give false positive results. Lehman himself often tests patients by simply placing them on a couch and stretching their leg into extension. Loss of movement is extremely rare.
- Lehman doesn't think sitting for eight hours will shorten the hip flexors.
- The feeling of hip flexor tightness can be subjective.
- Stiffness in movement does not necessarily have mechanical causes. We also have a nervous system, and restriction of movement may be associated with a perceived threat or defensive behavior.
- However, all methods used to treat the nonexistent "lower cross syndrome" may be helpful for pain or dysfunction. You shouldn’t throw out the baby with the dirty water of non-existent diagnoses, i.e. useful exercises.
Greg Lehman self-critically notes that he is not the first to write on this topic. There are other posts, shorter ones.
Treatment
Pharmacotherapy is mainly aimed at the problem of urinary incontinence rather than muscle failure. The purpose of the drugs is to increase urethral closure pressure by acting on the smooth and striated muscles of the urethra. Some patients may use painkillers or corticosteroid injections to relieve symptoms. However, these medications will not solve the main problem with MTD failure and pain in the lower back.
Friends, Marina Osokina’s seminar “Women’s health: opportunities for restorative fitness and physical therapy” will take place very soon. Find out more...
Surgery
Surgery is indicated for those patients with MTD weakness and low back pain who have not responded to conservative methods (eg, physical therapy) and who have symptoms that significantly affect their quality of life.
To solve the problem associated with pelvic dysfunction, the following operations are performed:
- Pubovaginal sling operations.
- Implantation of an artificial bladder sphincter.
- Midurethral sling.
Physical therapy
Physical therapy methods include MTD training, manual therapy, biofeedback training (boss therapy), motor training, and behavioral psychotherapy. Manual therapy and barefoot therapy are used to help the patient become more aware of this area of her body and improve her ability to contract and relax the muscles in addition to strengthening them.
Controlling MTD is the key to preventing urinary incontinence and a way to reduce pelvic pain. Pelvic organ dysfunction can be treated by strengthening the pelvic floor and improving control of the area. MTD training combined with bore therapy can achieve greater results than MTD training alone. In addition, according to a number of studies, the effect may also be stronger if electrical stimulation is added to these techniques.
A study by Xia B et al shows that conventional treatment is less effective than the same treatment, but in combination with pelvic floor exercises: in the second case, there is a decrease in pain and improved ability to work. Facilitation of MTD can be achieved through co-activation of the abdominals and vice versa. The abdominal muscles contract in response to contractions of the MTD, and the pelvic floor muscles contract in response to the command of the abdominal muscles to “shrink or relax.”
A randomized controlled trial of 20 women with chronic low back pain found that physical therapy combined with MTD training had a greater positive effect on muscle strength and endurance. In addition, this approach significantly reduced pain and functional disability. However, no significant difference was found between the control and experimental groups. It can be assumed that MTD training in combination with usual treatment was not superior to usual treatment only in patients with chronic low back pain.
Current evidence confirms the effectiveness of the previous exercise protocol. The goal of each training protocol is to restore functional neuromuscular control of the pelvic floor and deep abdominal muscles. There is also strong evidence that MTD training may be a conservative treatment for stress urinary incontinence.
Sequence of exercises for low back pain and pelvic floor dysfunction
Lumbar stabilization exercises
Treatment for such a patient should also include counseling on healthy lifestyle choices. New healthy habits may include maintaining good posture, controlling weight, eating an appropriate diet, exercising regularly and not smoking.