If your car breaks down, you take it to a service center, if your pipes are leaking, you call a plumber, and if you have a broken bone, you visit a surgeon. But unlike other things, bones begin to repair themselves. The human body has amazing healing powers that allow it to cope with a number of diseases. Of course, doctors play a vital role in the healing process, but in most cases they simply help the body heal itself. Doctors provide optimal conditions for bone healing, and the rest is up to your cells. But how exactly do bones recover after a fracture? To answer this question, we must study in more detail what bones are made of.
At first glance, the bone looks like an inanimate, immobilized part of our musculoskeletal system. But our entire skeleton is as alive as any part of the body. The body stores minerals in the tough part of the bone. The inner red bone marrow produces red blood cells, and the yellow bone marrow produces fats. It is important to remember that bones are constantly changing. Old bone tissue is replaced with new bone, a process called bone remodeling. Bone tissue consists of osteoclasts, osteoblasts and chondroblasts. The latter are responsible for the formation of cartilage, and all of them together form all bone tissue.
General information
A callus is a multilayer structure formed during the regeneration of bone tissue, which is caused by a violation of the integrity of the bone (as a result of mechanical trauma or other external or internal influences) during the normal course of healing of fractures.
As a result, connective (provisional callus) or cartilaginous tissue is formed to replace other heterogeneous structures at the fracture site, which then undergoes metaplasia to form the final callus. Bone callus is a unique pathological and anatomical substrate for bone regeneration.
Most typical for tubular bones. Histologically, it is a formation with all the specific elements and structures of bone tissue, but more calcified and phosphorylated.
Prevention: how to avoid the appearance of a growth after plastic surgery?
In the postoperative period, it is necessary to create optimal conditions for the formation of normal callus. To do this, you must follow all the instructions given by the surgeon:
- do not blow your nose for two weeks;
- sneeze with your mouth open;
- do not wear glasses and exclude any other mechanical impacts and damage to the operated area;
- monitor the correct position of the plaster splint, do not displace it or remove it prematurely;
- do not start playing sports until your doctor allows it;
- at the first symptoms of bone hypergrowth, consult a doctor;
- immediately after plastic surgery, observe bed rest for three days;
- Do not stay in the sun for a long time and do not go to the solarium.
Pathogenesis
of connective tissue occurs . After about a week, osteoid tissue begins to form, undergoing transformation either into bone itself, or initially into cartilage, and later into bone. This is usually caused by the mobility of bone fragments, which leads to trauma and disruption of the microcirculation of the resulting regenerate. The formation of initially cartilage tissue is due to the fact that this process requires less oxygenation and fewer biologically active compounds.
The formation of periosteal callus occurs as a result of processes in the bone-forming cells of the periosteum (periosteum) and endosteum. These mechanisms play a critical role in the process of healing of injured bone. The periosteum plays a fundamental role in the fusion process, from which the periosteal callus is formed.
Stages of callus formation
The formation of callus during a fracture is a complex regeneration process that occurs in several stages, although there may be variations in different locations; let’s look at the example of ribs:
- The formation of a primary connective tissue callus takes approximately 10-14 days - first, blood accumulates at the fracture site and a hematoma , hyperemia and serous impregnation are formed, initiating the influx of leukocytes that cause swelling, as well as fibroblasts - cells capable of producing connective tissue structures, against the background of which the the process of alteration - osteoclastosis, designed with the help of osteoclasts to destroy necrotic and damaged cells of the bone and adjacent soft tissues, while the process of formation of vessels (granulating tissue) occurs.
- The formation of young mesenchial tissue plays a critical role in filling bone defects and hematomas; hyaline or fibrocartilage grows between and around fragments.
- The formation of osteoid callus - the process of transformation of connective tissue into osteoid within 3-4 months is caused by decalcification - processes of deposition of inorganic compounds present in normal bone, sometimes it is mistakenly mistaken for a “cartilaginous callus” and it resembles a soft (primary) callus, forming approximately after 5 weeks, during which time reverse processes occur at the fracture site - reduction of blood vessels, elimination of edema and normalization of blood flow against the background of disappearance of signs of inflammation.
- The bone callus itself is a neoplasm enriched with apatites (hydroxyapatites) in the form of a conglomeration of amorphous osteoid tissue turning into bone, which is first distinguished by a loose structure, and then, decreasing in size, acquires the features of normal architectonics in the phase of reverse development of bone tissue structures (formation of trabeculae, restoration of the bone marrow canal), the process can last for years.
Callus does not form when bone fragments are tightly juxtaposed, when the size of the gap is fixed to 500 microns, there is good blood supply, there is no periosteum, as well as in fractures of the flat bones of the skull, sternum, pelvis and scapula, since fusion occurs due to connective tissue due to the peculiarities bone embryogenesis.
In the layers of skeletogenic cells of the periosteum and endosteum, bone beams can immediately, initially form, bypassing the fibrocartilaginous stage of bone formation, so the callus can be small in size or not expressed at all.
Layers of callus
Callus can have a different layered structure depending on the tissue source of its formation and usually differs in:
- periosteal layer;
- endosteal layer;
- intermediary layer or otherwise called intermediate, which can develop from elements of the Haversian canals and occupies the space between the endo and periosteal layers;
- the final - paraosseous layer covers from the outside all of the above layers, the source of its formation is the surrounding soft tissue;
- At the base of the entire layered structure is osteoid tissue.
By difficulty:
Simple (isolated) – not accompanied by other damage.
Combined (fracture + non-mechanical damage - burn, frostbite).
Combined (trauma of the musculoskeletal system + damage to organs of other systems - brain, abdominal organs).
Multiple – fractures of bones of various segments of the musculoskeletal system (for example: shoulder, pelvis and toes).
You should know and remember that there are no “simple” bone fractures, since any fracture is accompanied by damage to the soft tissue in the area of its location and is surrounded by a hematoma.
Classification
Depending on the functional characteristics, there are 4 types of callus, which develop on each bone fragment and form a common “coupling” of consolidation:
- periosteal (external) – characterized by the fastest rate of formation, necessary for fixation of bone fragments, formed by the periosteum;
- endosteal (internal) - like the external one, plays an adaptive function, is formed from the endosteum and is a temporary basis for future fusion and growth of bone regenerate, the first two types of callus ultimately undergo resorption;
- intermediary – formed at the junction of a compact layer of fragments and ensures true bone fusion;
- paraosseous - formed from connective tissue during the rapid development and proliferation of scar structures in cases of significant damage to surrounding tissues; such a callus subsequently undergoes transformation due to metaplasia into bone tissue, but can form a large protrusion on the bone.
Healing options
Normally, the process of fracture consolidation begins with the proliferation of periosteal and endosteal cells, which form bone calluses of the appropriate type, fix bone fragments and prevent their displacement. After this, an intermediary callus is formed, gradually acquiring the properties of normal bone. The periosteal and endosteal callus are reduced by this time, having fulfilled their functions. This option of fracture healing is the most optimal; it has a minimum duration and ensures complete restoration of the bone in the damaged area.
Healing is considered primary if an intermediary bone callus forms in the fracture area. A prerequisite for this is maximum comparison and immobilization of bone fragments. In the case where mobility between the fragments cannot be excluded and the germination of the vascular plexuses between them is difficult, then healing is secondary. In this case, the leading role belongs to the periosteum, which has an abundant blood supply and is actively involved in the regeneration of damaged tissues.
Causes
Diseases that contribute to the development of bone calluses, disruption or slowdown of the processes of true fusion:
- old age;
- endocrine pathologies, for example, hyperparathyroidism and diabetes;
- osteoporosis;
- obesity;
- pregnancy;
- radiation sickness;
- tuberculosis;
- syphilis;
- amyloidosis and chronic inflammatory diseases;
- general exhaustion;
- severe anemia ;
- hypoproteinemia;
- avitaminosis.
Symptoms
Signs of a fracture and secondary fusion with the formation of periosteal callus are:
- local pain that subsides;
- crepitus – a characteristic crunching sound, especially when trying to move a limb;
- disappearance of pathological mobility;
- distortion of the shape and structure of the bone during the formation of a paraosseous callus, which may look like a large protrusion.
Callus after a clavicle fracture
After a clavicle fracture, a natural process of formation, first of osteodin, then of callus, also occurs, which usually takes up to 2 months. The causes of fractures are most often falls, sports injuries, road accidents, and are also possible in newborns during birth.
Callus after a clavicle fracture
After the collarbone has completely fused, the callus should resolve, but in some cases this does not happen, as in the photo of the callus presented above.
Factors influencing the regeneration process
The process of bone recovery after a fracture is influenced by many factors.
These include:
- type and complexity of the fracture;
- location of damage;
- type of damaged bone;
- degree of blood supply;
- degree of displacement of fragments;
- patient's age;
- balanced diet;
- the degree of functional load on the damaged bone;
- degree of infection by pathogenic microorganisms;
- quality of fracture immobilization;
- speed of metabolic processes;
- the presence of somatic pathologies.
The presence or absence of damage to nearby structures, ligaments and muscles plays a big role.
Tests and diagnostics
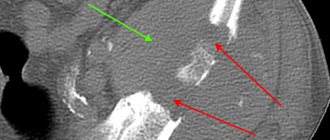
The main way to identify callus is x-ray examination. When collecting data, the patient’s complaints, medical history and the nature of the dysfunction of the limb are taken into account. In this case, it is necessary to trace the fracture line.
In severe diagnostic cases, radiographs are additionally repeated in various positions, as well as CT and MRI.
The speed and quality of callus formation become quite important for the prognostic picture. Osteodic calluses that form on the 10-20th day after a fracture are X-ray negative. Radiographically, callus becomes visible from about 4 weeks due to the fact that the tissue in it calcifies. Severe callus can be detected 3 months after injury.
Healing phases
Immediately after injury, under the influence of tissue breakdown products, the growth of mesenchymal tissue begins (the initial phase of regeneration). In the pathological focus, the so-called primary glue appears, which consists of fibrin threads, blood clots and tissue fluid.
In the second phase, its cellular elements undergo differentiation. Thus, mesenchymal tissue becomes osteogenic. At this stage, primitive bone beams are found in the callus, forming an abundant network (osteoid callus phase). Subsequently, calcification is observed. The callus matures and changes its structure: excess elements are absorbed and the bone beams approach the anatomical in shape and structure.
In women after rhinoplasty
There are known cases where in women, in approximately 12% of cases after rhinoplasty, callus and hyperplasia formed during the rehabilitation process. It does not pose a threat to health, but is a fairly noticeable and unattractive cosmetic defect. Externally, the organ of smell looks excessively large and has a hump, so patients have to turn to a plastic surgeon again. The size of the formation, due to circumstances, can vary significantly, as well as the time of its manifestation; most often the growth appears after a few weeks, but there have been cases when it appeared after a year. This is facilitated by the reactivity of the body, state of health, skill of the surgeon and the age of the patient. By the way, persons under 18 years of age are not recommended to carry out such manipulations, since due to active processes of bone formation there is a high risk of developing calluses.
Callus after rhinoplasty
The cause of callus after rhinoplasty is the improper fusion of connective tissue damaged during surgery to correct the nose as a complex anatomical structure that does not have much strength. The main symptoms of callus formation in the nose are:
- changing the shape of the nose;
- pain;
- swelling and a pronounced hump.
Surgical approaches to treat lumps:
, corrective osteotomies are used at SM-Clinic
. These operations allow you to get rid of deformity and preserve the joint. It is not enough to cut down the “bump”; it is necessary to eliminate the deformation of the first metatarsal bone and fix the fragments with special screw-clamps.
Patients begin to walk independently the next day after surgery wearing special postoperative shoes - Baruk shoes. After the operation, the patient spends no more than 2 days in the hospital. During this time, adequate pain relief, antibiotic therapy, dressings, physical therapy, and physiotherapy are carried out.
If you feel pain in your big toes, contact the SM-Clinic on the street. Clara Zetkin for modern surgical treatment!
Zhuravlev Kirill Andreevich traumatologist-orthopedist “SM-Clinic” on the street. Senezhskaya
You can find out more details, make an appointment with a specialist or call a doctor at home by phone
Diet for callus
Diet for fractures
- Efficacy: therapeutic effect after a month
- Timeframe: 2 months
- Cost of food: 1600-1800 rubles per week
The diet after a fracture and during the formation of callus should be complete and balanced. It is extremely important that every day your body receives:
- a sufficient amount of proteins, the source of which should be veal, poultry, rabbit, legumes, cottage cheese and cheeses, as well as bone decoctions;
- mineral compounds essential for osteogenesis are found in fish, seafood, eggs, dairy products and yoghurts such as “Rastishki”;
- antioxidants and vitamins - can be taken in the form of additional complexes, but it is better to enrich the diet with fruits, berries, vegetables and herbs, drink green tea with ginger, smoothies and fruit drinks;
- healthy fats - we must not forget about their benefits, so unrefined oil, nuts, seeds and seeds should be added to vegetables and other dishes;
- carbohydrates - porridge and whole grain baked goods - are essential components of a complete diet.
Stages of flat feet
The orthopedist determines the severity of the foot deformation based on the condition of the arches, range of motion, impression of the sole, and x-ray. For an objective assessment, computer podometry (diagnosis of the load on the foot) is prescribed.
There are four degrees in total, which are characterized by the following:
- Slight fatigue of the legs, swelling, the big toe is not displaced, redness is noticeable on the side joint.
- Distinct pain towards the end of the day, the thumb deviates up to 20 degrees.
- The angle of inclination increases to 30°, the range of movement is limited, and there is no transverse arch. The pain spreads to the knees.
- The thumb deviates more than 40° and may become curled. The swelling does not subside, my legs, lower back, and head hurt. It is difficult to walk in ordinary shoes.