During the pathological functional restructuring of bone tissue, Z.S. Mironova et al. (1980) distinguish four stages, reflecting the increase in pathological changes in bone substance, compensatory phenomena and dysfunction of the affected segment.
Stage I (periostosis) - thickening of the cortical bone, unevenness of this thickening in the pathological zone, development of dystrophic and degenerative changes in the periosteum.
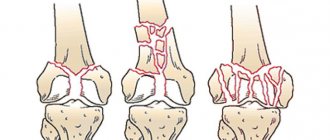
Clinically - complaints of pain in the corresponding bones after exercise, which disappear after a short rest. Stage II (formation of zones of linear or lacunar restructuring) is characterized by pain that does not go away after rest and intensifies after physical activity. There is swelling, hyperemia of the skin, local pain, unevenness of the bone upon palpation; X-ray - linear zones of clearing in the cortex or zones of lacunar restructuring in the cancellous bones in the form of racemose clearings; pathomorphologically - areas of osteocytic bone, deep dystrophic and degenerative changes with a sharp disruption of reparative processes. Stage III (pathological fracture) is characterized by sharp pain in the affected bone; X-ray - sclerotic changes in the edges of the fracture, irregularities in the fracture line or the formation of a carpal cavity in the center of the fracture. In stage IV (consequences of restructuring), moderate constant pain is noted during exercise; X-ray - violation of the shape of the articular end, deforming arthrosis.
Stress fractures of the sesamoid bone of the first toe. Its pathological restructuring is quite common, but its incorrect diagnosis makes the fractures observed with it rare. The difficulty of diagnosing stress fractures of this bone is explained by its lobular structure, which, as is known, is characteristic of some other sesamoid bones. There is an opinion that the sesamoid bone acquires a lobulated structure solely as a result of the development of the restructuring process in it.
Clinically, stress fractures of the sesamoid bone of the first toe are characterized by pain in the area of the first metatarsophalangeal joint, aggravated by running, rolling the foot, pushing off the forefoot, and while supporting the big toe. Many doctors and patients tend to explain this by injury to the first finger, bruising it against a stationary object. Radiographs during the initial examination, as a rule, are uninformative, and the lobulated structure of the sesamoid bone is usually interpreted as an anatomical norm. Only dynamic X-ray observation of the patient using non-standard projections sometimes makes it possible to detect a cloud of callus between the fragments, which confirms the correct diagnosis of the fracture.
One of the symptoms of pathological restructuring of the sesamoid bone is its increase in size, the appearance of resorption zones, as well as local ossification.
Here is an observation.
Patient F., 19 years old, a ballet dancer, for 9 months noted severe pain in the area of the first metatarsophalangeal joint, which intensified while jumping on stage. Stopping rehearsals for 2-3 weeks led to a decrease in pain. Physiotherapeutic procedures brought temporary relief. Based on a clinical and radiological examination, the CITO established a diagnosis of a fracture of the external sesamoid bone. No signs of callus were found. A plaster bandage of the “boot” type was applied for a period of 4 weeks; after removing the bandage, rehabilitation and sanatorium treatment was carried out. She was examined after 6 months, the fracture had healed, the patient began gradual exercise, and then began to dance without restrictions.
It should be remembered that removal of the sesamoid bone in ballet dancers can lead to instability at the first metatarsophalangeal joint, as this bone plays a significant role in increasing the traction of the flexor pollicis tendon.
What is a stress fracture
Let's say you run a lot and don't recover well. Over time, tired muscles will no longer be able to absorb the shock load and will transfer it to the bones. Repeated stress causes microdamage to the bone, and if you add neglect of recovery and ignoring the symptoms of injury, then gradually these damages will become more noticeable and more serious. What happens next is called a stress fracture.
According to orthopedic surgeons, the second and third metatarsal bones of the foot are more susceptible to stress fractures than other bones. The area where they are located is most involved in running. She is responsible for repulsion.
Read on the topic: Inflammation of the periosteum: how to treat and how not to get it
Complications[edit | edit code]
The first of the possible diagnoses is to exclude a stress fracture of the femoral neck, since if this fracture is missed, the consequences can be most severe. Without proper treatment, it can develop into a complete fracture of the femoral neck, which is much more difficult to treat and may require open reduction of the fragments with internal osteosynthesis. Possible complications of a complete fracture of the femoral neck include delayed healing, nonunion, and avascular necrosis of the femoral head, the treatment of which may require femoral osteotomy or hip replacement, that is, operations after which it will be almost impossible to return to sports.
Area of injury
Stress fractures can affect the heel, the ankle, the midfoot, and even the pelvis, sacrum: in general, all those areas that are exposed to impacts, and the muscles, due to fatigue, cannot absorb them. But runners most often suffer from the bones of the lower leg or foot, because they are the ones that work the hardest for this sport. We are talking about load-bearing bones - the tibia and metatarsals.
Stress fractures of the leg and foot can be successfully treated, and if the fracture occurs on very strong bones of the pelvis or hip, this indicates health problems much more serious than a sharp increase in load and insufficient recovery.
Symptoms and diagnosis
The most common symptoms of a stress fracture are:
- Pain while running, walking and even at rest. If you experience pain while running that forces you to land on your foot differently than usual to avoid pain, consult a doctor.
- Sharp pain when pressing on the area where discomfort is felt.
- Swelling in the affected area, but most often swelling occurs in the top of the foot. For example, the outline of the veins on your injured leg may be more noticeable compared to the other foot.
To diagnose an injury, there is also a jump test: you need to jump several times on the leg that hurts, and if you feel pain when landing, this may indicate a fracture.
Training plans for marathon and half marathon. Download and start preparing today.
Good news: bone has a certain margin of strength. This means that pain hinting at a stress fracture appears long before it occurs. Timely measures will allow you not to fall out of the running program for one and a half to two months.
Stress fractures of the base of the metatarsal (Jones fracture)
This pathology has long been known to specialists due to the tendency of fractures to slow consolidation and nonunion, and sometimes to the development of a pseudarthrosis. It is believed that the high rate of nonunion in this fracture is due to circulatory failure.
The signs of a Jones fracture are quite clear. This is pain along the outer edge of the foot, swelling at the base of the fifth metatarsal bone. There is lameness when walking. Radiologically, a clearing area up to 0.3 cm in size in the wide part of the base of the fifth metatarsal bone is determined, having a wedge shape, thinning of the cortex.
Successful treatment requires early, reliable immobilization with the correct position of the fragments. It is difficult to achieve this using conservative methods. In this regard, surgical treatment for such patients may be justified, especially in athletes who need a quick return to professional sports. Surgical methods include tunnelization, arthroplasty with a sliding graft, and osteosynthesis with a tightening wire loop according to Müller. After the operation, a posterior plaster splint is applied from the toes to the level of the knee joint for up to 6 weeks. Subsequently, rehabilitation treatment is carried out (physical therapy, massage, physiotherapy) and after 4 weeks, athletes begin light training, and ordinary patients begin walking with full load. Metal structures are removed on average 4-5 months after surgery.
We present a clinical observation.
Patient K., 32 years old, a highly qualified football player, felt a sharp pain in the area of the outer edge of the foot while playing football. After stopping intense training, the pain disappeared. After 6 months, with the resumption of intensive training, pain in this area reappeared. Radiographs of the right foot revealed a fracture of the wide part of the base of the fifth metatarsal bone, passing through the cortex on both sides. An operation was performed according to the developed technique for the separation of sports and ballet injuries from CITO. After removal of the plaster cast, restorative treatment was carried out. Recovery was achieved, and after 3.5 months he began training.
What Causes a Stress Fracture
In simple terms, this injury is caused by insufficient recovery. Have you all heard about the golden rule of 10% increase in training loads? All this is not just like that, since both muscles and bones must get used to the load in order to be able to digest it. And it's not just about the mileage on your watch.
Stress fractures are typically the result of not only unusually high volume, but also a sudden increase in intensity when the body does not have enough time to adapt. In this case, the bone will simply exhaust all its resources for restoration.
Winter is the period when the risk of developing a stress fracture is greatest. Cause: Vitamin D deficiency. So remember that as an active person, you need higher levels of vitamin D than everyone else.
What else could put a runner at risk? Low calcium levels coupled with high caffeine intake flushes it out of the body. In addition, research shows that women with a low body mass index and older runners, whose bone density decreases as they age, are particularly at risk.
The influence of running technique
Running on your heel more often leads to stress fractures, according to global statistics. This placement of the foot puts more stress on the hip, increasing the likelihood of injury to the tibia. However, running from the forefoot is not without sin. For untrained feet, it carries the risk of stress fractures in the foot and ankle bones.
You should also pay attention to the surface. Let’s say you’ve been running along dirt paths all the time, and then in winter you switch to the arena, maintaining the same volumes. A sudden change of surface is fraught with danger, especially considering that the track in the arena involves turns, and asphalt, for example, is much harder than natural soil.
Read on the topic: Where is the best place to run: 9 running surfaces and their features
Prevention[edit | edit code]
Several factors predispose to stress fractures, which can be divided into extrinsic and intrinsic: extrinsic factors include footwear, playing field or track surfaces, and intensity of exercise, and intrinsic factors include osteopenia and various disorders of normal skeletal anatomy, such as varus deformity of the femoral neck. All these factors must be taken into account to prevent stress fractures. Thus, long-distance runners are better off wearing shoes with soft, elastic soles and running on a surface that is not too hard. In addition, gradually, rather than suddenly, increasing the load during training reduces the likelihood of any stress fractures.
Internal predisposing factors are more difficult to influence. Anatomical defects can be corrected using orthopedic devices. Osteopenia is more common in women and is part of the so-called triad of female athletes (including, in addition to osteopenia, an eating disorder and amenorrhea). It requires more active intervention from a doctor and the prescription of medications and a special diet.
Prevention
- Slowly increase the load and gradually make changes to the program. Experts recommend increasing volume by no more than 10 percent from week to week.
- Work on increasing your cadence: 80-90 steps per minute for one leg reduces the risk of injury.
- Don't do too much speed or tempo work. On easy days, run really easy;
- Include exercises to strengthen weak areas in your program. The key muscles are the gastrocnemius and tibialis anterior.
- If possible, consult a specialist who will evaluate your running technique.
- Vary your running surface.
- Eat a healthy diet: Get enough calcium and vitamin D. Take vitamin and mineral supplements for healthy bones.
- Give yourself recovery days after a tough session. Yes, you may feel full of energy, but the musculoskeletal system takes much longer to recover than the cardiovascular system.
Treatment and rehabilitation
The wisest thing to do after the first pain is to make an appointment with an orthopedic doctor. If you cannot do this right away, help yourself: stop running, apply ice 3-4 times a day for 10 minutes, take painkillers.
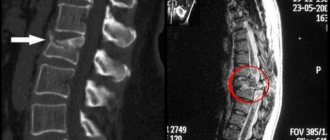
At your doctor's appointment, you will be prescribed an examination. This will likely be a CT or MRI scan as X-rays cannot detect a fracture at an early stage.
If an injury is confirmed, you will be restricted from activity and a cast will be placed over the injured area to support the bone while it heals. During this period, your main medicine is rest. Within 6-8 weeks, you should completely stop the activity that led to the injury and replace it with an activity that does not negatively affect the injury. For example, you can spin a bicycle or run skiing, roller skiing or rollerblading. Talk to your doctor, he will recommend a safe load.
How to replace running: 13 alternative training options
photo: Zoff-Photo/Getty Images, source: runnersworld.com
If running is resumed before complete healing, this can lead to a much larger fracture, which will make the bone problems chronic. Don't let your injury lead to surgery or, even worse, a complete bone fracture. Just imagine that treatment and rehabilitation in this case will take at least six months.
It should also be remembered that once a stress fracture occurs, it poses an additional risk for re-injury. This is a hint to continue to take care of your body.
Symptoms
Stress fracture on x-ray
The main symptom is severe pain during physical labor or sports. In addition, a stress fracture can also be determined by x-ray, but to get it done you will have to go to a medical institution. However, most people do not like to visit the clinic and go there only if the pain becomes too severe. But the problem is that a stress fracture is not accompanied by such severe pain as a closed and open fracture, so it is not possible to determine it.
However, there are symptoms that indicate that the body is malfunctioning:
- pain in the bone appears in waves, it increases when a person is in an active state and subsides in a calm state;
- severe swelling appeared at the site of microcrack formation;
- when you feel the limb, you feel a slight pain;
- presence of small bruises.
When visiting a doctor, an x-ray is prescribed. But sometimes the injury is so small that it cannot be seen on an x-ray, so when the patient is experiencing severe pain in the bones, but there is no apparent reason, magnetic resonance imaging is prescribed.
How to get back to running and exercising
So, after 8 weeks of rest from the impact of running, your muscles and bones have recovered. How to train? Of course, forget about previous volumes and do not try to update all your personal records. Exercise should be resumed gradually and stopped if you feel pain. Ignoring these simple recommendations increases the likelihood of a recurrent fracture.
During your gradual return to exercise, wear compression gaiters, a brace, or a support boot, depending on the location of the injury. They will take the pressure off the weakened area. For your running shoes, purchase special inserts or orthotics for better shock absorption.
Read more: 9 simple exercises to strengthen your feet
Treatment
First of all, a stress fracture is treated with rest and peace, and physical activity on the body should be completely limited. If you ignore the symptoms associated with a stress fracture, you can expect severe injury.
At the first symptom you need:
- keep the injured limb absolutely still;
- Apply a cold compress periodically.
Once a stress fracture is diagnosed, treatment can be conservative or surgical. The first type of therapy includes:
- Rest. The injured limb should be immobilized until the fracture heals.
- Orthopedic insoles or shoes. They help reduce the load on the injured bone;
- Gypsum bandage. It is used if the crack is large;
- Taking painkillers.
The surgical technique includes the introduction of fixing plates or wires.
During the rehabilitation period, the patient is prescribed anti-inflammatory, healing, warming ointments and compresses, physiotherapy, and physical therapy exercises. As the injured limb recovers, the patient can slowly return to physical activity, but this is done only under the supervision of a doctor.