The anterior cruciate ligament is responsible for the dynamic stability of the knee joint, fixing the tibia from non-physiological anterior displacement and supporting the lateral condyle of the tibia. More than 1/2 of the stability of the knee is provided by the ACL. That is why experts call this structure the first stabilizer of the knee; without it, the joint will not be able to function normally. It is located in the very center of the bony junction, crossing with the posterior cruciate ligament in an x-shape, which gave these two structural elements their names. We will now talk specifically about the ACL and its post-traumatic reconstructive plastic correction.
Anterior CS.
Rehabilitation after ACL plastic surgery: first week
Painkillers as prescribed by your doctor
Antibiotic as prescribed by a doctor
Working with the Arthromot or Kinetek mechanotherapy apparatus for the knee joint:
- Start working in the evening of the same day: flexion amplitude from 0 to 30 degrees three times a day (morning, afternoon, evening) for 1 hour
- Increase the flexion angle by 1 degree each session (or as tolerated). Make sure that working on the device does not cause sudden painful sensations; increase the degree of flexion and extension carefully and gradually. Make sure that the hip or foot does not lift, this indicates that the flexion angle is too high.
- Stimulate knee extension by placing a pillow or bolster under the ankle (without anything touching the back of the knee) for 30 minutes after each mechanical therapy session.
- The knee must always be in a knee joint orthosis, the only exception being work on a mechanotherapy apparatus. The orthosis is removed during the session. Some methods and doctors allow patients to be without an orthosis during the rehabilitation period
- Walking: use crutches to place measured weight on the operated leg (25% of the weight on the leg). The knee brace must be locked while walking.
Recommendations after discharge:
- Continue using the mechanotherapy device. The goal is to reach 90 degrees in 10 days.
- Lie with a bolster under your knee to encourage full knee flexion
- If necessary, continue to take pain medication as recommended by your healthcare provider.
- Keep seams dry
Indications for surgery
Arthroscopic plasty of the ACL of the knee joint is not performed immediately after the incident to avoid complications. As a rule, a surgical session is not scheduled until the inflammatory focus and swelling are eliminated. Throughout this period, competent conservative medical care and limb immobilization are provided.
For what identified problems will it be necessary to undergo ACL reconstruction of the knee joint after some time? There are certain factors that are a clear reason for performing plastic surgery using arthroscopy, these are:
- transverse rupture of the ligament along the entire line of width;
- absolute separation of fibers from the place of attachment to the bone;
- partial injury with a pronounced degree of knee instability;
- unsuccessfully performed plastic surgery of the injured ACL of the knee joint, which did not contribute to stabilization due to incorrect transplantation;
- chronically recurring sprains and tears;
- unsuccessful conservative treatment.
Important! Let us remind you once again that a reconstructive procedure is not performed immediately after an injury, but this does not mean that the victim does not need the help of a traumatologist. In order not to aggravate the problem, you need to immediately get examined, get qualified recommendations from a specialist and immediately begin to implement them! As an exception, immediate surgery can be performed either for extensive combined trauma (ACL rupture in combination with injuries to bones, menisci, or other ligaments), or for athletes to quickly return to professional sports.
Rehabilitation after ACL plastic surgery: 10 days after surgery (first visit to the doctor)
Mobilization of the knee joint by the patient
Range of motion: knee bending up to 90 degrees on a mechanotherapy apparatus
Full extension support (roller under the ankle or ankle three times a day)
After finishing work on the mechanotherapy apparatus, begin independent exercises:
- Allow your leg to bend 90 degrees
- Active extension up to 45 degrees
- Passive extension from 45 degrees to full extension (using unaffected leg)
- Meniscus repair: limited range of motion (usually up to 90 degrees, unless otherwise recommended by a doctor)
Wearing a knee orthosis:
- wear the orthosis all the time, remove it while taking a bath and working on the device
mechanotherapy Artromot K1 or Kinetek
- lock the orthosis while you sleep
- If you have good control of your quadriceps, after three weeks, unlock the orthosis while walking (provided that your doctor has allowed it)
Walking: Gradually add weight to your leg as tolerated.
General information about damage
Anterior cruciate ligament reconstruction is the most common knee ligament procedure. The remaining ligaments of this section of the lower extremities are much less likely to be injured and rarely require surgical intervention. For example, the ACL is injured approximately 15 times more often than the PCL. Some sources even indicate that it is 30 times. The explanation for this is the specific anatomical structure of the ACL: it is longer and thicker than the posterior connective tissue cord.
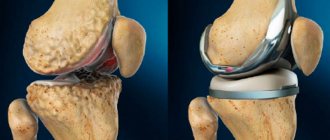
Image of gaps.
Violation of integrity, namely its ruptures, mainly occurs due to sports injuries, as well as as a result of falls with legs fixed parallel to the surface (skier injuries), unsuccessful landings after a jump on straightened legs. Damage to the ligamentous bundles can also occur due to a strong blow to the back of the knee, twisting and sudden movements, for example, during a sharp turn or sudden braking while running. It is possible to recognize that a particular ligament has been damaged only through certain diagnostic tools:
- MRI (CT and X-ray are less effective);
- diagnostic arthroscopy;
- special clinical tests, for example, “anterior drawer”, Lachman, Pivot Shift test, etc.
What does the injury look like on an MRI?
As for the symptoms that may indicate a similar problem, they are pronounced, especially in the early period. The clinical picture of a complete rupture is as follows:
- cracking immediately at the moment of rupture;
- acute severe pain in the knee;
- the painful syndrome intensifies with any attempt to move the leg;
- the lower leg is shifted forward;
- rapid increase in swelling;
- hemorrhage in the joint;
- dysfunction of supporting ability.
The above signs are inherent in diseases of other components of this joint, so to confirm it you will definitely need to undergo an examination by a traumatologist and diagnostic procedures. Depending on the severity of the rupture (micro rupture, partial or complete), the doctor will select adequate treatment tactics. For non-serious injuries, conservative therapy is used; complex cases require surgical treatment.
Due to the destructuring of the frontal cruciate ligament, the biomechanics of the joint as a whole suffers: joint instability and pathological displacement of the articular surfaces relative to each other occur. This adversely affects the cartilaginous coverings of interacting bone units - they begin to suffer from irrational loads during movements. If the ligamentous apparatus is not corrected in time, gonarthrosis may develop, which leads to serious degeneration of not only the articular cartilage, but also the menisci.
Torn fibers are visible through the arthroscope.
Attention! A completely torn anterior cruciate ligament of the knee joint without plastic surgery is not able to unite and heal on its own. Therefore, to restore its functionality, if the defect is truly serious, an arthroscopic procedure is prescribed to restore the integrity of the ACL.
Rehabilitation after ACL reconstruction: 4 weeks after surgery
Start putting full weight on your leg.
Gradually wean yourself off crutches
The seams may get wet when taking a bath, it is recommended to limit yourself to a shower
Gradually move on to the exercises:
- Include closed kinetic chain exercises that involve highly directed forward and backward movements of the leg. In this case, both parts of the limb must be fixed and should not dangle freely
- ¼ volume squats
- steps up the stairs (approximately 3 cm high)
Open kinetic chain exercises, in which one part of the limb is in a free state:
- flexion: active and passive, full range of motion
- extension: not to final position
- passive only: from 45º to 0º
- active: from 90º to 45º
- Leg raise with bent knee (>45º)
- Isometric exercises
- Stationary bike when the flexion angle reaches 90º
Contraindications for surgery
Despite the fact that cruciate ligament repair of the knee joint is one of the most popular techniques due to its high efficiency and minimal invasiveness, it cannot be performed on everyone. Fortunately, there are not many contraindications:
- severe contracture of the joint;
- local skin infections, inflammations, purulent abscesses, ulcers;
- severe forms of pathology of the heart, respiratory system, veins and blood vessels of the legs;
- any chronic diseases in the acute stage;
- allergy to medications used for anesthesia.
If transplantation of own tendons from the quadriceps femoris muscle or patellar ligaments is intended, and the patient has problems with the muscle-tendon elements of the flexor/extensor apparatus, such a procedure cannot be performed. However, he may be offered one of two alternative options: allotransplantation or implantation of the Legamis system. Of course, if the clinic provides such services.
Rehabilitation after ACL reconstruction: 6 weeks after surgery
Schedule a knee x-ray
Scheduled visit to the doctor: you can remove the orthosis
Continue physical exercise (three times a day):
The main task of this stage is to achieve full knee flexion.
in case of meniscus repair: removal of restrictions on movement after 4-6 weeks
Continue closed kinetic chain exercises
Begin open kinetic chain exercises without resistance
Eight weeks: Begin isotonic (in motion) extension from 90 to 45 degrees
Start isokinetic exercises from 90 to 45 degrees on stationary machines. Isokinetic exercises involve lifting weights on special machines or exercises using any fixed solid object that can provide insurmountable resistance to the muscles (for example, a wall).
Damage to the cruciate ligament of the knee
At this stage of medical development, surgery to restore the cruciate ligament is performed using arthroscopy, through the smallest possible incisions.
Most surgeons prefer to reconstruct the anterior cruciate ligament using a graft from the patient's own tendons and ligaments.
A transplant that is formed using the patient's own tissue is called an autograft in medicine.
Most ligament reconstruction surgeries are performed on an outpatient basis, meaning many patients can go home the same day after surgery. Some patients may need to stay in the hospital for two or three nights.
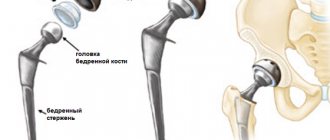
There are many different ways to reconstruct the anterior cruciate ligament. One of the most commonly used is to take the semitendinosus and gracilis tendons from the patient, form them into a graft, and place it in place of the torn anterior cruciate ligament.
In some cases, to restore the anterior cruciate ligament, for example, in professional athletes or in elderly people with severe artosis, a special synthetic endoprosthesis can be used. The use of synthetic endoprostheses has a number of advantages and disadvantages.
The advantages include the high strength and inertness of the synthetic endoprosthesis to the tissues of the body, which allows for aggressive rehabilitation immediately after surgery, there is no pain at the site of taking the tendons of the semitendinosus and tender muscles, the anatomy of the muscles of the posterior surface of the thigh and the function of the flexor apparatus of the knee joint are not disturbed.
Disadvantages include the low elasticity of the synthetic endoprosthesis, which requires precise positioning of the bone canals, as well as the low bioavailability of this method of reconstruction of the anterior cruciate ligament.
Surgery technique using a graft from the tendons of the pes anserine (semitendinosus and tender muscle)
The muscles of the back of the thigh in humans are well developed. They originate from the pelvis and femur, cross the knee joint on both sides and attach to the lower leg.
The tendons for the graft are taken from the semitendinosus and gracilis muscles, which are attached by their tendons along the inner surface of the leg.
During surgery, the surgeon uses a special optical device (arthroscope) to control manipulations inside the joint. This surgical technique does not require the surgeon to make large incisions in the joint area, which significantly speeds up healing and recovery after surgery.
Anterior cruciate ligament (ACL) reconstruction surgery is usually performed under spinal anesthesia.
The surgeon begins the operation by making two mini punctures in the joint area of no more than 4 mm, through which an arthroscope and special mini-instruments are inserted into the joint. After the joint cavity is examined and the diagnosis is confirmed, the surgeon makes a small incision in the soft tissue in the projection of the attachment of the tendons of the semitendinosus and tender muscles and removes them with a special tool.
The tendons are specially processed and folded 3 or 4 times, which significantly increases the strength of the entire graft.
Next, the surgeon prepares the knee joint for implantation of a new ligament. The remains of the damaged ligament are removed, and if necessary, the intercondylar space is expanded so that the graft is not damaged. This manipulation is called notch plastic.
Once this is done, special instruments are used to drill holes in the femur and tibia through which the autograft will be inserted.
Very important at this stage is the correct location of the canals in the femur and tibia, only under this condition will the ligament work correctly and the patient will not feel pain and instability.
Subsequently, the autograft, under arthroscope control, is pulled through the canals and joint cavity, stretched with a certain force and fixed intraosseously with special screws or buttons.
Then the range of motion in the joint is checked, drainage is installed, sutures are applied, and the leg is placed in a postoperative orthosis.
Surgery technique using a graft from the patellar ligament
Another long-established method of reconstruction of the anterior cruciate ligament is arthroscopic plasty using an autograft from the tendon of the patellar ligament. For the operation, a strip of tendon with bone blocks at each end is removed.
The advantage of this type of autograft is its inherently greater strength and the possibility of rapid rehabilitation.
The tendon of the patellar ligament is very thick and strong, located on the front surface of the knee joint. It starts from the lower pole of the patella and is attached just below the knee joint to the tibia. The main function of the patellar ligament is to extend and elevate the leg.
When using the tendon of the patellar ligament as an autograft, the surgeon removes a strip of tendon, usually in its middle part, and also cuts out bone blocks from the patella and tibial tuberosity fixed to it.
The anatomy of the graft helps speed healing and create a strong attachment of the new ligament to the tibia and femur. When a graft is implanted, bone blocks are placed into bone canals. The surfaces of the bone walls of the canal and the bone blocks of the graft are in contact with each other and heal over time, like a normal fracture.
The surgeon performs the operation using an arthroscope connected to a monitor; this method allows you to control manipulations inside the joint without performing extensive soft tissue incisions, which were practiced in the pre-arthroscopic era. This surgical technique significantly speeds up recovery and is characterized by significantly lower pain and swelling after surgery.
Surgical procedures for reconstruction of the anterior cruciate ligament (ACL) are usually performed under spinal anesthesia. The orthopedic surgeon begins the operation by making two skin punctures, through which an arthroscope and special mini-instruments are inserted into the joint cavity. After inspection of the joint cavity and confirmation of the diagnosis, two small incisions are made in the projection of the patellar ligament. Precautions are taken to avoid damaging nearby nerves and blood vessels.
Working through small incisions, the surgeon removes the middle portion of the patellar tendon with two bone blocks from the patella and tibia.
The bone blocks are rounded and smoothed, and holes are drilled in the blocks through which strong threads are passed, through which the autograft will be pulled through the tunnels in the femur and tibia and stretched.
Next, the surgeon prepares the knee joint, removes degenerative tissue,, if necessary, sutures the meniscus, and resects the remains of the damaged anterior cruciate ligament.
Once this is done, bone canals are drilled into the femur and tibia.
The holes in the bones are located in such a way that the autograft, passed through them and fixed, functions as the original anterior cruciate ligament.
The graft is then pulled through the tunnels in the bones, stretched and secured with screws or special buttons.
After arthroscopic control of the position of the ligament, drainage is installed in the joint cavity, and sutures are applied to the soft tissue.
Rehabilitation is not aimed at a specific person
Linda Truong (2020) reviewed that there are many psychological, social and contextual factors that influence all stages of sports injury recovery. A better understanding of these factors, both at the time of injury and throughout the rehabilitation period, could help optimize patient management or achieve desired outcomes. For example, promoting a speedy return to sport, as well as helping to ensure a better quality of life and health in the long term.
What we often do wrong is that we don't target our interventions enough to the individual. No two rehabilitation programs are alike. Not only because of the physical impairments associated with ACL injury or reconstruction, but also because of the psychological, social, and contextual factors that have a profound influence on the recovery process. Hence the conclusion: treat the person, not just the knee.
Low compliance and motivation
Research has shown that patient compliance with the rehabilitation program and motivation to exercise are key factors in predicting outcome. You can prescribe the best rehabilitation program in the world, but that program can only be effective if it is effectively implemented. Patients who perform less well on the program, who do not follow the program as well as they should, and who have less motivation for rehabilitation typically have less optimal outcomes after ACL injury and reconstruction.
As physical therapists, we play a key role in motivating patients and maintaining the highest possible compliance. For example, by setting realistic expectations, open communication with patients, and setting goals for both the short and long term. Provide feedback and involve the patient in the rehabilitation program. Remember to evolve your program, make it challenging, and don't forget to have fun.
Risk factors
- Genetic (hyperelasticity, hypermobility of joints and connective tissue).
- Anatomical factors (width of the intercondylar space, tibial plateau inclination, valgus).
- Hormonal factors (in women, the risk of ACL rupture increases 2-5 times depending on the cycle).
- Internal factors (diabetes).
- External factors (nutrition, quality of coating, shoes, humidity, etc.).
- Muscle biomechanics (muscle imbalance - predominance of quadriceps strength over flexor muscles).
Relevance of ACL rupture
The relevance of ACL injuries is confirmed by statistical data from different countries:
- The number of new cases in Europe is 250-300,000 per year (M. Yabroudi, H. Bjornsson 2016). At the same time, about 100,000 reconstructions are carried out annually. According to insurance companies, most injuries occur among skiers. For example, in Germany there are 32 people per 100,000 of the total population, in France - 47 per 100,000.
- In the USA, the number of primary ACL reconstructions per year is 100,000 operations, including up to 50 per 100,000 people among skiers.
- According to national registries since 2004 in Scandinavia: In Sweden, 17,000 primary anterior cruciate ligament reconstructions and 1,000 revisions are performed annually. Of these, skiers account for 32 per 100,000 people.
- In Denmark 38 per 100,000 people.
- In Norway 34 per 100,000 people.
Clinical manifestations of ACL damage during diagnosis.
From the observation of 587 cases of isolated ACL injuries carried out at the Sports Clinic from 2015 to 2021, the following distribution of knee joint instability was determined:
- In 146 cases or 24.8% when the injury lasted no more than 2 months, instability of the knee joint did not manifest itself during diagnostic tests.
- In 426 cases or 72.6% with an injury period of more than 1 year, instability was mildly expressed in one plane.
- And only in 15 cases (2.5%) significant multiplanar instability was observed, including anteroposterior displacement of the tibia, an increase in pathological adduction/abduction + rotational component.
Thus, in only 2.5% of cases, additional surgical procedures were required in addition to ACL reconstruction.
The gap between research and practice
Second, there is a clear gap between what we know from research and what is routinely done in clinical practice. This could be due to many reasons. For example, for many physical therapists, it can be very difficult to keep up with the times because there is no time to delve into individual studies while working in a clinic all day. Additionally, as mentioned in the first point, research findings are often too nonspecific to be directly translated into clinical practice.
What complications can there be?
After the intervention, there is a risk of developing undesirable consequences. Among them:
- Joint contracture (may occur due to improper intervention).
- Arthrosis, degenerative changes in the knee.
- Pain, limited mobility.
- Displacement or tearing of the transplanted tissue.
- Material rejection is extremely rare.
- Allergic reaction to anesthesia.
Full recovery takes about four months. In 95 cases out of 100, the operation is successful.
Rehabilitation is carried out in a hurry
There is no need to rush during rehabilitation. It should not be the case that we skip a few steps or stages to speed up recovery. In fact, we often move too fast. We know that from both a functional and biological perspective, we need time to reach our maximum potential after such severe injuries.
A combination of criteria focusing on the patient's functional status combined with time since injury and/or reconstruction should be used. The takeaway from this point is: don't rush. Be patient. Take your time to improve and achieve your goals. From the patient's perspective, rehabilitation after an ACL injury can be very difficult.