Injuries and wounds of the chest
CLASSIFICATION OF INJURIES AND WOUNDS OF THE CHEST
Closed chest injuries (bruises, compression of the chest organs, fractures of the sternum, ribs, collarbone, scapula) prevail over open ones by 9 times and account for more than 6% of patients with injuries:
- without damage to internal organs (71.8%)
- with damage to internal organs (28.2%)
In each of these divisions, it is necessary to indicate the presence or absence of damage to the bones of the chest of other parts of the body.
Closed chest injuries are more often associated with motor vehicle accidents and falls from height. With closed injuries, the bone base of the chest is primarily damaged. This circumstance is the main cause of trauma to the thoracic cavity organs. Pathological changes vary from ordinary bruises to deep tears and ruptures of organs, partial crushing, and in some cases even complete separation. In addition, these injuries are often accompanied by damage to organs in other areas.
Open chest injuries are divided into:
- penetrating
- non-penetrating
In peacetime conditions, the vast majority of chest wounds (up to 97.3%) are so-called domestic. Wounds are inflicted by cutting, piercing objects, as well as firearms. In most individuals, the injuries are penetrating in nature (3 - 3.5% of the entire injury and 50 - 67% of the chest injury). Penetrating injuries are divided into:
- stab and gunshot
- blind and through
- unilateral, bilateral, multiple, combined
- with pneumothorax (open and closed), hemothorax, pneumohemothorax, chylothorax
- with injury to the pleura, lung, trachea, bronchi and other organs of the chest cavity
- thoraco-abdominal wounds (with and without damage to the thoracic and abdominal organs).
The size of the external wound in no way indicates the nature and extent of intrathoracic damage. Among penetrating wounds, blind wounds predominate (97.8%), which pose a real threat to viewing injuries to the chest organs. Gunshot wounds are superior in nature and severity to stab wounds, as they are accompanied by more extensive damage and greater bacterial contamination.
Combined injuries are injuries caused by exposure to one type of energy, but with damage to two or more of the seven anatomical areas of the body, which are characterized by clinical diversity, difficulty in diagnosis, duration of treatment, and difficulty in determining the required volume and nature of assistance. Combined chest injuries account for up to 33% of cases.
Combined - caused by the action of multidirectional energy (combination with a burn, stab wound with a gunshot, etc.) and account for 1.5% of chest injuries.
DIAGNOSIS OF INJURIES AND WOUNDS OF THE CHEST
For some injuries, the diagnosis is obvious (“sucking” wound of the chest wall, fenestrated rib fracture), while for others it is quite complex (aortic rupture, tracheal damage). In order not to miss severe injuries to the chest organs, the examination must be complete, consistent and fairly rapid. Treatment begins immediately in accordance with the general principles of resuscitation (infusion therapy, ensuring airway patency, hemodynamic stabilization). Associated injuries, which most often include fractures, head and abdominal injuries, are often more dangerous than chest injuries. Therefore, treatment priorities should be determined from the very beginning.
2.1 History and physical examination
The main purpose of the initial examination is to detect life-threatening conditions and determine their cause. The main life-threatening conditions that occur with chest injuries and require emergency care include:
- cardiac tamponade;
- massive hemothorax;
- tension pneumothorax;
- open pneumothorax;
- the presence of a rib valve;
- diaphragm rupture.
When examining a patient, pay attention to:
- Cyanosis is a sign of increasing hypoxia caused by respiratory failure. If only the face, neck and upper half of the chest (“neckline”) are bluish, one should suspect traumatic asphyxia caused by compression of the chest. Traumatic asphyxia is also characterized by pinpoint hemorrhages in the skin, mucous membranes, and under the conjunctiva.
- Spontaneous breathing – presence or absence; retraction of the intercostal spaces during inspiration (respiratory failure, airway obstruction); paradoxical breathing (fenestrated fracture with flotation of the chest wall); unilateral respiratory movements (bronchial rupture, pneumothorax, hemothorax); stridor (damage to the upper respiratory tract). Symptom of “interrupted inspiration”, Payr’s symptom (pain when bending to the healthy side).
- Swelling of soft tissues, especially the eyelids and neck (subcutaneous emphysema) is a sign of damage to the lung or main bronchus.
- Unusual breathing sounds (stridor, etc.), “sucking” wound of the chest wall.
- The presence of entry and exit wound openings for penetrating wounds, and it is necessary to examine both the anterior and posterior surfaces of the body.
2.2 Monitoring blood pressure, heart rate and pulse
The pulse is palpated in each limb. The absence of a pulse may be due to damage to a large vessel. Be sure to compare the results of blood pressure measurements and pulse parameters on symmetrical limbs. With cardiac contusion and electrolyte disturbances, arrhythmias may occur. In this case, ECG and EchoCG are indicated; Antiarrhythmic drugs may be required. Alternating pulse (alternating high and low pulse waves) is observed with cardiac contusion and myocardial dysfunction caused by other reasons, incl. electrolyte disturbances. A weak, rapid pulse is a sign of cardiac tamponade or hypovolemia. A racing pulse (high with low diastolic and normal or high systolic blood pressure) appears with damage to the aortic valve and acute aortic insufficiency.
2.3 Palpation
The neck, chest, arms and abdomen are quickly palpated. Subcutaneous emphysema is a sign of tension pneumothorax or bronchial rupture. The ribs and sternum are sequentially palpated, and the chest is lightly compressed in different directions. Pay attention to the symmetry of the chest, the nature of the respiratory movements, and a section of the chest wall moving in an unnatural direction (“costal valve”). If a rib is fractured with displacement, the organs of the thoracic cavity may be injured by a sharp bone fragment. Swollen, non-pulsating neck veins are a sign of cardiac tamponade. In addition, swelling of the neck veins is observed during agony, as well as during intensive infusion therapy.
2.4 Auscultation and percussion
When auscultating the lungs, breath sounds in the right and left lungs are compared. If they differ, perform percussion. Dullness of percussion sound on the affected side means either hemothorax or atelectasis (blockage of the bronchus by a mucus plug, aspiration of a foreign body). A loud tympanic sound over one lung, especially in the case of a penetrating wound on that side, is a sign of pneumothorax. Listen to heart sounds. Heart murmurs may indicate valve damage, which often occurs with blunt chest trauma, rupture of the papillary muscles or ventricular septum. If a noise resembling crunching snow (pericardial friction rub) is heard during diastole, there may be air in the pericardial cavity.
2.5 Primary X-ray examination
After a brief physical examination, a plain chest x-ray is performed. Usually, bedside radiography is sufficient (a picture in the posterior direct projection), but if the patient’s condition allows, it is better to take photographs in the anterior direct and lateral projections. Radiological signs that you should pay attention to first:
- increased transparency of the lung, the border of the lung crosses the shadows of the ribs;
- partial or complete darkening of the pulmonary field;
- subcutaneous emphysema, pneumomediastinum;
- rib fractures;
- mediastinal shift;
- widening of the mediastinum (more than 8 cm in the posterior projection in an adult patient lying on his back - a sign of rupture of a large vessel);
- absence of the contour of the aortic arch in direct projection, posterior or anterior (a sign of aortic damage);
- deviation of the nasogastric tube to the right (possibly due to aortic rupture);
- enlargement of the heart shadow, straightening of the left border of the heart;
- gas bubbles in the stomach and intestines above the diaphragm (diaphragmatic rupture);
- damage to the thoracic and upper lumbar vertebrae.
2.6 Other research methods
An ECG is performed on all patients. Particular attention is necessary in case of blunt trauma - a strong blow to the chest or a fall with the chest onto a hard object. Heart rhythm disturbances, changes in the ST segment and T wave, characteristic of myocardial ischemia, are signs of cardiac contusion.
Echocardiography, expertly performed in the emergency department, is a valuable diagnostic method. Transesophageal echocardiography is not recommended if aortic rupture is suspected, since fluctuations in blood pressure during the study may aggravate bleeding or provoke rupture of a pulsating hematoma.
An X-ray examination of the esophagus is performed if perforation is suspected. Damage to the esophagus should be excluded in case of neck wounds, gunshot wounds of the mediastinum, and puncture wounds of the back. It is advisable to use water-soluble radiocontrast agents, especially if a violation of the integrity of the intestine is suspected. Esophagoscopy is less reliable because small injuries to the esophagus are easily missed.
Targeted radiography of the ribs for extensive chest injuries is usually not necessary. It is used to diagnose isolated rib fractures in minor injuries, as well as for complaints of persistent chest pain after injury. If a sternal fracture is suspected, an x-ray of the sternum in a lateral projection is indicated, since plain x-rays in this case are not very informative.
Arterial blood gases are measured immediately after admission to assess pulmonary ventilation. In the future, regular measurements of blood gases are carried out in all intubated patients, as well as in those with a high risk of developing respiratory failure (pulmonary contusion, fenestrated rib fracture). If peripheral circulation is not impaired, pulse oximetry is used.
Aortography is the only method that can accurately diagnose aortic rupture. The images should show the aorta (from the aortic valve to the aortic opening of the diaphragm) and all branches of the aortic arch. In diagnosing aortic rupture, aortography is more informative than CT - it allows you to simultaneously see the entire vessel and its main branches, that is, all possible areas of damage. In addition, a hematoma detected on a tomogram does not necessarily mean damage to a large vessel, and vice versa, damage to a large vessel is not always accompanied by heavy bleeding into the mediastinal tissue.
Bronchoscopy is performed if damage to the bronchi is suspected. Indications: hemoptysis after blunt chest trauma, stridor, neck injury, perforating injury to the mediastinum, release of large amounts of air through drains from the pleural cavity. In addition, bronchoscopy is used to remove aspirated foreign bodies. During the study, all airways are examined - from the vocal folds to the distal parts of the bronchial tree. If the patient is intubated, to examine the upper airway, the endotracheal tube is carefully pulled toward the vocal folds by deflating the cuff.
Emergency thoracoscopy should be performed in the operating room. The method makes it possible to detect bleeding from the intercostal arteries, hemopericardium, damage to the diaphragm with prolapse of the abdominal organs into the chest, and lung damage. Examinations can be performed under local or general anesthesia, using a rigid mediastinoscope or more modern endoscopic techniques.
PRINCIPLES OF TREATMENT
After carrying out resuscitation measures and making a preliminary diagnosis, treatment tactics are determined. There are three options: drainage of the pleural cavity, surgery or expectant conservative therapy. In most cases, for blunt trauma and penetrating chest wounds, conservative therapy, alone or in combination with the installation of drains, is sufficient.
3.1 Indications for drainage of the pleural cavity
- Pneumothorax (any degree). Having installed drainage into the pleural cavity, monitor the amount of incoming air and released contents. If bleeding occurs into the pleural cavity and a large amount of air is released, surgery may be required. To decide on the installation of drainage, you can focus on the indications established for spontaneous pneumothorax: air occupies more than ⅓ of the lung field, increasing or tense pneumothorax. However, in this case, continuous monitoring of the lung condition and dynamic radiography is required, which is often impossible due to concomitant injuries and surgical interventions on other organs.
- “Sucking” wound of the chest wall. The drainage tube is installed through the counter-aperture. This allows for complete surgical treatment and suturing of the main wound.
- Acute hemothorax (any degree). Installing a drainage allows you to evacuate the spilled blood and monitor the intensity of bleeding.
- Subacute hemothorax (moderate or total). If the hemothorax does not increase, but is accompanied by clinical symptoms, they first try to remove the blood using pleural puncture. If this fails, and blood occupies more than ⅓ of the lung field, installation of drainage is indicated. If blood occupies less than ⅓ of the lung field, hemothorax may resolve on its own, usually within 6 weeks; when clinical symptoms appear, they resort to pleural puncture or drainage.
Installation of drainage for prophylactic purposes is not indicated. The exceptions are severe injuries to the chest (for example, fenestrated rib fractures) and the need for mechanical ventilation in the absence of access to the pleural cavity (surgical intervention in any position of the patient, except for the supine position, orthopedic interventions). The decision to install drainage in these cases is made individually. Passive drainage with a water seal or aspiration drainage is used. Drainage is stopped when less than 50 ml is separated through the drains. liquid per day, the release of air completely stopped, and the patient was transferred to independent breathing. During drainage of the pleural cavity, prophylactic antibiotic therapy is not necessary.
3.2 Indications for surgery
- Cardiac tamponade. During preparation for surgery, pericardial puncture and infusion therapy may be required.
- Extensive gaping wound of the chest wall.
- Penetrating wounds of the anterior and superior mediastinum with possible damage to internal organs (signs of pneumothorax, hemothorax, cardiac tamponade). The risk of cardiac injury is considered high if the entry hole is in the area bounded by the costal arches, clavicles and midclavicular lines. The localization of the wound in itself is not an indication for surgery; when deciding on surgical intervention, many surgeons are guided by hemodynamic parameters and the clinical picture. Others, given the high likelihood of heart damage, perform emergency exploratory surgery on all patients. In case of a through wound of the mediastinum, surgical intervention is usually resorted to due to hemodynamic instability. The course of the wound channel is often unknown, especially with bullet wounds; Damage to many internal organs is possible. Previously, a penetrating wound of the mediastinum was considered an absolute indication for diagnostic surgery. Currently, if the patient's condition is stable, echocardiography, aortography, esophagoscopy and bronchoscopy are performed. In the absence of pathology, expectant conservative therapy is indicated. If surgery is necessary, a surgical approach (sternotomy or bilateral anterolateral thoracotomy) should be carefully considered. Sternotomy is not suitable for examining the esophagus and descending aorta.
- Continuing or profuse bleeding into the pleural cavity.
- after installing the drainage, more than 1500 ml was immediately received. blood;
- In the first hour, more than 500 ml was received through the drainages. blood;
- blood flow through the drains in the following hours exceeds 150 - 200 ml/h;
- an increase in the amount of blood separated through drainages, regardless of the initially received volume;
- accumulation of blood in the pleural cavity, accompanied by clinical symptoms and not amenable to drainage (after x-ray confirmation).
- The release of a large amount of air through the drainages, regardless of whether the lung expands or not.
- Established rupture of the trachea or main bronchus.
- Diaphragm rupture.
- Aortic rupture of any location.
- Perforation of the esophagus.
- Foreign bodies of the chest cavity (knife, bullet, shrapnel, etc.). All foreign bodies with the exception of bullets must be removed. Foreign bodies are removed during surgery, after providing access to the affected organ and the ability to quickly stop bleeding, since a foreign body stuck in the myocardium or pulmonary parenchyma usually packs the wound and prevents bleeding.
The ineffectiveness of resuscitation measures for extensive chest injuries is an indication for direct cardiac massage and the application of a clamp to the descending aorta to temporarily block blood flow.
In case of thoracoabdominal injury with signs of life-threatening intra-abdominal bleeding, the operation usually begins with laparotomy; The pleural cavity is drained at this time and the discharge is observed through the drains. Absolute exceptions to this rule are cardiac tamponade and profuse bleeding into the pleural cavity; relative - the release of a large amount of air through the drains and rupture of the aorta with the formation of a pulsating hematoma. In the last two cases, you can try to postpone the thoracotomy and first stop the intra-abdominal bleeding, but the patient should be prepared for both operations simultaneously. If the need arises, a second team of surgeons proceeds with an emergency thoracotomy.
There is no consensus regarding the tactics of treating penetrating wounds of the mediastinum in the absence of signs of damage to internal organs. Conservative treatment of such injuries requires:
- hospitalization of the patient in the intensive care unit;
- installation of a catheter in the central vein and hourly measurement of central venous pressure;
- installation of an arterial catheter and blood pressure monitoring;
- conducting echocardiography upon admission;
- plain radiography of the chest over time (first after 4–6 hours, then according to indications);
- hourly measurement of the volume of discharge through drains.
Close monitoring of the patient and timely adjustment of treatment are mandatory.
3.3 Antibiotic therapy
Antibiotic therapy begins immediately upon admission and continues until the postoperative fever ends and the number of leukocytes in the blood normalizes. During surgical interventions for blunt chest trauma (“clean” wounds), antibiotics are prescribed in the same way as for planned operations: 1 time before and 2–3 times after surgery. Indications for long-term use of broad-spectrum antibiotics are: heavily contaminated wounds, foreign bodies, prosthetics. It is not necessary to prescribe antibiotics during drainage of the pleural cavity.
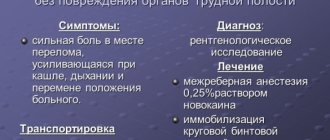
3.4 Pain management
Anesthesia is absolutely necessary for severe chest injuries, including rib fractures, during drainage of the pleural cavity and in the postoperative period, i.e. when it is necessary to ensure full independent breathing and cleanse the respiratory tract of mucus. Analgesics can be prescribed orally, intramuscularly or intravenously. Any medications can be used.
Intercostal conduction anesthesia is performed after thoracotomy, with multiple rib fractures, and with pain at the site of drainage installation. Typically, several intercostal spaces are blocked above and below the wound with lidocaine (or lidocaine in combination with epinephrine). Under the lower edge of the rib at the lateral edge of m. erector spinae (i.e. 2.5 cm lateral to the site of exit of the intercostal nerve from the intervertebral foramen) 5 ml is injected. 0.5 – 1% lidocaine. A needle is used for a spinal puncture. Do not damage the pleura or allow the drug to enter a blood vessel. You can block 4–5 intercostal spaces at a time. If there is no drain installed on the side of the chest where anesthesia is performed, a chest x-ray is indicated after the procedure.
Epidural anesthesia is performed once or a catheter is installed for long-term infusion of anesthetic. For infusion, you can also use a mixture of a local anesthetic with a narcotic analgesic (for example: 20 ml of 0.5% bupivacaine + 200 mcg of fentanyl + 26 ml of 0.9% NaCl; administered at a rate of 5 - 8 ml/h). This type of pain relief is especially effective for chest pain. Consultation with an anesthesiologist and follow-up by a qualified nurse are necessary.
If suction drainage is not used, an analgesic can be injected into the pleural cavity.
3.5 Selecting online access
In case of damage to the heart and great vessels, preference is given to longitudinal sternotomy. The left anterolateral approach is also convenient; the incision is made in the IV – V intercostal space and, if necessary, expanded laterally. However, with this access it is difficult to approach the mouth of the great vessels.
If the brachiocephalic trunk is damaged, a sternotomy is performed, moving to the neck along m. sternocleidomastoideus or along the collarbone.
In case of unilateral total hemothorax, an anterolateral or posterolateral thoracotomy is used on the injured side. For right-sided hemothorax, they prefer to position the patient on his back, since in the position on the left side, cardiopulmonary resuscitation, if necessary, is extremely difficult.
The optimal access to the thoracic aorta is a left posterolateral thoracotomy in the fourth intercostal space (the aortic arch is usually located here during single-pulmonary ventilation). However, if spinal injury cannot be ruled out, an anterior approach is used and the apex of the lung is retracted or a single-lumen endotracheal tube with a bronchial blocker is used to visualize the thoracic aorta. A large diameter Fogarty catheter can be used as a bronchial blocker.
If hemopericardium is suspected, a diagnostic subxiphoidal pericardiotomy is performed (as an independent intervention or during surgery on the abdominal organs). A skin incision 5–7.5 cm long is made above the xiphoid process and the aponeurosis is dissected along the white line of the abdomen. The xiphoid process is excised, the mediastinal tissue is bluntly peeled off, the pericardium is exposed and dissected. If blood is detected in the pericardial cavity, a sternotomy is performed, the bleeding is stopped, and the wound of the heart or great vessel is sutured. The subxiphoid approach is used for diagnostic purposes only; It is not suitable for specialized operations.
PREVENTION OF PULMONARY COMPLICATIONS (PNEUMONIA, ATELECTASIS)
The purpose of the measures is to ensure the release of mucus from the airways and deep breathing. Aspiration of sputum through a tracheal tube, percussion and vibration massage, postural drainage, spiro-trainer, breathing with humidified oxygen (ultrasound nebulizers), and adequate pain relief are indicated. All these activities are not mutually exclusive, but complementary. Bronchoscopy can provide significant assistance in clearing the airways of mucus and blood after injury.
CONCLUSION
Successful treatment and diagnostic tactics require joint work of teams from intensive care units, thoracic, cardiovascular and abdominal surgery, traumatology, as well as diagnostic departments. Carrying out adequate and timely therapy is the key to successful treatment of this category of victims.
How dangerous is a chest injury?
So, first of all, let's look at what types of chest injuries there are:
- damage to the chest skeleton (fractures of the ribs, sternum, collarbones, shoulder blades, vertebrae of the thoracic spine);
- damage to soft tissues and internal organs (skin and subcutaneous layers, lungs, trachea, bronchi, esophagus, diaphragm, heart, large main vessels, pericardium).
The external manifestations of various types of injuries will depend on the severity and nature of the injuries and concomitant pathology.
Damage to soft tissues - hematomas in the subcutaneous fat, muscle ruptures, intermuscular hematomas, etc. Such injuries usually do not cause serious complications, with the exception of aesthetic ones; recovery (resorption of hematomas, healing of superficial wounds, reduction of swelling) occurs within 7-10 days, in rare cases with extensive injuries up to 3 weeks.
Diagnostic features: in most uncomplicated cases, an examination by a traumatologist or surgeon is sufficient. Special techniques are used to eliminate “deeper” damage.
Injuries to the chest skeleton - the first place is occupied by rib fractures, which in turn can be divided into multiple and single, one-sided and bilateral, linear, splintered.
Diagnostic features: at the initial stage, it is necessary to perform an X-ray of the chest, and, if necessary, a spiral computed tomography to detail the displacement, the adherence of internal organs to fragments, to exclude pathology of internal organs, and to diagnose “hidden” fractures.
Fractures of the clavicle and scapula are accompanied by multidirectional displacements and local reactions.
Diagnostic features: first of all, radiography in standard settings, in special settings, and, if necessary, to detail the picture of the fracture - SCT (computed tomography).
Subpleural hematoma - occurs in the event of a fracture of the ribs or sternum and hemorrhage into the parietal pleura.
Diagnostic features: method of choice – SCT.
Lung damage is accompanied by ruptures of lung tissue and the occurrence of foci of contusion.
Diagnostic features: X-ray ruptures of the lungs are diagnosed based on the detected pneumothorax (air in the pleural cavity), pneumohemothorax (air and blood in the pleural cavity), hemothorax (blood in the pleural cavity), also using the diagnosis of subcutaneous, muscular or mediastinal emphysema.
Damage to the esophagus is rare and occurs in patients with combined trauma to the thoracic skeleton, contusion and rupture of the lungs, and mediastinal hematomas.
Features of diagnosis: when the wall of the esophagus ruptures, air penetrates through the defect into the tissues of the mediastinum, mediastinal emphysema develops - an indirect sign, 100% diagnosis is esophagoscopy.
Damage to the diaphragm is rare in practice, occurring predominantly on the left, against the background of a combined injury to the abdomen, chest, and fractures of the X-XII ribs. When the muscle fibers of the diaphragm are torn, displacement of the abdominal organs into the chest (for example, stomach, spleen, intestinal loops) may occur.
Diagnostic features: X-ray images can be used to determine the displacement of the abdominal organs into the chest, a change in the contour of the diaphragm.
In conclusion: traumatic injuries to the chest are extremely dangerous : while the patient appears well on the outside, there may be serious internal injuries that can lead to death, that is, in cases of an accident, a fall from a height, or serious blows to the chest, an in-person examination by a doctor is necessary, to exclude invisible but very important pathology.
Take care of yourself!
If you have questions, ask me here.
The article was prepared by specialists from the Department of Radiation Diagnostics at ACMD-MEDOX
Togliatti Medical Consilium 2015 No. 03-04 2015
TRADITIONAL AND MODERN PRINCIPLES OF DIAGNOSTICS CLOSED chest injuries (Clinical lecture)
AS Benyan
Summary
Examination of victims with closed chest trauma is a complex intellectual process, the success and effectiveness of which is based on the unconditional implementation of all diagnostic algorithms under conditions of limited time and the need for immediate elimination of life-threatening conditions.
Correct interpretation of clinical data determines the subsequent correct choice of the scope of laboratory and instrumental examination, which helps optimize the treatment of victims. Key words:
closed chest injury, pleural puncture, thoracoscopy, fibrobronchoscopy
Summary
Examination of patients with closed chest injury is a complex intellectual process, the success and effectiveness of which are based on the strict implementation of all diagnostic algorithms in a limited time and the need for simultaneous removal of life-threatening conditions.
The correct interpretation of clinical data makes the subsequent selection of the correct amount of laboratory and instrumental examination that helps to optimize treatment of victims. Keywords:
closed chest trauma, pleural puncture, thoracoscopy, bronchoscopy
Introduction.
In the era of industrial and information progress, the fact of the paradoxical influence of technological achievements on the social and health aspects of human life is of particular importance. On the one hand, the widespread and, at times, uncontrolled use of resources of various types of industry, leading to the occurrence of man-made disasters and consistently high traumatization of the population, both in local and on a larger scale. On the other hand, the growing share of innovative methods of high-precision diagnostics and specialized treatment forces healthcare professionals to balance between the negative and positive sides of the technological development of mankind [17, 31, 46]. Thus, approaching the question of modern possibilities for diagnosing chest trauma, it should be said that at present there is the most comprehensive and comprehensive range of diagnostic services, which makes it possible to identify almost all types of damage at the systemic, organ, tissue and cellular levels. However, in light of such broad diagnostic capabilities, it is also necessary to understand that these capabilities are often concentrated in a small number of multidisciplinary and specialized hospitals, and one of the main features of the organization of the diagnostic and treatment process for trauma is the frequent remoteness of victims from high-tech medical care resources. It is in these conditions that traditional methods of classical physical examination and publicly available diagnostic methods come first. The importance of observing generally accepted and mandatory principles for examining victims with chest trauma, as well as the reasonable inclusion of all available paraclinical services in the diagnostic process will be discussed in this work [4, 29, 44].
Features of diagnosis of closed chest injury
The chest contains organs responsible for the vital functions of blood circulation and respiration. Despite the protection of the internal organs by the musculoskeletal frame of the chest, they remain quite vulnerable to the effects of traumatic force, and any damage to them is associated with the risk of the rapid development of life-threatening conditions. Thus, the traditional perception of the concept of “trauma” as an urgent condition requiring immediate recovery measures is also complemented by the need for additional acceleration of therapeutic and diagnostic measures inherent in the destabilization of the respiratory and circulatory systems. This is where both directions of the vector of the diagnostic process for chest trauma originate. Firstly, the need for a quick diagnosis in a limited time environment. And secondly, given the severity of the condition of the victims and the presence of life-threatening conditions at the initial stage, it is more advisable to be guided by the principles of syndromic diagnosis and, accordingly, carry out syndromic therapy according to indications. According to this concept, an initial examination should be performed, measures should be taken to maintain vital functions, the patient's condition should be re-evaluated and treatment methods should be determined [8, 20, 50].
Physical examination of victims with closed chest trauma
The task of the initial examination of victims with any injury, and especially with chest trauma, is to determine the function of the vital organs and then take the necessary measures. Guided by the rule of resuscitation of victims "ABC", in which "A" - airway open (assessment of airway patency), "B" - breath for victim (assessment of the presence of external respiration), "C" - circulation his blood (assessment of the state of cardiovascular system), it is necessary to first determine the degree of damage and dysfunction of the airways, the presence and state of natural respiration, and indicators of cardiac activity and pulse [19, 34, 42]. Physical examination
should begin with the upper airway to identify damage or foreign body obstruction.
To detect damage to the larynx, examination of the oropharynx is necessary. In this case, you should pay attention to the patient’s voice, changes in which may be a manifestation of stridor breathing. Then the patient's breathing should be assessed (respiratory movements, respiratory rate and rhythm, cyanosis) to exclude hypoxia. The initial assessment of blood circulation includes determining the pulse (frequency and regularity) and studying peripheral blood flow (color and temperature of the skin). It is important to pay attention to the filling of the jugular veins (it will be reduced with hypovolemia and increased with cardiac tamponade or tension pneumothorax). An extremely important criterion for the presence of acute post-traumatic conditions is the degree of consciousness of the victim, which can vary from excitement to complete absence [8, 21]. If the victims do not have life-threatening conditions, the clinical examination should not differ from the standard one for surgical diseases and injuries, but the pace of the examination should correspond to the emergency nature of the patient’s condition. When collecting complaints, it is necessary to actively list all the classic signs of damage to the chest organs, as well as focus the patient’s attention on specific symptoms that are little known in the common environment. Most often, victims complain of chest pain, disturbances in the rhythm and depth of breathing, attacks of shortness of breath and suffocation, cough, hemoptysis, irregular heartbeats, difficulty performing active movements, and general weakness. There may be complaints about changes in phonation and the act of swallowing, the presence of signs of tissue emphysema in the form of changes in the configuration of various parts of the body. From the anamnesis it is necessary to establish the time and place of injury, the nature of the action of the traumatic agent, and the possible presence of combined mechanisms of injury. In addition, the doctor must determine the dynamics of the development of symptoms, the effectiveness of the first medical measures taken and other previous types of assistance [7,9,43]. Further examination
is a detailed visual examination of all areas of the victim’s body, regardless of the nature of the prevailing complaints.
Initially, you should pay attention to the patient’s position - patients often sit with their hands resting on a hard surface, thereby including additional respiratory muscles. Changes in skin color in victims with chest trauma are most often presented in the form of cyanosis (with hypoxia) or severe pallor (with bleeding). In the area of application of traumatic force, hemorrhagic impregnation of superficial tissues (skin, subcutaneous tissue) is often determined. If there is a violation of the integrity of the skin, it is necessary to study the location, shape of the wound and determine the direction of the wound channel. With severe trauma to the bone frame of the chest, changes in the shape and outline of the chest are often observed - asymmetry, edema, subcutaneous emphysema, retraction or bulging of the intercostal spaces, paradoxical respiratory movements [1, 8, 34]. Determination and measurement of respiratory rate and pulse, as well as arterial respiration are mandatory components of diagnosis in victims with chest trauma. The most common are different degrees of tachypnea and tachycardia, which indicates the tension of the protective compensatory forces of the patient’s body. The appearance of bradycardia or rare breathing, on the contrary, may indicate decompensation of basic vital functions. In addition, the assessment of these clinical data is included in all scales for assessing the severity of the condition of victims and helps to properly structure further treatment and tactical actions [34]. The following other medical actions, simultaneously with a visual examination, involve performing classical methods of physical examination. When palpating
the chest, it is necessary to determine the points of greatest pain, evaluate the presence of hematomas in soft tissues, tissue emphysema, pathological mobility of the ribs, sternum, and crepitus of fragments.
Vocal tremors, as a rule, are weakened in all intrapleural pathological post-traumatic conditions. Simultaneously with palpation, a test with dosed axial load can be performed to identify areas of rib fractures [8, 19]. Percussion
makes it possible to determine the presence of air and fluid in the pleural cavity, expansion and displacement of the mediastinum.
The appearance of pathological tones and changes in the normal boundaries of organs during percussion indicate the presence of intrapleural pathology. Thus, with pneumothorax there will be a tympanic (box) sound, the boundaries of the mediastinum are often shifted to the healthy side, but reverse displacement may also occur due to a decrease in the volume of the pleural cavity with long-term pneumothorax. Dullness of percussion sound most often occurs with hemothorax, post-traumatic pleurisy, and pulmonary atelectasis. Moreover, if, in the presence of fluid in the pleural cavity, the mediastinum is shifted to the healthy side, then with atelectasis there will sometimes be a sharp shift of the mediastinal structures towards the lesion. Changes during percussion are characteristic if the victim has pneumomediastinum (mediastinal emphysema) - a tympanic sound is noted in the neck and in the projection of the sternum, as well as the absence of cardiac dullness. It must be remembered that in order to objectify percussion sounds, it is always necessary to adhere to the principles of comparative percussion, that is, to carry out mandatory tapping on the undamaged side. In addition, percussion of the lungs is of little information in the presence of tissue emphysema or extensive soft tissue hematoma, since the data obtained will primarily indicate the condition of the chest wall [8,19,43]. Auscultation
, carried out after palpation and percussion, allows you to confirm the presence of changes in the intrathoracic organs, as well as obtain additional information based on the identification of pathological noises. In most cases, there is a weakening of vesicular respiration up to its complete absence. If there is fluid in the pleural cavity, you can hear the characteristic sounds of splashing and friction of the pleura. An indicative result of auscultation is the recognition of bowel sounds in the pleural cavity, which occurs when the diaphragm is damaged and translocation of intra-abdominal organs into the pleural cavity. Detailing data from auscultation of the lungs, identifying and assessing the type of wheezing in chest trauma is a rather complex process and is not accompanied by a large information load. It is important to detect fundamental pathological manifestations, the comparison of which with the clinical picture will serve as the main conclusion of the examination [8,19,34]. This also includes mandatory auscultation of the heart, neck and sternoclavicular region, and abdominal cavity. In case of any chest injury, special attention should be paid to inspection and objectification of the presence of possible damage to organs and systems adjacent to the chest. Because often, when exposed to one damaging, usually high-energy force, there are combinations of chest trauma with trauma to the neck organs, organs of the upper abdominal cavity, retroperitoneal space, and the upper extremity girdle [8,19,50]. The importance of a full and high-quality physical examination is especially obvious in victims who are in a serious and sometimes unconscious state, in victims in whom the use of complex diagnostic procedures is associated with a high risk of worsening the condition or is impossible for organizational and technical reasons. At the same time, it is necessary to emphasize such features of the diagnostic process as repeating some studies, in other words, assessing the objective status of damaged organs over time. In addition, after receiving the results of the laboratory and instrumental examination, it is necessary to return once again to the assessment of the physical examination data, so that a comparison of the available information contributes to making the most accurate syndromic and clinical diagnosis [17].
Classification of methods for diagnosing chest trauma
The traditional classification of diagnostic methods is based on the identification of known groups, each of which is based on certain properties of various physical phenomena. According to this concept, there are: a) methods of radiation diagnostics;
b) ultrasound diagnostic methods; c) electrographic methods; d) intraluminal and intracavitary endoscopy; e) laboratory diagnostics; f) other and additional methods. At the same time, in victims with chest trauma, and especially in the most severe category of patients, the distribution of diagnostic methods according to other criteria that characterize the other capabilities of each method seems quite relevant.
Thus, depending on the degree of invasiveness in relation to the victim’s body, all diagnostic methods can be divided into 2 groups: a) non-invasive diagnostic methods (radiation methods, ultrasound diagnostics);
b) invasive diagnostic methods (endoscopic methods, laboratory diagnostics, X-ray endosurgical methods, thoracoscopy) .
Such a division is justified from the point of view of causing additional trauma to an already obviously injured patient, the possible worsening of the patient’s condition during a particular study, and, accordingly, determining its feasibility and associated risks. In addition, in patients classified as “non-transportable” (victims with severe chest trauma, in a state of shock, requiring emergency surgical interventions), the issue of “mobility” of the diagnostic method is very important. In other words, depending on the capabilities of applying diagnostic instruments and devices to the patient, among the examination methods we can distinguish : a) “stationary” diagnostic methods - requiring delivery of the patient to the location of the diagnostic base (computed tomography, magnetic resonance imaging, x-ray endovascular diagnostics);
and
b) “mobile” diagnostic methods - instruments and devices that can be freely moved over any distance, as well as diagnostics based on the study of biomaterials taken from the patient (intraluminal endoscopy, ultrasound diagnostics, laboratory tests).
Finally, based on the fact that although most examination methods meet the main condition for their use - direct diagnosis, at the same time there are a number of techniques that combine both diagnostic and therapeutic capabilities.
For trauma victims, such a combination can significantly reduce the examination time, and at the same time directly assess the effectiveness of the treatment component. As a result, taking this factor into account, all examination methods can be divided into: a) purely diagnostic methods;
b) methods that combine the properties of diagnostic and therapeutic measures (pleural puncture, thoracoscopy, fibrobronchoscopy - diagnostic and sanitation). Summarizing the characteristics of the criteria for classifying diagnostic methods in victims with chest trauma, attention should be focused on the basic requirements for each examination method - fast, accurate diagnosis, if possible, not requiring additional clarification, with an optimal ratio of invasiveness and diagnostic value of the method, as well as the presence auxiliary therapeutic effect [2, 6, 25, 47].
Methods of instrumental diagnosis of closed chest injury
Historically, radiation methods have become the main ones in the diagnosis of pathology and trauma of the chest. Their role today is no less important. The leading method for diagnosing injuries to the chest organs is chest radiography
.
The standard research protocol includes taking pictures in frontal and lateral (if possible) projections, as well as polypositional fluoroscopy
, which allows assessing the status of organs in a dynamic mode.
X-ray allows you to identify damage to the bone structures of the chest (ribs, sternum, spine), diagnose pathological intrapleural syndromes - pneumothorax and hemothorax, and suspect damage to the lung, heart and mediastinal organs. In particular, bone damage is assessed by the presence of a fracture line, displacement of fragments, deformation of bone contours, and a decrease in the volume of the hemithorax; if the lung is damaged, pneumothorax, the presence of fluid in the pleural cavity, infiltrates in the parenchyma corresponding to the areas of bruises, pathological atelectasis, pneumomediastinum, tissue emphysema are visualized; intrapleural bleeding and hemothorax will correspond to darkening in the pleural cavity, a shift of the mediastinum to the healthy side; damage to the structures of the mediastinum is manifested by expansion of its borders, emphysema, smoothness of the contours of the heart; Trauma to the diaphragm will be indicated by the absence of its normal contour, elevation of the dome and the appearance of pathological shadows in the pleural cavity, corresponding to the abdominal organs; If the foreign bodies are X-ray positive, their presence and location are established. Interpretation of chest X-ray data forms the basis for some classifications of chest trauma. For example, the radiographic classification of hemothorax includes: small hemothorax - darkening in the pleural sinus, medium hemothorax - darkening up to the angle of the scapula (level VII intercostal space), large hemothorax - darkening above the angle of the scapula [5, 17]. The technical side of the radiographic method involves performing direct and lateral survey photographs with the obligatory capture of both halves of the chest from the diaphragmatic sinuses to the apexes of the lungs. To diagnose intrapleural injuries, images of normal stiffness are necessary; bone damage is better identified on images of increased rigidity in oblique projections. Dynamic x-ray examination is mandatory for all chest injuries. Fluoroscopy allows for differential diagnosis between different diseases and traumatic conditions that have a similar radiographic picture [10,31]. An important place in the X-ray examination of victims is occupied by contrast examination of the upper gastrointestinal tract
.
A publicly available and easy-to-use method allows in most cases to diagnose injuries to hollow organs (esophagus, stomach), rupture of the diaphragm with translocation of intra-abdominal organs into the pleural cavity [10, 30, 45]. The scientific basis for the X-ray examination method in diagnosing various types of chest trauma is specificity - 100%, sensitivity - 82%, diagnostic value of the method - 90%. Routine radiography is recommended for all patients with chest trauma, as it is a high-quality diagnostic method and allows for initial screening and the need for further research [27]. High-tech types of X-ray examination of patients are endosurgical angiography and spiral computed tomography
.
But if the first method has fairly narrow indications and is used only when there is a suspected injury to the thoracic aorta or its branches, then multislice computed tomography of the chest is by far the most highly accurate and sensitive diagnostic method. Performing computed tomography allows you to identify direct damage to organs, determine the exact topographic boundaries of damage zones, and assess the degree of post-traumatic changes. In the presence of lung injuries, areas of bruises, hemorrhagic impregnation, the presence of pneumatocele are visualized, the trachea and large bronchi are examined for rupture, and the presence of background pathology that can contribute to the formation of post-traumatic pathological conditions is assessed. The classification of the severity of pulmonary contusion is also based on data from computed tomography of the lungs: mild degree - contusion of less than 1/3 of the lung volume, moderate degree - contusion of up to 2/3 of the lung volume, severe degree - contusion of more than 2/3 of the lung volume. Computed tomography gives absolutely accurate answers to questions about the number and location of damage to bone structures - the presence of rib fractures, determination of fracture lines, degree of displacement of fragments, identification of the costal flap. With regard to hemothorax, this study determines the volume of blood poured into the pleural cavity, the ratio of liquid and coagulated components, and its encystation in hard-to-reach places. The method also has good visualization in the presence of pericardial effusion and hemopericardium. Considering that when performing a tomography, the organs of the upper floor of the abdominal cavity inevitably fall into the scanning area, information about their condition is also an auxiliary element in determining the extent of damage. A special type of multislice computed tomography is CT angiography
, which can be used to detect damage to large vascular structures of the mediastinum and heart [3,26,38,40,48].
The sensitivity of computed tomography is 98%, the specificity is 100%, and the diagnostic value of the method is 98%. All this allows us to consider it in case of chest trauma as the main diagnostic method with maximum resolution [13, 16, 35, 36, 49]. The use of magnetic resonance imaging in
chest trauma is limited by the laboriousness of the method and the lack of need for its frequent implementation due to the comparability of its sensitivity and diagnostic value with those of the computed tomography method.
Ultrasound examination
is also among the most valuable methods for examining victims with closed chest trauma.
With its help, the condition of the soft tissues of the chest, the presence of hematomas, and subcutaneous emphysema are assessed. Ultrasound examination is also quite informative in the diagnosis of rib fractures. There are works that talk about the use of ultrasound methods for diagnosing intrapulmonary hematomas and post-traumatic abscesses. However, the main point of application of ultrasound is to identify pathological contents in the pleural cavity, in particular hemothorax or pneumothorax. The advantage of the method is the ability not only to visualize liquid or air, but also to measure its volume. No less useful is ultrasound diagnosis of traumatic conditions in the pericardial cavity. Modern ultrasound with Doppler sonography
is the simplest and most accessible way to diagnose damage to the heart and great vessels of the mediastinum and the root of the lung.
Considering the portability of most ultrasonic devices, its implementation in dynamics does not present great organizational difficulties, and therefore should be widely used [14,24,33,41]. Endoscopic methods
occupy an important place in the diagnosis of chest injuries.
It should be remembered that a prerequisite for endoscopic examination is effective decompression of the pleural cavity in pneumothorax or the mediastinum in mediastinal emphysema. Fiberoptic bronchoscopy
is an objective method for diagnosing damage to the lung and respiratory tract.
Indications for fiberoptic bronchoscopy for chest trauma are: a) suspicion of damage to the trachea, bronchi and lung; b) pulmonary hemorrhage of any severity; c) atelectasis or hypoventilation of the lung; d) obstruction of the respiratory tract with blood, sputum, food masses; e) concomitant and background lung diseases; f) the need for sanitation of the tracheobronchial tree; g) difficult intubation. Fibroesophagoscopy
allows you to diagnose injuries and traumatic ruptures of the esophagus, as well as identify indirect signs of damage to other mediastinal organs [22].
The use of electrographic methods
in patients with chest trauma is, on the one hand, a mandatory routine nature, as is the case with
electrocardiography
, and on the other hand, it is indicated when diagnosing the consequences of injuries or predicting the outcomes of associated injuries (
electromyography
,
electroencephalography
) [17,20].
In addition to the listed purely diagnostic methods, instrumental diagnostic methods also include such surgical procedures as pleural puncture, thoracentesis with drainage of the pleural cavity, diagnostic pleuroscopy and thoracoscopy [8,19]. A diagnostic puncture
allows you to initially determine the nature of the contents of the pleural cavity, verify the correct topical diagnosis of hemothorax, and should also precede the mandatory drainage of the pleural cavity if it is present.
Drainage of the pleural cavity
allows you to evacuate the pathological contents, thereby assessing its nature and volume, and, most importantly, determining the presence or absence of ongoing bleeding.
The criteria for the latter are the Rouvilois-Gregoire test and a blood loss rate of more than 250 ml per hour after the immediate evacuation of the main volume of hemothorax [8,19]. Pleuroscopy and diagnostic operative thoracoscopy
are methods that maximally combine the properties of diagnostic and therapeutic methods. The main difference between these two methods is the type of anesthesia that accompanies these interventions. Pleuroscopy is performed using a flexible endoscope under local anesthesia, while thoracoscopy involves the use of rigid instrumentation and general anesthesia. Based on this, operative thoracoscopy has the greatest diagnostic capabilities, and accordingly it has become most widespread. The method allows not only to visualize almost all intrapleural injuries, but also to assess their degree, identify concomitant pathology, determine the possibilities of their immediate elimination, and also compare the information obtained with the data of the preoperative examination. The sensitivity of diagnostic thoracoscopy according to meta-analyses is 100%, specificity – 75%, accuracy – 95.8%. Injuries to the diaphragm are recognized by thoracoscopy in 98% of cases, hemothorax - in 99%, intrapericardial pathology - in 92% of cases. The frequency of diagnostic errors during thoracoscopy is less than 0.8% [11,15,18,23,28,30].
Methods for laboratory diagnosis of closed chest injury
Laboratory methods
in victims with chest trauma are important for obtaining information about the volume of blood loss, the nature and severity of gas exchange disorders, water and electrolyte balance disorders, and the state of the blood coagulation system.
The standard line of examination includes general and biochemical blood tests, general urine analysis, multimodal examination of bronchial secretions and pleural exudate (general analysis, cytological examination, bacteriological examination). A dynamic study of the hemoglobin level in the evacuated hemothorax also allows one to judge the presence of ongoing bleeding. To assess the degree of respiratory failure, a blood gas test is used. Determination of hemostasis values serves to predict the possible development of thrombotic and infectious complications. In severe cases with the development of traumatic disease and multiple organ failure, diagnostics of indicators of the systemic inflammatory response is carried out: lactate dehydrogenase, creatine phosphokinase, C-reactive protein, myoglobin [32, 39]. It should be especially emphasized that, regardless of the diagnostic capabilities available in a medical institution, an active dynamic examination of the victim
.
Only repeated instrumental and laboratory studies, carried out every 3–6 hours during the first day, and then at least once a day, make it possible to present a complete clinical picture of the injury and its consequences, to predict and prevent complications [12, 37]. Conclusion.
Examination of victims with closed chest trauma is a complex intellectual process, the success and effectiveness of which is based on the unconditional implementation of all diagnostic algorithms under conditions of limited time and the need for immediate elimination of life-threatening conditions. Correct interpretation of clinical data determines the subsequent correct choice of the scope of laboratory and instrumental examination, which together will optimize the entire further treatment program for victims.
For correspondence
Benyan Armen Sisakovich
, head of the surgical thoracic department of the Samara Regional Clinical Hospital named after. V.D. Seredavina", Candidate of Medical Sciences. Home address: 443066, Samara, st. Soviet Army 101, apt. 80. Work phone: 8(846)9562272, Home phone: 8(846)2255067. Email
Publications in the media
Chest injuries account for 10–12% of traumatic injuries. A quarter of chest injuries are severe injuries requiring emergency surgical intervention. In peacetime, closed injuries predominate over open ones and account for more than 90% of all chest injuries.
Classifications • The classification of chest injuries accepted in Russia divides them into closed wounds and penetrating wounds of the chest •• Closed injuries ••• Soft tissue injuries ••• Damage (fractures) of bones ••• Injuries to internal organs •• Open injuries (wounds) ••• non-penetrating: injuries (wounds) of soft tissues, injuries (open fractures) of bones ••• penetrating: injuries of the pleura and lungs with hemothorax and/or pneumothorax, heart injuries, injuries of the esophagus •• Combined injuries ••• thoracoabdominal injuries •• • other injuries (damage to the chest in combination with injuries to the head, spine, etc.) • Classification of the College of Traumatology of the American Society of Surgeons. Injuries to the chest are divided into emergency conditions that directly threaten the life of the victim, and potentially life-threatening conditions.
Immediately life- threatening injuries can be fatal within minutes. Despite the significant diversity in the nature and intensity of disorders, first of all they must include: disorders of external respiration (respiratory), circulatory disorders (circulatory), shock • Obstruction of the respiratory tract quickly leads to hypoxia, acidosis and cardiac arrest. It is necessary to immediately ensure and maintain patency of the airways: remove secretions, blood, foreign bodies, perform tracheal intubation, cricothyroidotomy or tracheostomy (as indicated) • Pneumothorax and hemothorax • Cardiac tamponade occurs with the rapid accumulation of blood in the pericardial cavity (under the cardiac membrane), accompanied compression of the heart, a decrease in its filling in diastole and a decrease in cardiac output •• Clinical manifestations: arterial hypotension, tachycardia, a sharp weakening of the apical impulse, expansion of the borders of the heart, significant expansion of the veins of the neck. Localization of the wound in the projection of the heart makes it possible to timely suspect injury to the pericardium and myocardium •• Treatment: sternotomy or left anterolateral thoracotomy and rapid decompression of the pericardium. A left-sided anterior thoracotomy and pericardiotomy are performed, and the blood that has spilled into the pericardial cavity is evacuated. The myocardial injury is sutured. The pericardium is also sutured with separate rare sutures to ensure free outflow of the contents of the pericardial cavity into the pleural cavity • Pathological mobility of the chest wall - see Rib fractures.
Potentially life - threatening injuries are usually fatal if not treated promptly. However, the condition of the patients allows an accurate diagnosis to be made within a few hours and the necessary treatment tactics to be developed.
• Ruptures of the trachea and main bronchi usually occur within 2 cm of the tracheal bifurcation. More often observed with blunt chest injuries. Injury to the trachea and bronchi rarely occurs in isolation, usually in combination with damage to other organs of the mediastinum and thoracic cavity • • Diagnosis is made clinically, by radiography or bronchoscopy. Characteristic signs include severe respiratory distress, pneumothorax, mediastinal emphysema, subcutaneous emphysema, pneumothorax, hemothorax and hemoptysis. Suspicion of rupture should arise in the following cases: ••• The collapsed lung could not be expanded after drainage of the pleural cavity (decompression failure) ••• A large volume of air continues to enter the pleural cavity ••• Massive mediastinal and subcutaneous emphysema in the early stages after injury ( 1–2 hours) • • Treatment: restoration of the wall of the trachea and bronchus. If it is not possible to restore the integrity of the ruptured main bronchus with the vessels intact, both ends of the bronchus should be tightly sutured and the patient should be transferred to a specialized thoracic surgery center.
• Aortic rupture usually occurs due to acute and blunt trauma to the chest or sudden stoppage of body movement (car accident). When large vessels of the chest are injured, less than half of the victims reach the hospital: there are few conditions for thrombus formation, the wound usually gapes, which is accompanied by heavy bleeding. As a result, about 2/3 of the victims die • • Clinical manifestations: hemorrhagic shock, localization of the injury in the upper half of the chest, intense pulsating hematoma, noise on auscultation above it, hemopneumothorax • • X-ray ••• Widening of the mediastinum ••• Blurred contour of the aortic arch ••• Downward displacement of the left main bronchus ••• Shadow at the apex of the lung ••• Deviation of the trachea to the right ••• Fluid (blood) in the left pleural cavity • • Aortography: confirm the diagnosis • • Treatment. Emergency thoracotomy, restoration of the integrity of the aorta by suturing the wound or interposition of the graft. Usually performed using a heart-lung machine.
• Injury to the diaphragm usually occurs with open and closed injuries to the chest and abdomen. In this case, the pleural and abdominal cavities communicate with each other •• The diagnosis is established using radiography, revealing the displacement of the stomach or colon into the chest. All penetrating wounds of the chest below the level of the VII rib are dangerous due to possible damage to the diaphragm. Therefore, if the clinical picture is unclear, these patients are indicated for diagnostic thoracoscopy •• Treatment. Immediate insertion of a nasogastric tube (if one has not previously been placed) prevents significant gastric dilatation, usually accompanied by severe, life-threatening respiratory distress. Then, ruptures in the diaphragm are urgently sutured (via transabdominal access) and at the same time the associated injuries to the abdominal organs are eliminated. The pleural cavity is drained.
• Damage to the esophagus most often occurs with penetrating wounds of the chest or with iatrogenic damage during esophagoscopy •• Clinical manifestations: immediate development of subcutaneous emphysema in the neck and rapidly progressing mediastinitis •• Diagnosis: X-ray examination of the esophagus with water-soluble contrast •• Treatment. Wide drainage of the mediastinum and suturing of the rupture should be performed as soon as possible. Access depends on the location of the rupture: either through the soft tissue of the neck or by performing a thoracotomy. The sutures are usually covered and reinforced with surrounding tissue (pleura, intercostal muscles).
• Cardiac contusion occurs with direct blows to the sternum. The severity of the manifestations of cardiac tissue contusion ranges from minor subendocardial or subpericardial petechiae to damage to the entire thickness of the myocardium • • Clinical picture: pain in the heart area, rarely relieved by validol, nitroglycerin, anxiety, fear, feeling of suffocation, weakness. The skin is earthy-gray in color, cold sweat, weak pulse, arrhythmic, tachycardia up to 140–150 per minute. On auscultation - dullness of tones, arrhythmia, arterial hypotension. On the ECG - decreased voltage, increased, flattened, biphasic or inverted T wave, deformation of the QRS complex • • Complications ••• Arrhythmias (including ventricular extrasystoles, supraventricular tachycardia and atrial fibrillation) ••• Ruptures of the myocardial walls ••• Ruptures of the interventricular septum • •• Left ventricular failure • • Diagnosis is based on the results of ECG and two-dimensional echocardiography • • Treatment: constant monitoring of cardiac activity and hemodynamics using monitoring equipment, treatment of arrhythmias with appropriate drugs, and with the development of cardiogenic shock - appropriate intensive care.
• Pulmonary contusion is the most common injury, accompanying extensive chest injuries in 30–75% of cases •• Causes. Closed injury causing intra-alveolar hemorrhages, edema and bronchiole obstruction •• Diagnosis is based on chest x-ray data (shading of lung tissue in the first hours after injury), gas composition in arterial blood and clinical signs of respiratory distress •• Treatment: restriction of fluid intake , oxygen inhalation, physiotherapeutic procedures, adequate pain relief (including epidural analgesia). If complications occur (pneumo- and hemothorax), emergency drainage of the chest cavity is performed.
• Mediastinal emphysema and subcutaneous emphysema •• Subcutaneous emphysema most often occurs with tension pneumothorax and rupture of the parietal pleura, which corresponds to a typical injury - a lung rupture with rib fractures or penetrating injury. With an intact parietal pleura, air enters the soft tissues of the chest from the mediastinum through the superior thoracic aperture. It is possible to develop extensive subcutaneous emphysema with a closed rupture of the bronchus or lung and preserved parietal pleura. It is necessary to distinguish between limited, widespread and total subcutaneous emphysema • • Mediastinal emphysema (pneumomediastinum) occurs when a bronchus (less commonly the trachea) ruptures while maintaining the integrity of the mediastinal pleura (air spreads through the paratracheal and mediastinal spaces). Another cause of pneumomediastinum is a complication of laparoscopy (when the insufflated gas, instead of the abdominal cavity, enters the preperitoneal tissue and then into the anterior mediastinum) ••• Clinical manifestations. Symmetrical swelling in the supraclavicular areas, quickly spreading to the neck and face. Hoarseness, extrapericardial cardiac tamponade. On palpation - a symptom of “crispy snow” (crepitus) ••• Treatment. With progressive mediastinal emphysema with dysfunction of the cardiovascular system and respiratory system, emergency suprasternal mediastinotomy is indicated: local anesthesia, procaine is sequentially injected into the skin, subcutaneous tissue and retrosternal space. A horizontal incision is made above the manubrium of the sternum and, sliding along the posterior wall of the sternum, carefully penetrates the mediastinum. Then drainage is installed and guiding sutures are applied.
• Chest compression (traumatic asphyxia). With prolonged and strong compression of the chest, almost complete or partial holding of breath occurs, entailing an increase in intrathoracic pressure with a sharp increase in pressure in the intrathoracic blood vessels. The outflow of venous blood through the system of the superior vena cava to the right side of the heart is disrupted •• Clinical picture: consciousness is often impaired, patients complain of chest pain, tinnitus, hoarseness, often aphonia, bleeding from the nose and ears is possible. The patient's appearance is characteristic: the skin of the head, neck, and upper half of the chest is bright red with multiple pinpoint hemorrhages spreading to the mucous membranes of the oral cavity, eardrums, conjunctiva and retina. In places where clothing fits tightly, there may be no bleeding on the skin. In severe cases - shortness of breath, weak rapid pulse, arrhythmias, arterial hypotension. On auscultation - a large number of moist rales, on the radiograph - various darkening of the pulmonary fields •• Treatment. For mild traumatic asphyxia - rest, cervical vagosympathetic novocaine blockade according to A.V. Vishnevsky, oxygen therapy. For severe traumatic asphyxia - mechanical ventilation, resuscitation, intensive care.
ICD-10 • S20 Superficial injury to the chest • S21 Open wound of the chest • S22 Fracture of the rib(s), sternum and thoracic spine • S23 Dislocation, sprain and damage to the joints and capsular ligament apparatus of the chest • S24 Trauma to nerves and spinal cord in the thoracic region • S25 Injury to the blood vessels of the thoracic region • S26 Injury to the heart • S27 Injury to other and unspecified organs of the thoracic cavity • S28 Crushing of the chest and traumatic amputation of part of the chest • S29 Other and unspecified injuries of the chest