Problem
The term "spinal cord injury" refers to damage to the spinal cord due to injury (such as a car accident) or disease or degeneration (such as cancer).
There is currently no reliable estimate of the worldwide prevalence of this phenomenon, but the global incidence rate is estimated to be 40–80 cases per million inhabitants per year. Up to 90% of these cases are caused by trauma, although the proportion of atraumatic spinal cord injuries appears to be constantly increasing. Symptoms of spinal cord injury depend on the severity of the injury and its location on the spinal cord. Symptoms may include partial or complete loss of sensory function or motor function of the upper limbs, lower limbs and/or body. The most serious spinal cord injuries affect the systems that regulate the gastrointestinal tract or bladder, breathing, heart rate and blood pressure. Most people with spinal cord injuries experience chronic pain.
Closed injuries of the spine and spinal cord
Clinical manifestations of spinal cord damage in spinal trauma. The clinical symptoms of a complicated spinal fracture are determined by a number of reasons, primarily the level and degree of damage to the spinal cord.
There are syndromes of complete and partial transverse spinal cord lesions.
In the syndrome of complete transverse lesion of the spinal cord down from the level of the lesion, all voluntary movements are absent, flaccid paralysis is observed, tendon and skin reflexes are not evoked, all types of sensitivity are absent, control over the functions of the pelvic organs is lost (involuntary urination, defecation disorders, priapism), and the autonomic system suffers. innervation (sweating and temperature regulation are impaired). Over time, flaccid muscle paralysis can be replaced by spasticity, hyperreflexia, and automatisms in the functions of the pelvic organs are often formed.
Features of the clinical manifestations of spinal cord injury depend on the level of damage. If the upper cervical part of the spinal cord is damaged (CI-IV at the level of the I–IV cervical vertebrae), tetraparesis or spastic tetraplegia develops with the loss of all types of sensitivity from the corresponding level. If there is concomitant damage to the brain stem, then bulbar disorders appear (dysphagia, aphonia, respiratory and cardiovascular disorders).
Damage to the cervical enlargement of the spinal cord (C5 – Th1 – at the level of 5-7 cervical vertebrae) leads to peripheral paraparesis of the upper extremities and spastic paraplegia of the lower extremities. Conduction disorders of all types of sensitivity occur below the level of the lesion. There may be radicular pain in the arms. Damage to the ciliospinal center causes the appearance of the Bernard-Horner symptom, decreased blood pressure, and slowed pulse.
Injury to the thoracic part of the spinal cord (ThII-XII at the level of the I-IX thoracic vertebrae) leads to lower spastic paraplegia with the absence of all types of sensitivity, loss of abdominal reflexes: upper (ThVII-ThVIII), middle (ThIX-ThX) and lower (ThXI- ТhXII).
If the lumbar thickening (LI–SII at the level of the X–XII thoracic and I lumbar vertebrae) is damaged, peripheral paralysis of the lower extremities occurs, anesthesia of the perineum and legs downward from the inguinal (pupart) ligament occurs, and the cremasteric reflex falls out.
In case of injury to the conus of the spinal cord (SIII-V at the level of the I–II lumbar vertebrae), there is saddle-shaped anesthesia in the perineal area.
Damage to the cauda equina is characterized by peripheral paralysis of the lower extremities, anesthesia of all types in the perineum and legs, and sharp radicular pain in them.
Spinal cord injuries at all levels are accompanied by disorders of urination, defecation and sexual function. With transverse damage to the spinal cord in the cervical and thoracic parts, dysfunction of the pelvic organs occurs, such as the “hyper-reflex neurogenic bladder” syndrome. At first after the injury, urinary retention occurs, which can last for a very long time (months). The sensitivity of the bladder is lost. Then, as the segmental apparatus of the spinal cord disinhibits, urinary retention is replaced by spinal automaticity of urination. With a hyperreflex bladder, involuntary urination occurs when there is a slight accumulation of urine in it. When the conus spinal cord and roots of the cauda equina are damaged, the segmental apparatus of the spinal cord suffers and the syndrome of “hyporeflex neurogenic bladder” develops. It is characterized by urinary retention with symptoms of paradoxical ischuria. Defecation disorders in the form of stool retention or fecal incontinence usually develop in parallel with urination disorders.
Damage to the spinal cord in any part is accompanied by pressure sores that occur in areas with impaired innervation, where bony protrusions are located under the soft tissues (sacrum, iliac crests, heels). Bedsores develop especially early and quickly with severe (transverse) damage to the spinal cord at the level of the cervical and thoracic regions. Bedsores quickly become infected and cause the development of sepsis.
When determining the level of spinal cord damage, the relative position of the vertebrae and spinal segments must be taken into account. It is easier to compare the location of the spinal cord segments with the spinous processes of the vertebrae (with the exception of the lower thoracic region). To determine the segment, add 2 to the vertebral number (so, at the level of the spinous process of the third thoracic vertebra the fifth thoracic segment will be located).
This pattern disappears in the lower thoracic and upper lumbar regions, where at the level ThXI-XII-LI there are 11 segments of the spinal cord (5 lumbar, 5 sacral and 1 coccygeal).
There are several syndromes of partial spinal cord damage.
Half-lesion syndrome of the spinal cord (Brown-Séquard syndrome) is paralysis of the limbs and impairment of deep types of sensitivity on the affected side with loss of pain and temperature sensitivity on the opposite side. It should be emphasized that this syndrome is rare in its “pure” form; its individual elements are usually identified.
Anterior spinal syndrome - bilateral paraplegia combined with decreased pain and temperature sensitivity. The reason for the development of this syndrome is a violation of blood flow in the anterior spinal artery, which is injured by a bone fragment or a prolapsed disc.
Central spinal cord syndrome (more often occurs with sudden hyperextension of the spine). It is characterized mainly by paresis of the arms, weakness in the legs is less pronounced, there are varying degrees of sensitivity disturbances below the level of the lesion, and urinary retention.
In some cases, mainly with trauma accompanied by sharp flexion of the spine, a syndrome of damage to the posterior cords of the spinal cord may develop - loss of deep types of sensitivity.
Damage to the spinal cord (especially when its diameter is completely damaged) is characterized by disturbances in the regulation of the functions of various internal organs: respiratory disorders with cervical damage, intestinal paresis, dysfunction of the pelvic organs, trophic disorders with the rapid development of bedsores.
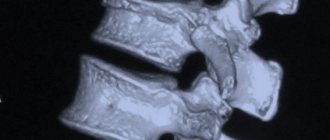
In the acute stage of injury, disturbances in cardiovascular activity and a drop in blood pressure are often observed. In case of a vertebral fracture, an external examination of the patient and identification of such changes as concomitant soft tissue damage, reflex muscle tension, sharp pain when pressing on the vertebrae, and finally, external deformation of the spine (for example, kyphosis with a compression fracture in the thoracic region) can be of some importance in recognizing it. ).
Spinal cord concussion. It is characterized by damage to the spinal cord of a functional type in the absence of obvious structural damage. Macro- and microscopically, swelling of the brain substance and its membranes, and single point hemorrhages are usually detected. Clinical manifestations are caused by neurodynamic changes and transient disturbances of hemo- and liquorodynamics. Short-term, mildly expressed paresis, paresthesia, sensory disturbances, and dysfunction of the pelvic organs are observed. The cerebrospinal fluid is not changed, the patency of the subarachnoid space is not impaired. Spinal cord concussions are rare. A much more common and serious injury is spinal cord contusion.
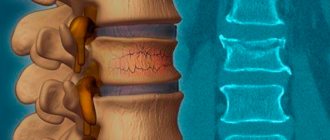
Spinal cord contusion. The most common type of lesion in closed and non-penetrating spinal cord injuries. A bruise occurs when a vertebra is fractured with its displacement, intervertebral disc prolapse, or vertebral subluxation. With a contusion of the spinal cord, structural changes always occur in the substance of the brain, roots, membranes, and vessels (focal necrosis, softening, hemorrhages). Damage to brain tissue is accompanied by spinal shock. The nature of motor and sensory disorders is determined by the location and extent of the injury. As a result of a contusion of the spinal cord, paralysis, disturbances in sensitivity, functions of the pelvic organs and autonomic functions develop. Trauma often leads to the appearance of not one, but several areas of injury. Secondary circulatory phenomena can cause the development of myelomalacia foci several hours or even days after injury. Spinal cord contusions are often accompanied by subarachnoid hemorrhage. In this case, an admixture of blood is detected in the cerebrospinal fluid. The patency of the subarachnoid space is usually not impaired.
Depending on the severity of the injury, restoration of impaired functions occurs within 3–8 weeks. However, with severe bruises with a complete anatomical break of the spinal cord, the lost functions are not restored.
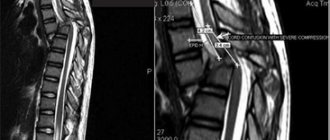
Spinal cord compression. Occurs when a vertebra is fractured with mixing of fragments or when there is a dislocation or herniation of an intervertebral disc. The clinical picture of spinal cord compression can occur immediately after injury or be dynamic (increasing with spinal movements) if it is unstable and there are moving bone fragments.
There is a so-called hyperextension injury of the cervical spine (whiplash injury) , which occurs in car accidents, diving, and falling from a height. The mechanism of this spinal cord injury is a sharp hyperextension of the neck, exceeding the anatomical and functional capabilities of this section and leading to a sharp narrowing of the spinal canal with the development of ischemia or compression of the spinal cord. Clinically, hyperextension injury is manifested by spinal cord lesion syndromes of varying severity - radicular, partial dysfunction of the spinal cord, complete transverse lesion, anterior spinal artery syndrome.
Hemorrhage in the spinal cord. Most often, hemorrhage occurs when blood vessels rupture in the area of the central canal and posterior horns at the level of the lumbar and cervical thickenings. Clinical manifestations of hematomyelia are caused by compression of the posterior horns of the spinal cord by effusion of blood, spreading to 3-4 segments. In accordance with this, segmental dissociated disturbances of sensitivity (temperature and pain) acutely occur, located on the body in the form of a jacket or half-jacket. When blood spreads to the area of the anterior horns, peripheral flaccid paresis with atrophy is detected. When the lateral horns are affected, vegetative-trophic disorders are observed. Very often, in the acute period, not only segmental disorders are observed, but also conduction sensitivity disorders, pyramidal symptoms due to pressure on the lateral cords of the spinal cord. With extensive hemorrhages, a picture of complete transverse lesion of the spinal cord develops. The cerebrospinal fluid may contain blood.
Hematomyelia is characterized by a regressive course. Neurological symptoms begin to decrease after 7–10 days. Recovery of impaired functions may be complete, but more often neurological disorders remain.
Hemorrhage into the spaces surrounding the spinal cord. It can be either epidural or subarachnoid. As a result of epidural hemorrhages (from the venous plexuses), an epidural hematoma is formed, which gradually compresses the spinal cord. Epidural hematomas are rare.
Clinical manifestations. Epidural hematomas are characterized by an asymptomatic period after injury. A few hours after it, radicular pain occurs with varying irradiation depending on the location of the hematoma. Then symptoms of transverse compression of the spinal cord appear and begin to increase.
The clinical picture of intrathecal (subarachnoid) hemorrhage in spinal cord injury is characterized by acute development of symptoms of irritation of the membranes and spinal roots. Intense pain in the back and limbs, stiffness of the neck muscles, and Kernig's and Brudzinski's symptoms appear. Very often, these symptoms are accompanied by paresis of the limbs, conduction disturbances of sensitivity and pelvic disorders due to damage or compression of the spinal cord by gushing blood. The diagnosis of hemorrhachis is verified by lumbar puncture: the cerebrospinal fluid is intensely stained with blood or xanthochromic. The course of hemorrhachis is regressive, and complete recovery often occurs. However, hemorrhage in the cauda equina area may be complicated by the development of adhesive or cystic arachnoiditis.
Mortality
The highest risk of mortality occurs during the first year after injury and remains high compared with the general population. People with spinal cord injury are 2 to 5 times more likely to die early.
The risk of mortality increases with the level and severity of injury and is largely determined by the availability of timely and high-quality medical care. Factors such as the method of transport to hospital after injury and the time elapsed before admission to hospital are also important.
Secondary conditions that can be prevented (for example, infections from untreated pressure ulcers) are no longer considered the leading causes of death in people with spinal cord injury in high-income countries, but these conditions still remain the leading causes of death in people with spinal cord injury , in low-income countries.
Health, economic and social consequences
Spinal cord injury is associated with a risk of developing secondary conditions that can lead to overall poor health and even life-threatening conditions, such as deep vein thrombosis, urinary tract infections, muscle spasms, osteoporosis, pressure ulcers, chronic pain, and airway complications. Prevention and treatment of these conditions requires emergency care, a system of rehabilitation services and ongoing provision of medical care.
Spinal cord injury may result in the individual requiring assistance from others. Often, orthopedic and rehabilitation equipment is needed to facilitate mobility, communication, personal care, or homework. It is estimated that 20-30% of people with spinal cord injury exhibit clinically significant symptoms of depression, which in turn has a negative impact on functioning and overall health.
Misperceptions, negative attitudes and physical barriers to basic mobility functions leave many people unable to fully participate in society. Children with spinal cord injury are likely to be less likely than their peers to start school and, once enrolled, less likely to succeed in school. Adults with spinal cord injury face similar barriers that prevent them from participating in economic life, as evidenced by their global unemployment rate, which is over 60%.
Current data does not allow an estimate of the costs associated with spinal cord injury at a global level, but it does provide a general picture:
- the level and severity of the injury has a significant impact on these costs—the higher the injury is located on the spinal cord (eg, tetraplegia versus paraplegia), the higher the costs;
- direct costs are highest in the first year immediately after spinal cord injury and then decline substantially over time;
- indirect costs, especially loss of sources of income, often exceed direct costs;
- most of these costs fall on the shoulders of the people who have suffered spinal cord injury;
- the costs associated with spinal cord injury are higher than those associated with comparable conditions such as dementia, multiple sclerosis and cerebral palsy.
Publications in the media
Spinal cord contusion (spinal cord contusion) is a variant of spinal cord injury, characterized by the occurrence in the spinal cord of reversible (functional) as well as irreversible (organic) changes in the form of foci of necrosis, crushing, hemorrhages, leading to partial damage or to a morphological interruption of the spinal cord. brain • Pathomorphological changes can be both primary - at the site of application of traumatic force, and secondary - due to circulatory disorders and cerebrospinal fluid circulation • Morphological break of the spinal cord can be anatomical (with divergence of ends) and axonal, when the integrity of the spinal cord is externally preserved, although the conductive its systems at the level of injury are destroyed • Complete anatomical interruption of the spinal cord occurs rarely • Spinal cord contusion is not classified according to severity. Depending on the depth of the lesion, neurological deficits of varying severity are observed.
Clinical picture • Phased course. Spinal cord contusion is accompanied by spinal shock (for more details, see Spinal cord injury), which masks the true picture of spinal cord damage. Only after resolution of the shock does persistent symptoms arise, reflecting the degree of damage to the spinal cord • Conduction disorder syndrome is the most characteristic manifestation of spinal cord contusion • • Complete conduction disorder syndrome ••• Impaired motor functions in the form of flaccid paralysis, areflexia ••• Disorders of all types of sensitivity conduction type (absence below the level of the lesion) ••• Autonomic symptoms: disorders of thermoregulation, trophism (dry skin, rapid formation of bedsores) ••• Gross dysfunction of the pelvic organs • • Partial conduction disorder syndrome is characterized by the same disorders as with complete its violation, but at the same time they reveal signs indicating partial preservation of the conductivity of the spinal cord (detection of disturbances in movements or sensitivity below the level of damage, expressed to one degree or another) • Complete transverse lesion of the spinal cord (morphological break) - syndrome of complete disruption of conduction in acute period and the automaticity of the distal part of the brain is below the level of the break in the later periods. Prolonged priapism and early trophic disorders indicate irreversible brain damage.
Diagnostics • During a neurological examination, it is necessary first of all to find out whether there is a picture of a complete transverse lesion of the spinal cord or only a partial loss of its functions • Liquor is an admixture of blood; liquor-dynamic tests sometimes reveal varying degrees of blockade of the subarachnoid space • X-ray of the spine in two projections, myelography • CT and MRI.
Treatment is conservative - see Spinal cord injury.
Complications • Ascending edema of the medulla oblongata • Visceral: the occurrence of ascending urinary tract infection, urogenic sepsis, bronchopneumonia • Formation of bedsores • Joint contractures • Deep vein thrombosis, thromboembolism of various locations.
Prognosis • Relatively unfavorable. A significant improvement in the condition cannot be expected, since regeneration with inaccurate comparison of axon ends is insignificant • If, with the clinical picture of a complete transverse lesion, at least minor signs of functional restoration do not appear in the next 48 hours, this indicates an organic rather than functional nature of the damage, which is considered a poor prognostic sign (irretrievable loss of functions) • Spinal roots, being peripheral neurons, are capable of regeneration, but only in cases where at least the outer shell of the root remains intact. After complete rupture, the regenerating axons of the central stump are separated from the distal stump, so fusion does not occur.
ICD-10 • S14 Nerve and spinal cord injury at the neck level • S24 Nerve and spinal cord injury at the thoracic level • S34 Nerve and lumbar spinal cord injury at the abdomen, low back and pelvis level
Prevention
The leading causes of spinal cord injury are car accidents, falls, and acts of violence (including suicide attempts). A significant proportion of traumatic spinal cord injuries are caused by work- or sports-related injuries. Effective measures are now available to prevent some of the leading causes of spinal cord injury, including improving roads, vehicles and behavior to avoid car accidents, window protection to prevent fall out, and policy measures that to prevent alcohol abuse and limit access to firearms to reduce violence.
Types of damage
The classification of spinal injuries takes into account:
- localization (division/divisions of the spinal column, combinations);
- skin condition
- type - isolated damage, open or penetrating
- character - stable/unstable (implies fixation)
- mechanism of injury—compression (compression), distraction (stretching), rotation (torsion), injury, consequence of an explosion
- presence of complications - involving the spinal cord, neurovascular bundles
Improving health care and problem solving
Many of the consequences associated with spinal cord injury are not due to the condition itself, but to inadequate levels of medical care and rehabilitation services, as well as physical environmental, social, and policy barriers.
Implementation of the UN Convention on the Rights of Persons with Disabilities (CRPD) requires appropriate action to address these gaps and challenges.
Key interventions to improve the survival, health, and social participation of people with spinal cord injury include the following:
- Timely and appropriate examination before admission to the hospital: prompt recognition of injury with suspected spinal cord injury, rapid assessment and implementation of first aid measures for the victim, including spinal immobilization.
- Emergency care (including surgery) appropriate to the type and severity of injury, degree of instability and presence of nerve compression, and in accordance with the wishes of the patient and family.
- Access to available health care, information materials and medical products (such as catheters) to reduce the risk of secondary conditions and improve quality of life.
- Access to qualified rehabilitation and mental health services to maximize recovery of function, independence, general well-being and inclusion in the community. Maintaining bladder and gastrointestinal function is extremely important.
- Access to appropriate assistive devices that can enable people to carry out activities of daily living that they would otherwise be unable to do, thereby reducing functional limitations and dependency. In low- and middle-income countries, only 5-15% of people have access to the assistive devices they need.
- Specialized knowledge and skills among health and rehabilitation professionals.
Necessary measures to ensure the right to education and economic participation include legislation, policies and programs that provide assistance in the following areas:
- creating physically accessible homes, schools, jobs, hospitals and transport;
- creating an education system for all;
- eliminating cases of discrimination at work and in education;
- rehabilitating skills to optimize employability;
- microfinance and other forms of self-employment benefits to support alternative forms of self-sufficiency;
- ensuring access to a social benefit system that does not act as a disincentive to return to work;
- a proper understanding of the problem of spinal cord injury and a positive attitude towards people who live with this condition.
WHO activities
WHO works across the spectrum, from primary prevention of traumatic and atraumatic causes of spinal cord injury, improving trauma care, strengthening health and rehabilitation services, and supporting the inclusion of people with spinal cord injury in society. WHO performs the following tasks:
- works on an interagency basis in partnership with national stakeholders across a variety of sectors (e.g. health, law enforcement, transport, education) to improve the prevention of spinal cord injuries, including from road traffic accidents, falls, acts of violence and nerve defects tubes;
- guides and supports Member States in raising awareness of disability issues and promotes the inclusion of disability as a component of national health policies and programmes;
- promotes the collection and dissemination of disability-related information and data;
- develops normative tools, including guidelines and good practices, to strengthen primary prevention (motor vehicle crashes, falls and violence), trauma care, health care, rehabilitation and support, and other care;
- builds appropriate capacity among health policymakers and service providers;
- promotes the expansion of rehabilitation work at the local level; And
- promotes strategies to ensure that persons with disabilities are well informed about their health conditions and that health care personnel support and protect the rights and dignity of persons with disabilities.