Greater trochanteric bursitis or trochanteric bursitis is an inflammation of the trochanteric bursa of the hip joint. While the term bursitis implies that there is an inflammatory component to the process, we must consider that 3 of the 4 elements of inflammation, which include redness, heat and swelling, are absent. The only cardinal sign of inflammation that is present is pain. Trochanteric bursitis is part of a broader terminological concept (bursitis of the hip joint), which includes 4 different types:
- Trochanteric bursitis.
- Bursitis of the iliopsoas muscle.
- Gluteal bursitis.
- Sciatic bursitis.
It is often used as a general term to describe pain around the greater trochanter of the femur. Trochanteric bursitis is often confused with pain syndrome of the greater trochanter of the femur. In fact, trochanteric bursitis is a component of greater trochanteric pain syndrome, which also includes other conditions that cause pain in the hip joint.
Clinically Relevant Anatomy
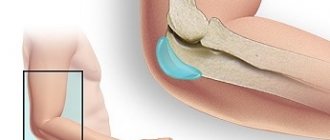
A bursa is a two-membrane bursa (or sac) filled with fluid located next to a joint. It forms a cushion to minimize friction between soft tissue and bone structures, and acts as a shock absorber during muscle and joint movement.
In the case of trochanteric bursitis, two bursae are usually involved:
- The gluteus medius bursa is located above the greater trochanter and under the insertion of the gluteus medius muscle.
- The gluteus maximus bursa is located between the greater trochanter and the attachments of the gluteus medius and gluteus maximus muscles.
What is the role of the joint capsule?
The joint capsule is usually located in those parts of the body where movement of layers of tissue occurs.
The joint capsule is a sliding layer of loose connective tissue and mucous membrane. Their task is to protect high friction areas from damage. Most often, inflammation of the joint capsule of the hip joint occurs on the surface of the large hill on the lateral side of the thigh. There is a thick tendon located on the hip bone here. Subsequent joint capsules are located deep in the thigh in front of the hip joint capsule, between the highly developed thigh muscles.
Epidemiology/Etiology
Inflammation of the bursa is a slow process that progresses over time. This type of bursitis most often occurs due to friction, overuse, direct trauma, or too much pressure.
There are two types of bursitis:
- Acute bursitis occurs due to injury or severe overload. After a few days, you may notice symptoms such as pain, swelling, and a feeling of warmth when you touch the affected area. The pain intensifies with movement in the joint.
- Chronic bursitis is one that is caused by overuse, too much pressure on structures, or extreme movements. Improper muscle tension can also be a cause of chronic bursitis. The main symptom that is always present is pain.
There are many predisposing factors that can cause trochanteric bursitis:
- Gender – Women are more often affected than men.
- Overweight/obesity.
- Trauma: For example, an injury to the greater trochanter can damage the bursa.
- Excessive use of the muscles around the bursa or the joint under the bursa.
- Incorrect positioning can lead to increased pressure on the bursa.
- Too much pressure on the bursa (caused by friction from the iliotibial band).
- Gluteus medius attachment dysfunction.
- Osteoarthritis of the hip joint.
- Lumbar spondylosis.
- Excessive or rapidly increased walking or running distance.
- Repetitive stress: for example, frequent training with too much weight or training in the wrong position.
- Bad shoes: leads to increased pressure on muscles, joints and bursa.
- Overpronation/extreme movements.
- Leg length difference.
- Iliotibial tract syndrome.
- Bacterial infection.
- Other inflammatory diseases.
- Hip endoprosthesis.
Symptoms of hip bursitis
The main symptom of hip inflammation is acute pain felt on the outer part of the thigh. From the moment inflammation begins, pain may intensify and its intensity may increase. But over time, the pain subsides - this is due to the spread of inflammation.
In addition to severe pain in the joint, other symptoms appear:
- a slight tumor forms in the area of the affected joint;
- swelling occurs;
- general body temperature rises, sometimes up to 40 °C;
- increased pain when bending or straightening the joint;
- weakness in the body and general malaise.
Often, with hip inflammation, the patient feels sharp pain on the outer thigh, which creates discomfort when lying down on the affected side. Sleeping problems may often occur.
Hip bursitis causes discomfort when walking up stairs, and in some cases the pain can become more intense. Acute pain occurs in the initial stages of the disease. When inflammation develops to a chronic form, the pain dulls and the symptoms become less noticeable.
Treatment
There are different approaches to treating trochanteric bursitis, depending on the presence of infection and the need for surgical treatment.
Aseptic trochanteric bursitis
- In most cases, trochanteric bursitis can be treated without surgery. If pain occurs as a result of overuse, it is recommended to reduce the activity or change the body mechanics that provoke symptoms.
- In addition, a stretching and strengthening program can help restore full range of motion to the hip joint (sometimes in combination with anti-inflammatory medications or the use of heat and cold to calm inflammation).
- If the above treatment fails to relieve symptoms, cortisone injections into the affected bursa may be necessary. It is important to understand that this reduces symptoms but solves the problem.
Septic trochanteric bursitis
- Infectious bursitis occurs, but is quite rare.
- Laboratory testing of the bursa fluid is necessary to evaluate which bacteria are causing the infection. Once this is known, antibiotic therapy can be prescribed.
Surgery
If conservative treatment is ineffective, surgery is indicated. Its purpose is to remove the inflamed bursa and bone spurs that have arisen on the greater trochanter. The gluteus maximus tendon is also treated. Some doctors prefer to remove the part of the tendon that rubs against the greater trochanter, while others prefer to surgically lengthen the tendon.
Physical therapy
There are several treatments that can be used to reduce pain and swelling in patients with trochanteric bursitis.
Physical therapy is the most common treatment option. When pain is the chief complaint, it is important to evaluate for associated disorders in order to more effectively treat the patient. Physical therapy can improve mobility, increase muscle strength, and normalize joint biomechanics. When these factors are corrected, pain usually decreases. Physical therapy also includes patient education and modification of daily and specific activities (eg, sports).
Friends, the seminar “Lower limbs, diagnosis and therapy, analysis of walking and running” will take place very soon. Find out more...
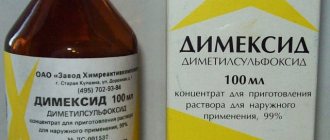
Working with pain can be carried out in different phases. The first phase is to manage pain and inflammation. Since pain is the leading reason for seeking medical help, we can use two common treatments to reduce pain: the use of ice and non-steroidal anti-inflammatory drugs. There are also other treatments that a physical therapist may use, such as electrotherapy, acupuncture, taping, soft tissue massage, and temporary use of aids to relieve weight on the affected side.
The second phase is to increase the patient's strength and restore normal range of motion. The physical therapist will also aim to normalize resting muscle length and tone, as well as proprioception, balance and gait through a controlled and carefully designed training program.
The next stage of rehabilitation is the restoration of all body functions. Many patients experience trochanteric bursitis due to their normal daily activities such as running, walking, etc. The goal of a physical therapist is to provide a patient with a specialized program to improve movement and reduce pain so that they can carry out their daily activities with less difficulty.
The final stage is preventing relapses. This may include an exercise program and orthopedic shoes to correct any biomechanical problems in the lower extremities. It also includes techniques for self-control. The ultimate goal is for the patient to safely return to their previous daily activities.
Conclusion
This article describes the causes and treatment of inflammation of the joint capsule in the hip joint.
The hip joint has several articular capsules. Here a description was given of the functions of the joint capsule and the causes of inflammation. Description does not apply to other joints. Latin name Bursitis. Damage to the joint capsule causes pain in the hip or groin. Symptoms may coincide with those of hip arthrosis (Coxarthrose). It is especially common among athletes and people with various musculoskeletal disorders. Arrival arrangements
1.General information
Trochanteritis (synonyms “trochanteric bursitis”, “peritrochanteritis”) is a particular variant of periarthritis, i.e. inflammation of the periarticular tissues, localized in the area where the femur meets the corresponding tendons (trochanter). Inflammation can spread to the synovial bursa and tendon-ligament apparatus.
As a separate, independent nosological unit, trochanteritis was isolated and described at the end of the 19th century by the prominent French surgeon Leon Clément LeFort (1890).
Mostly people of mature age suffer, with a slight predominance of women, which is due to morphological and histological gender differences.
A must read! Help with treatment and hospitalization!
Symptoms of pathology
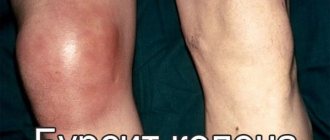
A specific sign of acute hip bursitis is the formation of painful, limited, elastic and round swelling. The skin over the lump turns red, swells slightly, and becomes hot to the touch. When pressing on this formation, fluid movement (fluctuation) is felt. In chronic bursitis, compaction is also present. But it is more limited; there is no swelling of the skin, hyperemia, or increased local temperature.
Bursitis of the trochanteric bursa
The trochanteric bursa is located at the site of attachment of the muscles (piriformis, gluteus medius and minimus) to the greater trochanter, a protrusion on the proximal epiphysis of the femur. Most often it is damaged during active and frequent sports training. The leading symptom of trochanteric bursitis is acute, piercing, burning pain. It intensifies when rotating the hip, climbing stairs, trying to squat, or lying down on the side of the damaged joint.
Iliopectineal bursitis
The iliopectineal synovial bursa is located on the inner femoral surface in the area of attachment of the tendons of the pectineal and iliopsoas muscles. Bursitis is manifested by severe or moderate pain, localized slightly below the inguinal ligaments. When lifting the leg bent at the knee, the intensity of the discomfort increases sharply. They radiate to neighboring areas of the body, radiating to the buttocks and lower back.
Ischiogluteal bursitis
With ischiogluteal bursitis, a rounded compaction is formed in the area of the ischial tuberosity to which the tendons of the biceps, semitendinosus, and semimembranosus muscles are attached. The skin over the swelling does not redden or swell due to the location of the synovial bursa deep in the soft tissues. The pain intensifies as the inflammatory process develops and bothers the person at rest and when moving. It occurs at night, especially when staying in one position for a long time.
Diagnostic methods
The primary diagnosis is made based on the patient’s complaints, the results of an external examination, and medical history. To confirm it, a sample of synovial fluid is taken using a puncture. Its study makes it possible to determine the nature of inflammation and establish the sensitivity of microorganisms to antibiotics.
If the development of specific infections (tuberculosis, syphilis, gonorrhea) is suspected, bacteriological studies are carried out. Since the symptoms of hip bursitis can mask arthritis and coxarthrosis, instrumental examinations of the joint are prescribed:
- radiography;
- MRI, CT, ultrasound.
They are usually carried out to differentiate bursitis from other diseases and to identify inflammation of the deep-lying synovial bursa.
Causes of the disease
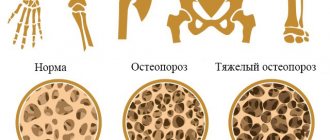
The main reason for the development of chronic bursitis of the hip joint is constant, long-term mechanical irritation. Most often it is caused by a person’s professional activity. The risk group includes people who spend most of the day on their feet or whose work involves frequent climbing of stairs. Factors that provoke the occurrence of bursitis include the following pathological conditions:
- systemic inflammatory diseases, including rheumatoid arthritis, scleroderma;
- gout, which occurs with the deposition of crystals of uric acid salts in the hip joint;
- osteoarthritis, in which soft tissue is injured by bone growths (osteophytes).
Acute infectious bursitis develops due to minor injuries - hematomas, abrasions, cuts, punctures. Pathogenic microorganisms penetrate from the surface of the skin into the synovial bursa, provoking the development of inflammation. Among the common causes of the disease, doctors also identify bedsores, osteomyelitis, carbuncles, and boils.