What is vertebrogenic cervicalgia?
The term "cervicalgia" means pain in the neck , and the word "vertebrogenic" indicates a connection with the spine. In terms of duration, this syndrome can be acute or chronic.
Information for specialists: according to the International Classification of Diseases, vertebrogenic cervicalgia is recorded with code M 54.2. The diagnosis must include the severity of symptoms, stage of the disease and treatment regimen. It is also advisable to indicate changes in the spine (spondylopathy or osteochondrosis).
The nature of pain during cervicalgia depends on the causes of its occurrence.
Pain of vertebrogenic nature in the cervical spine is divided:
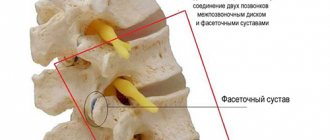
| For spondylogenic or vertebral cervicalgia: | For discogenic or true cervicalgia: |
| In this case, the affected bone tissue irritates the nerves, which causes pain and tonic spasms of the neck muscles. Usually the cause is an infectious process, neoplasms or osteoporosis. | This is a consequence of the destruction of the intervertebral disc. The disease is fraught with pinching of nerve endings and loss of elasticity of the cartilage layer. |
According to the manifestations of the course, they distinguish:
- Vertebrogenic cervicalgia in acute form . It is characterized by severe pain and severe accompanying symptoms. Usually a complication of dorsopathies and injuries. In general, symptoms last about 10 days
- Chronic . With this type of vertebrogenic cervicalgia, there is constant mild pain that lasts for over 3 months. The triggering mechanism is any tumors, indolent infections and pathologies affecting the carotid artery.
Depending on the location, the disease occurs in the following forms:
- Cervicobrachialgia. The vessels of the hands are affected, which causes loss of sensation in these limbs.
- Cervicocranialgia. The pathology contains negative changes in blood vessels, which is dangerous due to the deterioration of local blood flow.
In the international classification ICD-10, the disease is coded M54.2.
Read also
Schmorl's hernia
When a person undergoes magnetic resonance imaging of the spine for the first time and sees the phrase “Schmorl’s hernia” in the conclusion, he is naturally overcome by a feeling of anxiety.
After all, according to the patient, the terms... Read more
Rotational subluxation of the C1 vertebra
Dislocation or subluxation of a vertebra is a partial or complete disruption of the shape of the connecting articular surfaces of two adjacent vertebrae, and the overlying ones are considered dislocated. The reason for the rotational...
More details
Osteoporosis
Systemic bone disease associated with metabolic disorders. With osteoporosis, a decrease in bone mass occurs, a violation of the internal structure of the bone, its frame, as a result of which the bone becomes...
More details
Osteochondrosis
Osteochondrosis is a disease of the spine in which intervertebral discs and cartilage are damaged. This disease is very common; statistics show that osteochondrosis occurs all over the world...
More details
Disc herniation and back pain
A herniated disc is a truly dangerous and complex disease of the musculoskeletal system, which today is one of the most severe and at the same time very common...
More details
Causes of the disease
Vertebrogenic cervicalgia is a fairly common disease. There are a large number of factors that provoke this problem.
The main reasons are:
- Excessive physical activity.
- Prolonged uncomfortable position.
- Inactive lifestyle.
- Sedentary work at the computer.
- Depression and stress.
- Poor food.
- Diseases of the cervical spine.
- Metabolic disorder.
- Mental disorders.
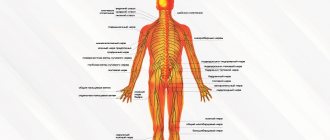
It must be taken into account that a lot of nerve endings and blood vessels pass through the neck . Therefore, all problems in the cervical spine result in acute pain, and sometimes a malfunction of the internal organs.
Complications of previous diseases may also be the cause.:
- Osteoporosis changes bone tissue.
- Rheumatoid arthritis affects the joints.
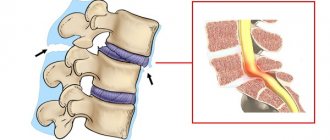
- Intervertebral hernia destroys the structure of the vertebrae.
- Spondylosis changes all structures of the spine.
As a rule, the causes of neck pain are degenerative changes in the cartilage of the spine
Pain in vertebrogenic cervicalgia is often caused by a functional disorder of the cervical vertebrae and concomitant pathologies.
Video: “Neck pain due to osteochondrosis: what to do?”
Possible consequences
Left untreated, it can lead to serious problems with brain function. This is explained by the fact that damaged vertebrae in the cervical region impair blood supply to the head.
Naturally, arterial stenosis causes the following problems:
- Excruciating headaches.
- Frequent fainting.
- Coordination of movements is impaired.
- Can paralyze limbs.
To avoid complications, treatment should be started in a timely manner.
Treatment of cervicalgia (neck pain)
Neck pain (cervicalgia)
- a very common complaint. Almost everyone has encountered this problem in their life. Pain in this localization is often short-lived and can go away even without treatment. However, cervicalgia can occur with a not always favorable outcome.
The neck is a very functionally significant area of the human body. Here, in a small area, many structures that are extremely important for life are collected: the spine, large blood vessels, nerve plexuses, autonomic centers. Therefore, even small problems in this area can affect your health and overall well-being.
The most common cause of cervicalgia is osteochondrosis and accompanying changes in the surrounding tissues: bone growths, calcification of ligaments, tension of various muscle groups in the neck and shoulders.
Factors that provoke the appearance of these pains may be prolonged static tension, sudden movements of the head, hypothermia (for example, due to the operation of an air conditioner).
However, neck pain can also be caused by other diseases and conditions, often accompanied by additional symptoms. These could be herniated discs in the cervical spine, trauma, tumors, neuroinfections, retropharyngeal abscess, mental stress and many other diseases.
To make an accurate diagnosis, it is necessary to undergo examination by a neurologist; in addition, additional examinations may be required:
- X-ray of the cervical spine with functional tests;
- MRI or CT scan of the cervical spine;
- ultrasound examination of brachiocephalic vessels;
- if necessary, consultation of related specialists.
The ROSA Clinic has a full range of necessary techniques and equipment to help with cervicalgia:
- To treat neck pain, medications, physiotherapeutic techniques, massage, exercise therapy, biofeedback therapy and other areas are used.
- To relieve pain associated with osteochondrosis of the cervical spine, non-steroidal anti-inflammatory drugs, combined analgesics, muscle relaxants, vasoactive and neurometabolic drugs can be used, as well as therapeutic blockades. According to indications, non-drug methods of influence are used: physiotherapy, manual therapy, massage, physical therapy.
- In case of severe manifestations and intense pain that are not amenable to conservative treatment methods, surgical treatment of degenerative changes in the spine is possible.
- For different causes of pain, different therapeutic approaches are used.
It is impossible to independently conduct an adequate examination and determine what is causing the pain.
!
Unfortunately, there are also cases when, due to improper treatment, pain transforms into chronic pain, or additional symptoms appear. This requires much more time and effort in the future to get rid of the entire complex of developed clinical manifestations.
Symptoms
The main manifestation of this disease is pain . Cervicalgia is accompanied by a lot of symptoms, but muscular-tonic syndrome is more often observed. In this case, the neck muscles become denser, and if you press on them, the pain intensifies.
Other symptoms include:
- The movement of the head is accompanied by a specific crunching sound.
- Throbbing headache, as well as dizziness.
- Restricted neck mobility.
- When you tilt your head back, fainting occurs.
- Partial loss of vision and hearing.
- The pain spreads to one of the arms and shoulder.
- The gait becomes unsteady.
- The upper limbs become weak.
- Tingling, as well as numbness of the face, hands and back of the head.
- Nausea, but no vomiting.
- When coughing or sneezing, the pain worsens.
Such symptoms are typical for any person, regardless of gender and age . In chronic cervicalgia, the symptoms are less pronounced, in contrast to the acute disease. In case of hypothermia or spinal injury, the pain is intense and severely hinders movement. When the disease occurs against the background of a concomitant disease, the pain is usually mild.
Video: “All causes of neck pain”
Treatment
Did you know that...
Next fact
Therapy is prescribed after a thorough examination. It should be noted that some drugs and physical procedures have strict contraindications. The prognosis for recovery is very favorable.
Drugs
To eliminate neck pain, a complex of several groups of drugs is prescribed. Painkillers with an anti-inflammatory effect : Celebrex, Xefocam, Ibuprofen. Medicines are used in the form of tablets, injections and ointments.
In the hospital, epidural blocks and botulinum toxin is injected into the muscles. If there is severe pain, they resort to novocaine blockades. Lidocaine is sometimes used. In case of acute pain syndrome, hormonal drugs (glucocorticosteroids) are sometimes prescribed, which have a powerful anti-inflammatory effect.
To tone blood vessels and improve microcirculation, Sermion and Trental are prescribed. Treatment is not complete without muscle relaxants , which relieve muscle spasms and reduce pain.
In the presence of osteoporosis , agents are used that activate bone tissue regeneration - fluorides and anabolic steroids. Drugs that prevent bone destruction are also needed - Myocalcic, estrogens.
Sometimes there is a need to take antidepressants: Sertraline, Diazepam.
Physiotherapy
- Electrophoresis.
- Ultraviolet irradiation.
- Electroneurostimulation.
- Diodynamic currents.
- Balneotherapy.
- Electroacupuncture.
Surgical
Any surgery in the neck area is quite risky due to the increased concentration of blood vessels and nerves in this area.
Indications for surgical intervention are considered:
- Acute damage, when damage to internal organs is noted.
- Increasing paresis with the threat of necrosis of nerve endings. In this case, the pain syndrome decreases, but weakness increases
The decision to carry out an operation must be motivated and soberly balanced.
Exercise therapy and massage
For vertebrogenic pathology, therapeutic exercises are necessary, which contain a complex of movements with muscle tension. The purpose of exercise is to correct muscle dysregulation .
The special complex has a common core of physical exercises that restore the motor pattern. They also promote post-isometric relaxation, stretch muscles and activate self-mobilization of the spine.
The exercises of the complex are treated with certain movements that are aimed at correcting changes in certain muscle groups of the spine.
It should be noted that exercise therapy is usually used for prevention or during remission to prevent exacerbation.
Basic exercises:
- Position sitting on a chair. The back is straight, arms are lowered. About 15 head tilts are done in different directions.
- The starting position is the same. Tilt your head back and hold for a few seconds. The movement is repeated up to 10 times.
- In a sitting position, raise your shoulders up as much as possible with a slight delay.
- Slowly rotate your head with a gradual increase in amplitude.
Such exercises can be done at any time and in any conditions. They are especially recommended for people leading a sedentary lifestyle.
Self-massage is very useful for this disease. It helps reduce pain and relieve vascular spasm.
Method of performing movements:
- Lightly stroking the head from the crown to the back of the head.
- Stroking the lateral cervical regions with fingertips. Be sure to do it from top to bottom and on both sides at the same time.
- Lightly massage the shoulders with your palms.
- Rubbing and kneading the trapezius muscle of the neck to the shoulder.
- Dashed movements in the direction of the spinous process of the 7th cervical vertebra.
- Stroking the back of the head, neck area and shoulder girdles.
At the moment of exposure to painful areas, pain, warmth and a feeling of stinging may occur. The main thing is to avoid severe pain and monitor the sensations. It is better to master self-massage with the help of a vertebrologist.
Therapy at home
At home, you can only reduce the symptoms of cervicalgia. You can use some folk remedies on your own, which are quite effective and time-tested.
The most popular of them : baths with certain herbal infusions, rubbing with a decoction of barberry root.
These 2 methods will not harm, but will not eliminate the cause of the disease. The most important thing is that they will relieve neck discomfort. Herbal baths warm up and reduce pain. Rubbing relaxes the cervical region, as the components of barberry have a gentle effect.
Naturally, if symptoms of a pinched nerve ending in the neck appear, you should immediately apply an analgesic ointment to the painful area. You can take a Diclofenac or Ibuprofen tablet.
It is imperative to exclude drafts and limit neck movements . Wrapping your neck in a woolen cloth will help reduce discomfort.
As for nutrition, there are no special diets for this syndrome.
Cervicalgia
Treatment of cervicalgia in Rostov-on-Don
The doctors at our center have many years of experience in treating dorsopathies of various origins. Cervicalgia
is a leading symptom of pathological processes in the cervical spine, neck pain that occurs with physical stress or awkward movement, turning the head. It can radiate to the back of the head (cervicocranialgia) or the space between the shoulder blades, shoulder, arm (cervicobrachialgia).
According to the nature of the flow:
• acute – the pain is sudden and pronounced and passes quickly;
• chronic – develops gradually, is of an unexpressed nature, occurs periodically and lasts a long time. By origin:
• vertebrogenic – associated with injuries and diseases of the spine. • spondylogenic cervicalgia - due to damage to the bones of the spine, for example, when bone growths put pressure on the spinal nerve; • discogenic cervicalgia, which occurs due to pathology in the intervertebral discs; pain is caused by their deformation. • nonvertebrogenic – associated with diseases and injuries of soft tissues (muscles, ligaments, nerves).
We must remember
! – Cervicalgia is a serious symptom that cannot be ignored. It is necessary to find the cause as quickly as possible. Particularly noteworthy is the combination of cervicalgia with headache, vomiting, rash, fever, photophobia, which may be a sign of a serious disease - meningitis! If you suspect, consult a doctor immediately!
| Where to begin? Since cervicalgia can be a consequence of various life-threatening pathologies, for an accurate diagnosis, and most importantly, to identify the causes and select the correct treatment, it is necessary to urgently consult a general practitioner, orthopedic traumatologist, neurologist, or vertebrologist. | What research may be needed? Instrumental: • X-ray • MRI • Computed tomography • Ultrasound Laboratory: • clinical blood test; • general urine analysis |
Causes:
• osteochondrosis of the cervical spine, osteophytes, degenerative changes in the vertebrae, hernia, protrusion of the cervical spine, • incorrect posture, stereotypical posture • hereditary diseases • developmental anomalies (nonfusion of the arch, tropism of the articular processes, etc.), causing instability of the spine; • rheumatoid lesions (especially with widespread osteochondrosis); • autoimmune disorders (appearance of autoantibodies in intervertebral discs during collagenosis); • tumors • infectious diseases (meningitis, encephalitis).
Provoking factors:
• sudden turn of the head • intoxication of the body • excess weight • excessive physical activity • intense sports • hypothermia • stress
Treatment:
Obviously, the diagnosis and treatment of cervicalgia requires a differentiated approach and joint efforts of both specialists in different fields - a general practitioner, neurologist, orthopedic traumatologist, vertebrologist, algologist, nutritionist, rehabilitation specialist, physiotherapist, and the patient himself.
Treatment of cervicalgia
- a painful pathological condition that significantly reduces the patient’s quality of life, in fact, is part of the complex therapy of the pathology that caused the corresponding symptoms and consists of eliminating pain and dysfunction of the spinal roots, relieving reflex muscle spasms, preventing the progress of dystrophic changes in the structures of the cervical spine .
It consists of non-medicinal, medicinal and surgical. Non-drug therapy for cervicalgia is a prerequisite for achieving stable remission of the disease.
Lifestyle correction:
• limitation of load, • exclusion of thermal procedures and massage during an exacerbation period • adherence to a special orthopedic regimen aimed at unloading the cervical spine • traction • orthosis (bandage) • nutrition correction (normalization of BMI, limiting foods that increase swelling, reducing salt) • refusal from smoking and alcohol abuse
Physiotherapy:
• scenar therapy • laser therapy • magnetic therapy • electrophoresis • phonophoresis • manual therapy • shock wave therapy • exercise therapy under the supervision of a physician
Sanatorium-resort treatment without exacerbation:
• radon baths, • hydrogen sulfide baths, • pine-salt baths.
Drug therapy
During an exacerbation, conservative treatment is aimed at reducing pain: therapeutic paravertebral blockades with glucocorticosteroids, lidocaine, novocaine; analgesics; NSAIDs; decongestant therapy; muscle relaxants; sedatives. Outside of exacerbation, therapy is aimed at improving the nutrition of the intervertebral discs and adjacent tissues - vitamin therapy, venotonics, correctors of cartilage tissue metabolism.
Surgery:
In severe cases, when conservative treatment is ineffective, the duration of the disease leading to disability, and verification of compression syndrome, surgical treatment - vertebroplasty - is indicated. This is a serious surgical intervention that requires the combined efforts of a surgeon, vertebrologist, neurosurgeon, and traumatologist.
Our clinic specializes in problems related to diseases of the musculoskeletal system. The doctors working in our center have many years of experience in treating joints, both surgically and, mainly, non-operatively. We will restore health to your joints.