Gynecology recognizes cervical dysplasia as non-invasive changes in the cervix in the transition zone of the single-layer columnar epithelium of the cervical canal into the multilayered squamous epithelium of the vaginal part of the cervix, often occurring after infection with HPV and HSV type 2. Moreover, cervical intraepithelial neoplasia (CIN), as cervical dysplasia is also called, implies processes of structural and cellular atypia (impaired cell differentiation) with a violation of the layering of the epithelium without involving the basement membrane.
These atypical changes refer to precancerous processes, in which the index of malignancy (oncological transformation) can reach 50%. In the early stages of their development, dysplastic changes are reversible, so gynecologists consider their timely detection and elimination to be a reliable way to prevent the risk of cervical cancer.
ICD-10 code N87 Cervical dysplasia.
General information
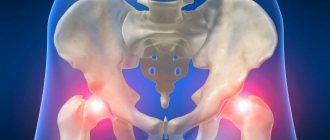
Connective tissue dysplasia in the body often manifests itself as pathology of the musculoskeletal system, including pathology of large (hip and knee) joints in the form of knee dysplasia and hip dysplasia.
Congenital hip dislocation (synonymous with congenital hip dysplasia) is a severe malformation of the musculoskeletal system and occupies one of the leading places among all congenital joint diseases. According to the literature, various degrees of underdevelopment of the hip joint (dysplasia) occur in 0.5-5% of newborns. Instability of the hip joint, subluxation/dislocation of the hip of dysplastic origin in children tends to rapidly progress and is the leading cause of the development of dysplastic deforming coxarthrosis already in adolescence. In the absence of adequate treatment, progressive trophic/functional disorders in the pelvic joint (JJ) lead to secondary severe disorders of the joint structures, which causes dysfunction of the support of the limb and its movement, disturbances in the physiological position of the pelvis, curvature of the spine and the subsequent development of deforming coxarthrosis and osteochondrosis , which are the leading cause of disability in adults.
ICD-10 code for hip dysplasia: Q65.0; Q65.1; Q65.2; Q65.3; Q65.4; Q65.5; Q65.6; Q65.9. Hip dysplasia in children is characterized by underdevelopment of almost all elements of the hip joint (bones, muscles, joint capsule, ligaments, vessels, nerves) and altered spatial relationships of the acetabulum and femoral head. In general, according to the literature, various degrees of underdevelopment of the hip joint (dysplasia) occur in 0.5-5% of newborns. At the same time, dysplastic changes in the hip joints are detected on both sides in 25% of cases. Left-sided lesions are more common (1:1.5) than right-sided lesions. TS pathologies are statistically significantly more common in girls (1:3). Moreover, girls experience more severe degrees of joint development delay, i.e. this pathology can be considered gender-related.
Features of the anatomy of the hip joint with dysplasia
The hip joint performs not only the physiological function of multi-axis movement. Its peculiarity (in combination with the function of the spine) is the formation of correct human posture, which is due to its anatomical structure (Fig. below) - a combination of the spherical head of the femur and the acetabulum, which form an extremely stable joint with the help of the ligamentous-muscular apparatus.
At the same time, in a newborn child, even normally, the structure of the hip joint is characterized by immaturity (not fully formed structure), excessive elasticity of the joint ligaments, which manifests itself:
- shallow flattened acetabulum;
- discrepancy between the size of the femoral head relative to the size of the acetabulum;
- insufficient density of the joint capsule;
- poor development of pelvic muscle tissue (gluteus muscle).
Essentially, the femoral head in infants is held in the acetabulum only by the round ligament, joint capsule and acetabular labrum. In addition, the predominant part of the joint elements at birth is cartilaginous, and the process of ossification and bone growth actively continues from 1 to 3 years. , the ossification of the femoral neck mainly increases , preserving the cartilaginous structure only in its upper part. During the same period, the highest growth rates of the acetabulum are observed. Normally, the growth of the femoral head and acetabulum occurs synchronously.
With hip dysplasia in newborns, the articular cavity and the head/neck of the femur are changed, but the ratio of the articular surfaces is still normal. It is the severity of anatomical defects of the joint, which are a consequence of tissue segmental inferiority, that determines the degree of dysplasia. Congenital hip dysplasia manifests itself in three forms, which gradually transform into one another (pictures below):
- Unstable hip (pre-dislocation) - characterized by joint instability due to connective tissue dysplasia. Its anatomical manifestation is the periodic displacement of the femoral head inside the articular cavity. Those. the head of the femur does not move beyond the acetabulum. At the same time, dislocation and reduction are carried out easily.
- Femoral subluxation - the articular surface of the femoral head is partially displaced outward and upward relative to the acetabulum, but does not extend beyond the limbus. At the same time, the contact between these elements of the joint is preserved. The round ligament and capsule are stretched, and the limbus moves upward, losing its support function, which allows the femoral head to move upward and partially to the sides.
- Hip dislocation - the head of the femur moves even higher and extends beyond the acetabulum. In this case, the contact of the femoral head with the glenoid cavity is completely lost. The limbus is displaced downwards, the ligaments and joint capsule are stretched. Dislocation is the most common form of damage to the hip joint (about 70%).
In the absence of treatment/or its ineffectiveness, the acetabulum gradually fills with connective fatty tissue, which complicates or makes the procedure of reducing the joint difficult or impossible.
Early detection of hip joint instability and timely initiation of treatment are of great importance, since as the child grows, the disease progresses, which significantly disrupts the biomechanics of the lower extremities and requires corrective surgical interventions aimed at stabilizing the joint, which significantly reduces the quality of life.
Causes of the disease
The causes of the disease have not yet been fully elucidated.
A number of provoking factors and features can be identified.
- Hereditary predisposition
- national traditions of tight swaddling,
- breech presentation,
- taking medications during pregnancy,
- premature birth,
- heavy baby weight
- girls are more predisposed
- the left joint suffers more often,
- bad ecology.
Symptoms
The newborn must be examined by an orthopedist while still in the maternity hospital. Warning symptoms:
- asymmetry of the inguinal, popliteal and gluteal skin folds,
- knees are at different heights,
- legs move apart differently (limited movement),
- a characteristic “click” during slow movement of the legs in both directions.
Stages of dysplasia
Depends on the nature and degree of joint disorders.
- Physiological immaturity (underdevelopment) - joint surfaces are comparable correctly.
- Pre-luxation is a slight displacement of the femur, the ends of the joint fit normally.
- Subluxation (incomplete dislocation)—the femoral head moves during active movements, but does not extend beyond the boundaries of the glenoid cavity.
- True dislocation - the head of the femur comes out of the acetabulum (articular) cavity, an extreme degree of dysplasia, requires surgical treatment.
Complications
If, when examining a child, the doctor discovers any dysplastic disorders in the development and correct formation of the hip joint, it is necessary to begin treatment immediately, without waiting for complications to arise.
- The child begins to walk later
- unsteady gait;
- clubfoot and flat feet appear;
- possible lameness;
- there is a possibility of developing osteochondrosis.
Lack of timely treatment for even minor changes in childhood in the future can not only worsen the quality of life, but also lead to disability.
Diagnostics
Immaturity of the hip joints in a newborn baby is normal. To exclude the development of pathology, all children should be regularly examined by an orthopedist at 1, 3, 6 months and a year.
It is necessary to identify and treat dysplasia from the first months of life.
To make a correct diagnosis, in addition to an external examination, it is necessary:
- X-ray examination - performed after 3 months;
- Ultrasound is a safe way to assess the condition of all joint structures and can be performed at any age from the first days of life.
- CT and MRI may be required if surgery is being considered.
Pathogenesis
Hip dysplasia is caused by a deficiency of connective tissue caused by mutations of various genes in different combinations and exposure to adverse environmental factors. Characteristic anatomical manifestations of hip dysplasia are underdevelopment of the joint: hypoplasia and flattening of the acetabulum in a newborn, slow development of the femoral head, bursal-ligamentous and neuromuscular apparatus of the joint, which causes its increased mobility.
Classification
There are several types of hip dysplasia:
- Femoral dysplasia . The mechanism of development of TB dysplasia is a violation of the neck-diaphyseal angle, which determines the centralization of the femoral head in the acetabulum (the angle of articulation of the femoral neck with its body). Both a decrease in the angle of the hip joint - coxa vara, and an increase in it - coxa valga can be observed (Fig. below).
- Acetabular dysplasia . The pathology is caused by a violation of the development of the acetabulum, which is reduced in size, flatter, with an underdeveloped cartilaginous rim.
- Rotational dysplasia . The movement of all joints of the lower limb is caused by a mismatch of axes (excessive antetorsion angle of the femur), that is, a violation of the location of the femoral head relative to the acetabulum.
According to clinical and radiological criteria preluxation (unstable hip), subluxation (primary, residual and hip dislocation (anterolateral/lateral), supraacetabular and iliac high dislocation .
Cervical dysplasia
The lower, narrow, cylindrical section of the uterus, partly located in the abdominal cavity and partly protruding into the vagina (supravaginal and vaginal parts, respectively), is the cervix.
The vaginal part of the cervix is examined using vaginal speculum during a gynecological examination. Inside, a narrow cervical (cervical) canal, 1-1.5 cm long, runs along the cervix, one end of which (external os) opens into the vagina, and the other (internal os) into the uterine cavity, connecting them.
The inside of the cervical canal is lined with a layer of epithelial columnar cells and contains cervical glands that produce mucus. The mucous secretion of the cervical canal prevents the introduction of microflora from the vagina into the uterus. Epithelial columnar cells are bright red in color.
In the area of the external uterine pharynx, the epithelial cylindrical cells of the cervical canal pass into multilayered squamous epithelium, which covers the walls of the vagina, the vaginal part of the cervix and has no glands. The squamous epithelium is pale pink and has a multilayer structure consisting of:
- basal-parabasal layer - the lowest, deepest layer of the epithelium formed by basal and parabasal cells. The basal layer of squamous epithelium borders the underlying tissues (muscles, blood vessels, nerve endings) and contains young cells capable of reproduction by division;
- intermediate layer;
- functional (surface) layer.
Normally, the cells of the basal layer are round in shape, with one large round nucleus. Gradually maturing and moving into the intermediate and superficial layers, the shape of the basal cells flattens and the nucleus decreases in size. Having reached the superficial layer, the cells become flattened with a very small nucleus.
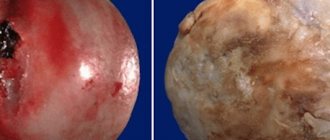
Cervical dysplasia is characterized by disturbances in the structure of cells and layers of squamous epithelium. The changed epithelial cells become atypical - large, shapeless, with multiple nuclei and the disappearance of the division of the epithelium into layers.
Cervical dysplasia can affect different layers of squamous epithelial cells. There are 3 degrees of cervical dysplasia depending on the depth of the pathological process. The more layers of epithelium are affected, the more severe the degree of cervical dysplasia. According to the international classification there are:
- Mild cervical dysplasia (CIN I, dysplasia I) - changes in the structure of cells are weakly expressed and affect the lower third of the stratified squamous epithelium.
- Moderate cervical dysplasia (CIN II, dysplasia II) - changes in the structure of cells are observed in the lower and middle third of the thickness of the squamous epithelium.
- Severe cervical dysplasia or non-invasive cancer (CIN III, dysplasia III) - pathological changes occur throughout the thickness of the epithelial cells, but do not spread to the vessels, muscles, nerve endings, as in invasive cervical cancer affecting these structures.
Causes
In the etiology of hip dysplasia in children, the leading role is played by the delayed development of the joint during intrauterine development (embryonic anlage), which develops under the influence of unfavorable endo/exofactors, as well as external influences on the joint after the birth of the child. Factors contributing to the development of hip dysplasia include:
- Unfavorable heredity (transmitted in an autosomal dominant manner from parents to child).
- Complications and unfavorable course of pregnancy (breech presentation of the fetus, large fetus, oligohydramnios, toxicosis of the first half of pregnancy, childbirth in women under 18 and over 35 years of age).
- Increased production of relaxin hormone , which is secreted in a woman’s body by the tissues of the uterus and placenta to prepare directly for childbirth (affects the ligaments, increasing their elasticity).
- Thyroid diseases.
- Infectious diseases from 10 to 15 weeks of pregnancy ( ARVI , rubella , influenza ).
- External influences - uncontrolled use of medications during pregnancy and alcohol, x-rays, radiation, unfavorable environmental conditions.
- Poor nutrition during pregnancy, contributing to the development of disorders of water-salt and protein metabolism, deficiency of vitamins and minerals in the body.
- Tight swaddling of the baby with straightened legs.
Symptoms of hip dysplasia
Signs of hip dysplasia in infants
As a rule, the symptoms in a newborn with hip dysplasia in the absence of displacement of the femoral head are extremely scarce. The main symptom in this period can be considered the presence of excessive rotation in one/both joints, as well as an increase in passive mobility in the hip joint. In infants, the early and main clinical symptoms of an unstable hip are:
- Limitation of the angle of passive extension of the legs in the hip joints of a newborn, bent at a right angle. Normally, the hips should be abducted to a horizontal plane (80-90); in the presence of pathology, there is a limitation in hip abduction (bilateral or on the affected side).
- Asymmetry of the buttock folds and skin folds on the thigh.
- Relative shortening of the leg and outward rotation of the limb.
- Marks-Ortolani/Barlow clicking or slipping sign.
Later symptoms of hip dislocation appear with the onset of independent walking and are manifested by a pronounced limitation of hip abduction, shortening of the hip (Galeazzi sign).
Sign of Galeazzi
Characteristic symptoms in children over one year of age include gait disturbance: the child clearly limps on one leg (symptoms of hip dislocation, on the one hand) or has a characteristic “duck” gait (pathology of both hip joints).
Symptoms in adults are manifested by pain in the hip joint, rapid fatigue when walking, a higher located greater trochanter and impaired locomotor functions (a specific pathobiomechanical symptom complex manifested by insufficiency of the gluteus medius muscle - Trendelenburg symptom ).
A decrease in the function of the gluteal muscle contributes to a violation of the stability of the pelvis - the occurrence of its lateral tilt, which is compensatory manifested by the Duchenne symptom (greater tilt of the body), due to increased function of the oblique abdominal muscles.
Functional shortening of the lower limb caused by upward displacement of the femoral head, changes in the gluteal muscles and lack of support for the femoral head contribute to the appearance of disturbances in the biomechanics of gait, namely: swaying of the pelvis and body when walking, disturbance of the rhythm of walking, and the appearance of lameness.
HOW TO TREAT CERVICAL DYSPLASIA
When determining the management tactics for a patient with this gynecological pathology, the severity of the detected changes, the patient’s age, reproductive function and plans for childbearing are taken into account.
1. SURGERY FOR CERVICAL DYSPLASIA.
For mild dysplasia (grade 1), this is radio wave treatment by creating thermal damage to a depth of 5-7 mm to destroy the potentially dysplastic epithelium underlying the transformation zone. The use of cryodestruction or laser vaporization for the treatment of grade 2 and 3 cervical dysplasia is not recommended due to the not always predictable depth of necrosis and the impossibility of postoperative histological control. For patients over 40 years of age, excision or conization methods for severe cervical dysplasia or in situ cancer are indicated, with mandatory examination of stepwise sections of the removed part of the organ. In case of severe dysplasia and intraepithelial oncology (cancer in situ), a consultation with a gynecological oncologist is indicated, followed by conization of the exocervix with curettage of the remaining part of the cervical canal and, if indicated, the uterine cavity. In postmenopausal patients with in situ cancer located in the transition zone of the cervical canal, the treatment of choice is hysterectomy.
CONIZATION OF CERVICAL DYSPLASIA
Conization of the cervix involves the removal of a conical section of cervical tissue with symptoms of dysplasia. The base of the cone is formed by the tissues of the exocervix (the vaginal part of the cervix), and the apex is formed by the tissues of the cervical canal. The transformation zone (the border between the exocervix and endocervix) is included in the conical tissue sample. With histological confirmation of the diagnosis and the absence of tumor cells in the resection margins and scrapings from the cervical canal, the given volume of surgical intervention is considered adequate.
Fig. 2 “Conization of the cervix with dysplasia.”
LOOP ELECTROCONIZATION OF THE CERVIX
Loop electroconization of the cervix or LEEP (Loop Electrosurgical Excision Procedure) or LLEETZ (Large Loop Electrosurgical Excision of Transformation Zone - large loop of electrosurgical loop excision of the transformation zone). The LEEP procedure is a surgical procedure that involves cutting out a thin layer of abnormal tissue using electric current and radio waves through thin loops called electrodes. The resulting tissue sample is sent to the laboratory for histological examination. In our clinic, the conization procedure for cervical dysplasia is carried out using a modern radio wave method.
Fig. 3 “Loop electroconization of the cervix (LEEP, LLETZ).”
Nuances of postoperative control.
After destructive methods and surgical treatment, examination of the cervix and colposcopy are carried out after 6-8 weeks. Patients with grade 1 dysplasia are advised to undergo observation (examinations including colposcopy and cytological examination) every 6 months for 2 years. observation (examinations, including colposcopy and cytological examination) of patients treated for CIN II, III should be carried out once every 3 months during the first year and 2 times a year thereafter; If treatment is effective, satisfactory colposcopy and cytological examination data, and negative HPV testing data, the patient can be transferred to the usual cervical screening regimen.
The presence of signs of dysplasia in the edges of the epithelium of the removed cervical sample indicates a high risk of relapse, but is not a reason for re-excision if:
- the transformation zone is completely visualized;
- there are no signs of glandular pathology;
- no signs of invasion;
- The woman's age is less than 50 years.
Women over 50 years of age with incomplete removal of dysplasia and positive endocervical margins are at risk for residual cervical disease. Adequate surveillance of endocervical cytology is the minimum requirement in this situation. An alternative method of treating cervical dysplasia with residual symptoms of the process is re-conization. Hysterectomy is indicated for women with persistent severe lesions, aggravated by the presence of a complicated general somatic and gynecological history.
2. DRUG THERAPY - an auxiliary method, used in the treatment of the cervix with an initial degree of dysplasia, or as a supplement to surgery.
Treatment of hip dysplasia
Treatment of hip dysplasia in children includes conservative and surgical methods. It should be understood that treatment of congenital dysplasia in newborns should begin as early as possible, since the later it is started, the longer the treatment process takes and the lower its effectiveness.
As a rule, in children under one year of age, dislocation of the hip joint is relatively easy to reduce using various functional techniques. Once a child reaches 5-6 years of age, it is no longer possible to correct a dislocated hip. Early therapeutic measures are aimed at gradual correction of disrupted relationships in the joint, provided that the age-related range of motion in the joints is maintained. The main goal of treatment is to achieve stable, complete reduction of the femoral head into the acetabulum while minimizing the risk of iatrogenic damage to the articular components.
Conservative treatment
Treatment of hip dysplasia in a child begins as early as possible with conservative treatment methods, including various orthopedic structures (stirrups, devices, splints, special pillows and panties) of a soft elastic design to hold the child’s legs in abduction and flexion.
For this purpose, the devices given below are used.
Pavlik stirrups
Frejk bandage (Frejk abduction panties, Frejk splint)
They work according to the well-known principle of wide swaddling. Made of dense material, they allow you to ensure that the child’s legs are constantly spread by more than 90°. Indicated for use for dysplasia in infants in the absence of dislocation, that is, in the presence of hip subluxation (Fig. below).
Vilensky tire
Designed to be worn constantly and cannot be removed even when changing the child's clothes. It is important to carefully adjust the length of the spacer. A modification of the Vilensky splint is the CITO splint.
Tübinger splint (orthosis)
It is a design combining Pavlik stirrups and Vilensky splints (Fig. below).
Only the most common orthopedic structures used to treat dysplasia are listed. There are other options, which you can familiarize yourself with by going to a specialized forum. Each design option has its own advantages and disadvantages in different clinics, and different doctors prefer one or another design.
However, parents should not choose an orthopedic design and carry out treatment on their own, but rather rely on the recommendations and prescriptions given by an orthopedic doctor. The duration of wearing orthopedic structures is quite long and is determined by the doctor individually. We should not forget that it is prohibited to put a child on his feet without the permission of an orthopedist.
Parents need to be patient. Despite the child’s whims, under no circumstances should you be cowardly and do not remove the structure, considering that a short break in wearing them does not pose a threat, since such behavior can lead to the child’s disability in the future.
As a rule, when wearing such functional splints, gradual closed reduction occurs; if necessary, wearing the splints is supplemented by myotomy (crossing the tendon) of the adductor muscles. For treatment, in addition to orthopedic splints, special children's massage, physical therapy (physical therapy) and physiotherapy are widely used. Drug treatment is not required during this period.
In some cases, even early functional treatment of congenital hip dislocation does not lead to reduction of the femoral head into the socket and its stable retention. In such cases (if there are indications - a mature dislocation of the hip in a child from one to 5 years of age without pronounced underdevelopment of the acetabulum or displacement of the femoral head), closed reduction of the hip is performed. It is performed under anesthesia.
The doctor performs a reduction, i.e., returning the femoral head to the correct position, guided by ultrasound/radiography data, after which a plaster cast is applied to the pelvis/lower limbs for 6 months, fixing the child’s legs in an extended position. After its removal, massage, physiotherapy and therapeutic exercises are prescribed. In case of combined dysplasia of several joints of the lower extremities (hip and knee joints), along with the treatment of hip dislocation, treatment of dysplasia of the knee joints in children is carried out.
Hip dysplasia in adults
Treatment of hip dysplasia in adults is significantly difficult, which is due to the gradual (by the age of 25-30) development of hip arthrosis, and later - deforming coxarthrosis and osteochondrosis , accompanied by severe pain, disturbance of gait, posture, and a significant decrease in the range of movements in the hip joint. Treatment of the disease in adults includes medication.
To relieve pain, symptomatic therapy is used - NSAIDs ( Diclofenac , Ibuprofen , Ketoprofen , etc.). To normalize the synthesis/catabolism of glycosaminoglycans Chondroitin sulfate , Glucosamine sulfate ( Structum , Chondroxide , DONA , Rumalon , etc.) or combined chondroprotectors ( Teraflex , Artra , Artroflex ) are prescribed in courses of 2–4 months.
To improve collagen formation, it is recommended to take Solcoseryl , Vitreous , L-lysine , L-proline in combination with a complex of vitamins D2/D3 and group B, C, E, nicotinic acid , as well as micro/macroelements ( Magnerot , Magne B6 , Zinc Aspartate , Zincite , Copper sulfate , Selenium ).
Physiotherapeutic treatment, exercise therapy, and massage are provided. If necessary, orthopedic correction using special devices to reduce the load on the hip joint. In severe cases - surgical treatment, and in case of joint dysfunction - endoprosthetics.
Medicines
—
Procedures and operations
Massage for hip dysplasia.
It is carried out as prescribed by an orthopedic doctor and is carried out without removing orthopedic structures. The massage is aimed at reducing/relieving increased muscle tone in the legs and improving blood circulation in the joint by actively influencing the muscles in the buttocks, back and legs. Massage for children with hip dysplasia is necessary for any degree of dysplasia.
Parents need to undergo training with a specialist and be sure to massage the child’s buttocks, joints and feet before performing physical therapy exercises. For massage, you can use only natural oil that does not contain fragrances or fragrances. The child is placed on a flat and hard surface on his back, having previously laid a blanket/diaper. It is important to follow the sequence of techniques (stroking, rubbing, kneading).
First, warm up (light massaging strokes on the surfaces of the thighs, joints, gradually moving, without pressing, to circular movements for 5 minutes). Next, applying a little effort, the sore joints are rubbed by alternating direct movements with careful circular strokes. Then the child turns over on his tummy and the lumbar area and buttocks are massaged (Fig. below). Course 10-15 sessions.
Physiotherapeutic procedures for hip dysplasia
Applications with ozokerite , electrophoresis with calcium, iodine and phosphorus, UV therapy, and salt baths are widely used.
Physiotherapy
Gymnastics is a mandatory component of treatment. In this case, a set of exercises is selected for each stage of exercise therapy (leg extension, stabilization of joints in a physiological position and rehabilitation). The most commonly used exercises are spreading the hips to the sides, rotating the hips along the axis, “bicycle”, games “ladki”, “butterfly”, imitation of crawling, exercises (swimming) in the water.
Surgery
Indications are severe displacement of the femoral head, which cannot be reduced using a closed method; child's age after 5-6 years; pinching of articular cartilage in the joint cavity, pronounced anatomical defects (underdevelopment of joint structures). Various types of surgical interventions are used:
- Open reduction of dislocation through cut tissues of the thigh.
- Operations on the femur (osteotomy) - dissection of the proximal end of the femur to give it the required configuration.
- Reconstructive operations on the pelvic bones to create a support above the femoral head, which prevents it from moving upward.
- In late diagnosed cases of hip joint dislocation with severe impairment of its function, hip replacement is performed.
The most important component of restoring joint function is rehabilitation after surgery.
What is hip dysplasia
Dysplasia in children under one year of age occurs as a result of delayed or incorrect formation of the elements of the hip joint in the prenatal period or immediately after birth. Dysplasia (from the Greek dys - disorder and plaseo - form) means a developmental defect. The immaturity of the hip joint in a newborn leads to a violation of the configuration of the joint - the femoral head and the articular cavity on the pelvic bone do not correspond to each other. As a result, congenital dislocation of the hip joint is formed.
Prevention
Prevention of hip dysplasia consists in the high alertness of doctors regarding newborns in mothers with a high risk of developing hip dysplasia and parents regarding the risk of developing this pathology of the hip joints. The basis of prevention is a thorough repeated examination of newborn children and monitoring them during the first year of life, and if a pathology is detected, its treatment as early as possible. It is necessary to carry out educational work so that parents know how to identify hip dysplasia in children (characteristic symptoms).
The famous pediatrician Komarovsky believes that in the presence of initial degree joint dysplasia (unstable/immature hip), proper care for the child is necessary and, above all, wide swaddling (Fig. below). Wide swaddling for hip dysplasia in infants is mandatory for all babies at risk with signs of an immature joint.
Dr. Komarovsky, as an alternative, recommends (see the forum) to use disposable diapers 1-2 sizes larger than necessary (with a wide layer of sorbent between the child’s legs). In addition, all children diagnosed with “immaturity of the hip joint” should be classified as a risk group and be registered with a pediatric orthopedist with periodic ultrasonography of the hip joints. If the dynamics are negative, the doctor prescribes the wearing of specialized orthopedic structures.
In the future, children at risk are recommended to undergo a control X-ray examination of the hip joint 1-2 times a year. Also, for such children, physical activity is limited and attendance at special orthopedic groups is recommended.
DEGREES OF CERVICAL DYSPLASIA
The disease can affect various layers of surface epithelial cells. Depending on the depth of the pathological process, there are several degrees of severity of cervical dysplasia. The more layers of epithelium on the neck are affected, the more severe the degree of dysplasia.
According to ICD-10 • N87, the following degrees of development of cervical dysplasia are currently distinguished (1, 2 and 3):
Cervical dysplasia of the 1st degree (mild, squamous intraepithelial damage of a small, weak degree) - moderate proliferation of epithelial cells of the basal and parabasal layers.
Stage 2 cervical isplasia ( moderate, moderate severity) - pathological changes cover the entire lower half of the epithelial layer.
Cervical dysplasia of the 3rd degree (severe, carcinoma in situ) - pathological changes occur throughout the thickness of the epithelial cells, but do not spread to the vessels, muscles, or nerve endings. This form already refers to precancerous conditions. Combining severe cervical dysplasia and carcinoma in situ into one category is justified due to the difficulty of their cytological differentiation. The final diagnosis is made on the basis of histological findings.
Fig. 1 “Progression of cervical dysplasia, from grade 1 to cancer.”
How does the degree of cervical dysplasia determine the possible course of the disease?
An analysis of the outcomes of dysplastic changes in the squamous epithelium of the cervix shows that with grade 1 dysplasia, regression is observed in 57%, persistence in 32%, progression in 11%, and the development of invasive cancer occurs in only one to three percent of cases. At the same time, with severe cervical dysplasia (grade 3), regression is observed in 32%, and malignancy occurs in more than 12% of cases.
CAUSES OF THE DISEASE
Its close relationship with herpes and HPV types 6, 11, 16, 18, 31, 33 and 35 has been revealed. Dysplasia of the cervical epithelium can be detected against the background of other diseases (pseudo-erosion, cicatricial deformation with ectropion, leukoplakia, polyps), but it can be on a visually unchanged neck.
The presence of risk factors greatly increases the risk of developing dysplastic processes on the cervix. Such provoking agents may be:
• Repeated pregnancies and/or births before the age of 20, • Early age of first sexual intercourse, • Presence of genital warts, • HSV-2 (HSV2) - herpes simplex virus, type 2, • Smoking, incl. passive, • Promiscuity, • Chronic cervicitis, • History of genetic oncofactor, • Reduced immunity, • Cervical injury.
In addition to the risk factors described above in the development of dysplasia, the significance of genetic predisposition, the association of dysplastic changes with bacterial vaginosis, and the role of absolute or relative hyperestrogenism are discussed.
SYMPTOMS OF THE DISEASE
Cervical dysplasia usually does not have a specific clinical picture. Absolutely asymptomatic pathology develops in 10-25% of women; the remaining category of patients has the opportunity to stop the process thanks to regular examinations by a gynecologist. If there is a microbial infection of the genital tract, there may be complaints of discharge, sometimes mixed with blood, pain during intimacy, etc. Most often, if there is dysplasia of varying severity on the cervix, patients present the following complaints:
- Itching in the vagina
- Burning sensation
- Discharges that are not typical for a healthy state, including bloody discharge
- Pain during sexual intercourse
- Nagging pain in the lower abdomen
- Visible condylomas, papillomas
Cervical dysplasia has a long course and can resolve after appropriate treatment.
DIAGNOSTICS AND ANALYSIS
What tests should be taken for cervical dysplasia? Gynecology takes into account the absence of pronounced clinical symptoms, therefore, instrumental and laboratory methods are placed at the forefront in diagnosis. Primary cytological examination of the cervix and cervical canal is a classic screening method for identifying pathological changes in the epithelium of the cervix.
The diagnostic algorithm for identifying cervical pathology is reduced to collecting anamnesis, a general examination of the patient, examination in the speculum and cytological examination using the Pap test at the first stage. In the absence of pathology of the squamous and glandular epithelium of the cervix based on the results of a standard cytological examination, further observation is recommended.
If a suspicion of cervical pathology is detected, the patient is subject to in-depth diagnostics. Tests for cervical dysplasia are taken to diagnose the condition of the exo- and endocervix and identify possible cervical pathology.
The optimal list of studies for suspected and presence of dysplasia:
- Examination with a gynecological speculum,
- Extended and video colposcopy,
- Oncocytology from 2 points,
- Tests for STDs,
- Analysis for HPV oncotypes,
- Direct biopsy.
The HPV-PAP test is the “gold standard” in diagnosing cervical dysplasia. The analysis determines clinically significant concentrations of the HPV virus at which the development of the oncological process occurs. Accordingly, using various treatment methods, it can be prevented.
Consequences and complications
Delayed diagnosis and lack/ineffective treatment can lead to a number of complications:
- Impaired functions of the hip joint.
- Shortening of the injured limb.
- Deformations of the glenoid cavity.
- Development of pelvic asymmetry and curvature of the spinal column.
- Formation of flexion-adduction contracture.
- Avascular post-reposition necrosis of the femoral head .
- Multiplanar deformations.
- Development of hip arthrosis / dysplastic coxarthrosis .
List of sources
- Lukash Yu.V., Shamik V.B. Early diagnosis of hip dysplasia in newborns // Modern problems of science and education. – 2012. – No. 6.
- Sertakova A.V., Morozova O.L., Norkin I.A., Anisimov D.I. Modern ideas about the mechanisms of development of hip dysplasia in children (review). Saratov scientific and medical journal. 2011. T. 7. No. 3. P. 704–710.
- Congenital dislocation of the hip in infants. Clinic, diagnosis, conservative treatment and rehabilitation / Baindurashvili A.G., Voloshin S.Yu., Krasnov A.I. – 2016
- Evseev, V.I. Biomechanical substantiation of the mechanogenesis of subluxation and dislocation in hip dysplasia / V. I. Evseev, V. D. Sharpar, I. A. Komolkin // Current issues in pediatric traumatology and orthopedics. St. Petersburg, 2004. - pp. 234-237.
- Goncherenko V. A., Stronina S. N., Klestova E. O. Congenital hip dislocation: frequency, structure, analysis of diagnostic and treatment methods // Young scientist. - 2021. - No. 3. — P. 257-259.