Cartilage tissue is destroyed imperceptibly, since the cartilage lining has no innervation - in other words, it does not hurt. Pain occurs when the cartilage deforms and thins and increases the load on the joints located near it. Chondromalacia of the knee joint is one of the types of damage to the cartilage pad - deformation of the posterior part of the kneecap. It is good if the disease is detected at the initial stage. Since the advanced stage of the deformity presents a sad picture of a through lesion, up to the exposure of the joint.
Causes
The two main causes of softening of articular cartilage are of greatest importance:
- Intense loads on the joint. Most often the knees of athletes involved in running and jumping are affected.
- Features of the structure of the knee joints. Women are more susceptible to pathology than men due to certain anatomical features.
As a result of pathological changes, articular cartilage begins to deteriorate, becomes soft and loses its elasticity. One of the main functions of cartilage – shock-absorbing – is lost.
At CELT you can get a consultation with a traumatologist-orthopedic specialist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
Effective Treatments
Chondropathy of the knee joint responds well to conservative therapy. Surgical intervention is usually indicated for developed complications, for example, severe bone deformation. Patients are recommended to wear orthoses that fix the joint structures, preventing their displacement or damage. In some cases, a plaster cast may be applied.
Knee brace.
Drug therapy
To eliminate pain, patients are prescribed non-steroidal anti-inflammatory drugs. In case of knee chondropathy, they are not very pronounced, so drugs in the form of tablets and ointments are used - Nimesulide, Celecoxib, Ketorol, Fastum, Voltaren. Since the pathology in most cases affects children and adolescents, the doctor calculates daily and single dosages taking into account age, weight, listed in the annotation of contraindications.
| Drugs used to treat knee chondropathy | Names of medicines | Therapeutic effect of drugs |
| Systemic chondroprotectors | Teraflex, Structum, Artra, Chondroxide, Alflutop, Dona, Chondrogard | Chondroprotectors partially restore damaged cartilage and bone tissue, improve the condition of the ligamentous-tendon apparatus |
| Preparations with B vitamins | Combilipen, Milgamma, Neurobion, Neuromultivit, Pentovit | Medicines increase blood flow and improve the functioning of the neuromuscular and cardiovascular systems |
| Balanced complexes of vitamins and microelements | Multivit, Vitrum, Multitabs, Centrum, Semevit, Supradin, Complivit | The drugs have a general strengthening, tonic effect, replenish reserves of bioactive substances, improve the functioning of all vital systems |
Physiotherapy
Pain in the knee joint of mild to moderate severity, characteristic of chondropathy, can be eliminated by physiotherapeutic procedures. Healing activities also stimulate blood supply to cartilage and bones, preventing the spread of the pathological process to healthy tissues. The following physiotherapy procedures have proven themselves to be particularly effective in the treatment of chondropathy:
- UHF therapy;
- magnetic therapy;
- laser therapy;
- shock wave therapy;
- galvanic currents.
UHF session.
It is practiced to apply applications with ozokerite or paraffin to the knee. Under the influence of heat, the regeneration of damaged structures, the removal of waste, toxins, and harmful salts are accelerated. At the rehabilitation stage, electrophoresis or ultraphonophoresis with chondroprotectors, B vitamins, and calcium chloride solution are used.
Physiotherapy
Since it is active sports training that often leads to the development of chondropathy, doctors recommend that patients reduce physical activity. During therapy, you should prefer swimming, physical therapy, and gymnastics. Daily exercises help strengthen the muscle-tendon system of the knee without putting stress on the bones and cartilage.
It is allowed to perform isometric exercises to maintain strength and muscle mass. Physical therapy doctors, after studying the diagnostic results, often allow training with a barbell or dumbbells, but not in a standing position. But jogging is strictly prohibited. Subsequently, after complete recovery, the teenager can return to running, football, and basketball.
Surgery
The ineffectiveness of conservative therapy over several months becomes an indication for surgical intervention. Arthroscopic surgeries performed in a minimally invasive manner make it possible to restore damaged bones and cartilage, while avoiding severe damage to connective tissue structures. The surgeon inserts instruments through small punctures or cuts in the skin above the knee. Manipulations are carried out with miniature arthroscopic instruments, and the progress of the operation is visualized on the monitor.
After minimally invasive surgery, the patient remains in the department for a short time under the supervision of medical staff. A few days later he is discharged for further rehabilitation. At the recovery stage, massage, physiotherapeutic procedures, and exercise therapy are indicated.
Folk remedies
It is not advisable to use products made according to traditional medicine recipes in the treatment of chondropathy. Firstly, they do not contain ingredients that can prevent deformation of cartilage and bone tissue. Secondly, folk remedies contain components that often provoke the development of local or systemic allergic reactions. Thirdly, most medicinal plants are prohibited for use in the treatment of children and adolescents.
Degrees of the disease
There are 4 degrees of chondromalacia:
- The first is characterized by thickening and softening of cartilage with the appearance of swellings. There is practically no pain syndrome. The specialist prescribes washing the internal area of the joint capsule.
- The second is that cracks and depressions appear on the joint, which provoke acute pain and have a chronic form. The pathology occurs in professional athletes who train through pain. Specialists excise the inflamed area with surgical scissors and wash the internal cavity of the joint.
- Third, the depressions and cracks are larger than 1 centimeter in size, and the bone opens due to significant deformation. To eliminate the pathology, plastic surgery and the use of a graft are performed.
- The fourth is the most severe degree, which is characterized by exposure of the subchondral bone.
Symptoms of the disease
Each type of knee chondropathy has its own specific signs, which often help diagnose the pathology at the first visit to the doctor. But there are general clinical manifestations that are similar to the symptoms of many musculoskeletal diseases:
- crunching, clicking, crackling when bending or straightening the knee;
- swelling, hyperemia due to blood vessels overflowing, increased local temperature;
- discomfort, and then pain when moving.
The teenager begins to noticeably limp and tries not to put full weight on his foot in order to minimize pain. It is also possible for the muscles to weaken with further atrophy, and the legs to shorten by several centimeters. With the accumulation of exudate in the joint cavity and the development of the inflammatory process, a deterioration in well-being occurs, including dyspeptic disorders. The psycho-emotional state of the patient changes. He becomes lethargic, apathetic, drowsy or, conversely, irritable and hot-tempered.
Diagnostics
To confirm the diagnosis and assess the condition of the articular cartilage, the orthopedic traumatologist, after examination, prescribes the following studies:
- Magnetic resonance imaging. This study is more accurate than x-rays and allows for a more detailed examination of the joint.
- Arthroscopy is an endoscopic examination in which the doctor inserts special equipment with a miniature video camera into the joint through a puncture. This is the most accurate technique that allows you to examine the articular cartilage in detail.
The modern equipment of the multidisciplinary CELT clinic allows for high-quality comprehensive diagnostics.
Treatment. Knee-joint. Chondromalacia of knee cartilage
What is Chondromalacia Patella?
This is the destruction of the cartilage of the posterior (articular) surface of the patella. As a result, the former elasticity is lost and its loosening is observed. According to statistics, chondromalacia of the patella is in first place for the causes of pain at a young age, with the exception of the traumatic consequences of it. Most often, this pathological process occurs in athletes and people engaged in heavy physical labor. Some anatomical features of the joint structure imply a more frequent incidence in women.
A number of authors consider chondromalacia of the patellar cartilage as one of the manifestations of the autoimmune process, which currently requires a greater evidence base. Read more about the treatment of chondromalacia cartilage of the knee
Symptoms
Clinically, chondromalacia of the patella does not manifest itself for a long time; pain appears when the inflammatory process sufficiently spreads through the cartilage tissue. Swelling of the knee joint is often detected; the temperature, as a rule, is either normal physiological or low-grade.
Conservative treatment
Treatment usually begins with conservative methods:
- recreation;
- NSAIDs;
- changing your training regimen;
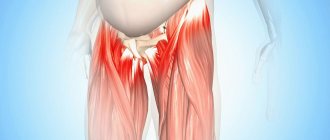
- After this, a rehabilitation program is prescribed, which is based on stretching the extensor muscles, the iliotibial band, the ligaments that support the patella, and the posterior thigh muscles.
- increasing the strength of the quadriceps muscle, especially the oblique part of the vastus medialis muscle, as the main limiter of patellar mobility. It is believed that due to the weakness of this muscle compared to the vastus lateralis muscle, the patella is subject to external subluxation. Low-range quadriceps strengthening exercises and straight leg raises reduce the patellofemoral joint's response to this imbalance.
- In addition to exercises, you can prescribe elastic bandaging of the knee joint, fixation of the patella with a bandage or orthopedic device.
Surgery
There are many surgical options for treating chondromalacia patella. Most of them are aimed at restoring the correct anatomical position of the femoral-patellar joint, a small part - at the regeneration of the cartilaginous lining. In severe cases, contouring of the articular surfaces and patellectomy are indicated.
Knee arthroscopy
It is not only an important diagnostic, but also a therapeutic procedure. Although the advisability of irrigating the joint cavity and removing pathological tissue during arthroscopy remains a matter of debate, the value of this examination in determining the stage of the disease and planning surgical treatment is obvious. Arthroscopic lavage temporarily reduces pain and improves function by removing dead tissue and proteoglycans produced by inflammation. But since the cause of the disease is not eliminated with this manipulation, the symptoms usually reappear. When arthroscopically staging the disease, the Outerbridge system is widely used because of its simplicity and reproducibility of results. The system is based on determining the location, shape, size and depth of the defect. This kind of minimally invasive technology has an extremely beneficial effect on the outcome of the disease, the duration of rehabilitation, etc. Treatment of chondromalacia of the cartilage of the knee joint now seems to be a simpler task that does not burden the patient, which is important.
- Defects of the first degree are soft thickenings, sometimes swellings.
- Grade II is characterized by depressions and fissures with a diameter of less than 1 cm.
- Grade III damage looks like deep cracks with a diameter of more than 1 cm, reaching the bone.
- Grade IV is characterized by exposure of the subchondral bone.
Lavage and removal of dead tissue is more appropriate for injuries without evidence of patellar instability than for degenerative lesions of a nontraumatic nature. If the patella is tilted and there is minimal damage to the articular surfaces, especially the lateral facet, the lateral edge of the patella can be mobilized with arthroscopy. This intervention is only appropriate for clinically obvious patellar tilt and non-severe joint injuries. In general, arthroscopic lavage and removal of pathological tissue with or without mobilization of the lateral edge of the patella is warranted for grades I–II lesions; in grades III–IV, long-term results are usually poor.
Arthroscopic chondroplasty
For severe cartilage degeneration, arthroscopic chondroplasty is used. Methods of abrasive and microgap chondroplasty include mechanical penetration into the underlying bone with the introduction of bone marrow mesenchymal stem cells into the defects, stimulating the regeneration of fibrocartilaginous tissue. Arthroscopic chondroplasty is usually performed on people under 30 years of age with well-demarcated grade III lesions; for more severe lesions it is contraindicated. This type of surgical intervention has its positive and negative aspects and has found its application in sports medicine. Clinically, the treatment of chondromalacia is no different, but from a functional point of view, the range of motion in the joints returns fully.
Additional methods are aimed at restoring hyaline (articular) cartilage. To regenerate cartilage, implantation of one's own chondrocytes, transplantation of an osteochondral auto- or allograft, and plastic surgery with a fragmented osteochondral graft (mosaic plastic) are performed. Implantation of native chondrocytes is carried out in case of significant through defects in the cartilaginous lining of the femoral condyle, which manifest themselves clinically. First, the patient's chondrocytes are harvested, then they are cultured and placed under a periosteal flap, on the articular surface defect cleared of pathological tissue. According to long-term cooperative studies, good and excellent results were obtained in 79% of cases. The method is indicated for young (20–50 years old) active patients with isolated (2–4 cm²) traumatic defects of the cartilaginous lining of the femoral condyles. The results of filling defects in the patellar surface of the femur or patella are much worse. Contraindications include extensive osteoarthritis, instability or tilting of the patella with subluxation, and previous meniscectomy.
Transplantation of an osteochondral autograft and mosaic plastic surgery are interesting because they use their own intact cartilage to fill deep defects. However, to accurately restore the relief of the articular surface requires considerable technical skill. In addition, the number of donor areas is limited and complications at the sites of cartilage collection cannot be excluded. Osteochondral allografts are usually used for large (10 cm² or more) defects of the femoral condyles and often after failure of other methods. In fresh allografts, chondrocytes are more viable, but at the same time they are more immunogenic and increase the risk of infection transmission. Moreover, fresh allografts are difficult to handle and require the surgeon and the patient to clearly plan the timing of the intervention in a relatively short time. Fresh frozen allografts are less likely to cause immune reactions and provide greater freedom in choosing the timing of surgery, but both chondrocyte viability and long-term graft viability are lower. Patellectomy and patellar contouring are used for extensive injuries to the patella that cause significant impairment of function due to pain, and also when other treatment methods have not produced the desired effect. The results of the methods are ambiguous. Surgeries that require movement of large amounts of tissue, such as osteotomy, transfer and elevation of the tibial tuberosity, and others, will be discussed in the section on patellar tilt and subluxation.
Our doctors
Samilenko Igor Grigorievich
Traumatologist - orthopedist, doctor of the highest category
24 years of experience
Make an appointment
Zubikov Vladimir Sergeevich
Traumatologist-orthopedist, Doctor of Medical Sciences, doctor of the highest category, professor
44 years of experience
Make an appointment
Marina Vitaly Semenovich
Traumatologist-orthopedist, head of the minimally invasive traumatology and orthopedics service
Experience 36 years
Make an appointment
Poltavsky Dmitry Ilyich
Traumatologist-orthopedist
Experience 28 years
Make an appointment
Osteochondritis dissecans of the elbow joint
The term "osteochondritis" means inflammation of bone and cartilage, while the word "dissecting" comes from the Latin "dissect", which means "to separate, cut off." This term continues to be used despite the absence of inflammatory cells in histological specimens of excised osteochondral fragments.
Osteochondritis dissecans of the elbow is a local process involving the articular surface, which ultimately leads to the separation of a fragment of articular cartilage and subchondral bone. This condition was first described by Konig in 1888 as a cause of the formation of loose bodies in the hip and knee joints without direct traumatic influence.
Osteochondritis dissecans of the elbow was first described by Panner, who noted the similarity of this condition to Legg-Calvé-Perthes disease.
Most often, osteochondritis dissecans affects the capitate eminence of the humerus in the central or anterior outer sections. Cases of localization of pathological foci in the trochlear region, head of the radius, olecranon and olecranon fossa have also been described.
Reasons for development
Most researchers believe that repeated microtrauma plays an integral role in the development of the disease. There is also evidence in favor of the ischemic theory of the development of osteochondritis dissecans.
Osteochondritis dissecans of the elbow joint often develops in athletes aged 11-22 years who experience excessive stress. The high-risk group includes adolescent athletes who experience repeated stress loads. Pathology is more common in boys and, as a rule, on the dominant limb.
A number of authors presented their interpretation of the dependence of the development of the pathological process in baseball and gymnastics. The dominant factor is the action of compressive or shear forces at the level of the humeroradial joint. The humeroradial joint, taking up to 60% of the axial compressive load, additionally serves as an auxiliary elbow stabilizer. The valgus stress experienced by the elbow joint during the swing phase of throwing creates a significant compressive load at the level of the brachioradialis joint. These forces can cause subchondral fractures or damage to the thin vessels leading to the capitate eminence.
Anamnesis
Osteochondritis dissecans is a pathology of young athletes (usually boys) and manifests itself at the age of 12-14 years, in contrast to Panner's disease, which manifests itself at 9-10 years. The dominant limb is most often affected; the number of patients with bilateral pathology is 5-20%. The history includes repeated collisions, excessive stress, and participation in sports that require hands above the head.
Symptoms
At an early stage, symptoms may be mild and consist of pain, the localization of which is difficult to determine. Most often, slight pain appears after exercise. Symptoms usually increase slowly. During the examination, patients complain of pain that intensifies after exercise, limitation of movements and swelling on the outer surface of the elbow area, the appearance of clicks in the joint and sudden weakness when lifting heavy objects.
Clinical examination
Classic signs include loss of full extension and swelling along the posterolateral surface of the joint, along with inflammation of the normal posterolateral fold. Performing a valgus-extension test causes pain in the outer part of the joint and leads to even greater limitation of extension, which is one of the key distinguishing signs of osteochondritis dissecans.
Most injuries resulting from throwing or hyperextension during the valgus test are characterized by pain along the inner surface of the joint. These conditions can occur simultaneously, but when performing an instability test, especially with valgus loading, patients with osteochondritis dissecans experience pain more on the outer surface.
Visualization
When performing radiography in standard (antero-posterior and lateral) projections, a classic sign is revealed in the form of a clearing zone in the central part of the capitate eminence of the humerus. In the center of the rarefied zone, a small area of increased density can be determined. At later stages, a free body may be detected.
Additional tests may be needed in the early stages of treatment. To identify such pathological foci, CT, arthrography and ultrasound are used. However, the standard examination for such conditions is MRI. Key signs, the assessment of which can help determine treatment tactics, are: the amount of bone tissue involved in the pathological process, the integrity of the cartilage covering, and the presence of free bodies.
Classification
The first attempt at classification was made by Minami based on lateral radiological features:
- Degree 1 – the presence of a shadow in the center of the capitate eminence.
- Grade 2 – the presence of a free zone between the lesion and the adjacent subchondral bone.
- Degree 3 – the presence of one or more free bodies.
Bradley and Petrie expanded this classification to include MRI features. Baumgarten classified lesions based on arthroscopic findings, similar to Ferkel's classification of talus lesions.
All these classifications do not reveal the patterns of development of pathology and have limited application.
Treatment of osteochondritis dissecans of the elbow joint
There is no generally accepted treatment strategy for osteochondritis dissecans. Treatment options range from complete avoidance of all irritants to immediate surgical intervention.
Conservative treatment can be used in patients with intact articular cartilage. If there is damage to the articular cartilage covering, conservative measures can also be used, however, with less chance of recovery.
The principles of conservative treatment are rest and complete exclusion of irritating influences. Such restrictions are necessary until the symptoms disappear (6-12 weeks), X-ray confirmation of complete recovery of the pathological focus on MRI (6-12 months).
An alternative method of treatment is the use of an unloading articulated orthosis for the elbow joint. Sports and everyday activities while wearing an orthosis are allowed to an extent that does not cause symptoms. The use of this type of treatment allows the patient to maintain activity without aggravating the impact on the pathological focus. In most cases, the patient returns to normal physical activity within 2 weeks of starting treatment.
Progression of the pathological process, the presence of symptomatic loose bodies or damage to the cartilaginous covering, which is aggravated despite resting conditions, the use of an orthosis, and the exclusion of physical activity are grounds for surgical intervention.
Modern principles of surgical treatment are arthroscopic assessment of the affected area, removal of loose bodies , debridement of the base of the pathological focus. Most modern studies emphasize the effectiveness of arthroscopic treatment.
Surgical treatment is recommended in cases of loose bodies, extensive involvement of the capitate eminence, or disease progression. The procedure is performed arthroscopically and consists of removing loose bodies, debridement of the pathological focus and reaming its bed. Fixation of large fragments is carried out using cannulated Herbert-Whipple screws. For extensive lesions with a defect in the lateral surface, osteochondroplasty is used.
Complications
- Relapse or progression of the pathological process.
- Arthrofibrosis.
- Heterotropic ossification.
Rehabilitation
In most cases, after debridement has been performed, patients begin exercises on the CPM machine on the day of surgery. An orthosis is placed on the elbow joint to relieve the capitate eminence. Within a week after the intervention, physical therapy with gentle stretching, pneumatic compression, and exercises for the hand and wrist is started.
The patient is transferred to the usual regimen during the first three weeks after surgery. Clinical observation is carried out with dynamic radiographs taken. Return to sports activities is allowed as painless range of motion and strength indicators are restored.
The recovery period can vary and range from 6 to 16 weeks.
Treatment
In the early stages, they try to treat chondromalacia with conservative methods:
- limiting physical activity;
- wearing a special orthopedic patella to stabilize the joint;
- anti-inflammatory agents and hyaluronic acid preparations to combat pain and inflammation;
- physiotherapeutic treatment;
- physical therapy to strengthen leg muscles.
If these methods do not produce results, surgical intervention is performed. During arthroscopy, the doctor inserts special instruments into the joint and corrects the shape of the cartilage.
Symptoms of the disease.
Chondromalacia of the knee joint makes itself felt with the following symptoms:
- When walking, a crunching sound in the knee joints may bother you;
- Periodic aching pain in the knee, increasing during or after training, and even minor physical activity - squats, climbing stairs;
- Swelling of periarticular tissues.
Even a crunch in elite sports is a reason to consult a doctor. As a rule, an initial examination is not enough to assess the condition of the cartilage tissue, so the doctor will prescribe additional tests, most often an MRI. An additional diagnosis for an atypical course of the disease or an unclear picture is arthroscopy, which we will discuss below.
Prevention
To avoid the development of the disease, you need to follow 7 rules:
- Always warm up thoroughly before performing strenuous exercise and use warming ointments.
- Additionally protect the knee joint with elastic bandages and bandages before training.
- Avoid sudden weight gain and obesity, so as not to create increased stress on the joints.
- Wear shoes of the appropriate size, made from natural materials and with soft soles. It is advisable to give preference to models with instep supports.
- Try to avoid injuries and blows to the knee area (relevant for contact martial arts).
- Reduce the amount of salty foods in your diet to avoid salt accumulation in the joints. Additionally, you need to reduce the amount of soda, tea and coffee, and also give up alcohol (all this washes away vitamins and minerals).
- Eat more foods rich in calcium, fluoride and zinc. It is advisable to add jellied meat and dairy products to your diet, as they strengthen cartilage and bone tissue.
At the first suspicion of the development of chondromalacia, immediately contact a specialist for diagnosis.
The multidisciplinary CELT clinic employs experienced traumatologist-orthopedic surgeons and has all the necessary equipment.
Description of the disease
Chondropathy begins to develop in childhood or adolescence, affecting the tubular bones of the legs and cartilage tissue. It is characterized by a benign chronic course. The pathology responds well to treatment and rarely causes complications from the musculoskeletal system.
Destructive changes in the knee occur due to disruption of metabolic processes against the background of deteriorating blood circulation. A deficiency of nutrients occurs, which leads to the destruction of that part of the bone that is subject to the greatest static and dynamic loads. The destructive process occurs in several stages:
- over the course of several months, gradual necrosis of bone tissue occurs, manifested in mild pain when bending or straightening the knee;
- for about six months the bone seems to “sag,” and its beams (structural elements of the bone) shift relative to each other, causing a decrease in the height of the epiphysis and an increase in the joint space;
- over the course of several months or years, dead areas of bone are resorbed, and in their places granulation tissues, osteoclasts, are formed, which causes a decrease in bone height;
- within 5-18 months, the shape and structure of the bone is restored.
In total, chondropathy lasts about 3 years. But only in rare cases does complete regeneration of bone tissue occur in the absence of medical care - usually more or less pronounced residual deformation is detected. And with timely diagnosis of the pathology and treatment, it is possible to completely restore the bone that forms the knee joint.
Orthopedics and traumatology services at CELT
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| MRI of the knee joint (1 joint) | 7 000 |
| MRI of the shoulder joint (1 joint) | 7 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Stages of the disease and principles of diagnosis
In modern medicine, there are 4 main stages of the disease. The division occurs on the basis of the x-ray picture, as well as the severity of the symptoms of the disease.
- First stage
It is characterized by a complete absence of symptoms or complaints ignored by the patient in most cases. The discomfort is mild, the pain is not clearly localized. On an x-ray image during this period, the doctor will note the presence of an oval body, which is separated from the main bone mass by a thin strip of light color.
- Second stage
The disease is progressing. The patient complains of moderate pain in the ankle joint. Your doctor may want to look for signs of synovitis. During this period, X-rays show an expansion of the clearing band. The endplate in the problem area ceases to be integral.
- Third stage
During this period, patients first begin to complain about blockades of the joint, its “sticking” when moving. A person pays attention to the intensification of pain, their presence even if the injured limb remains at rest. The x-ray shows the presence of a necrotic area, which is only partially connected to the main bone.
- Fourth stage
The person notes an increase in pain. However, at stage 4, joint blockades develop less frequently than at stage three. Synovitis intensifies, and even a change in the configuration of the joint is possible. An x-ray reveals the presence of an intra-articular body, which is the main source of the patient’s problems.
In most cases, radiography is used as an instrumental method. The method is simple, accessible, and has high diagnostic value.
CT scan reveals osteochondral damage to the talus.
However, sometimes necrotic bone particles are not visible on an x-ray due to their small size. In this case, the diagnosis is supplemented with MRI or CT techniques. Both methods make it possible to make a diagnosis in the early stages of pathology.
MRI reveals osteochondritis dissecans with separation of the osteochondral fragment from the talus.
Differential diagnosis of Koenig's disease
| Disease | Features |
| Chondromatosis | With chondromatosis, it is not possible to identify a typical “niche” in the epiphysis of the femur or tibia; the chondromic bodies have a “bean” shape, their number can reach 10 or more, while with Koenig’s osteochondropathy there is a single sequester. |
| Deforming osteoarthritis | Fragments of osteophytes and areas of ossification of ligaments can simulate intra-articular loose bodies, but they have an irregular shape and pointed edges. The condyle defect also cannot be detected. |
| Hoff's disease | With Hoff's disease, the structure of the infrapatellar or suprapatellar fat body changes, it becomes dense and can lead to symptoms of strangulation, just as with Koenig's osteochondropathy. With MRI and CT, it is possible to distinguish with a high degree of reliability a compacted fat body from an articular “mouse”; on radiographs, the main distinguishing feature will be the absence of a “niche”. |
| Intra-articular fracture | The joint “mouse” of a traumatic nature has an irregular shape and uneven edges. It is not possible to identify a typical “niche”. |
| Errors in interpreting normal joint anatomy | Sometimes an inexperienced doctor may mistake the sesamoid bone in the tendon of the gastrocnemius muscle - fabella - for an intra-articular free body on radiographs. The “niche” in the lateral condyle of the femur can be confused with the subchondral “light” zone, which is well defined in some patients - a variant of the normal anatomy of the joint. |
Treatment of osteochondrosis of the hip joint
Therapy takes months and even years. Treatment for osteochondrosis of the hip joint is selected according to the stage of the disease. Here we need an integrated approach that solves several problems at once: strengthening and improving blood flow to the affected area, regulating the quantity and quality of lubricating fluid, relieving pain, ensuring good tissue nutrition, normalizing metabolism and restoring cartilage. All this can be achieved through a combination of drugs, exercise therapy and other rehabilitation methods.
How to treat osteochondrosis in the hip joint?
- Medication.
- Physiotherapy.
- Therapeutic exercise.
- Massage.
Attention! In particularly severe cases, surgery may be required. It is the most risky and is not suitable for everyone.
Gymnastics for osteochondrosis of the hip joints
The exercises are aimed at relieving muscle stiffness, strengthening smooth muscles, and improving blood circulation. These are activities that will take no more than 20-30 minutes a day.
Features of exercise therapy:
- You cannot make sudden jerks.
- If pain occurs, you need to reduce the range of motion or stop the exercise.
- Repeat the movements no more than 10-15 times, start with a small number of repetitions.
Effective exercises for osteochondrosis of the hip joint:
- Lie on the bed and alternately rotate your legs. Raise your leg and rotate from side to side like a pendulum. Alternately stretch your feet towards the ceiling.
- Lying on the bed, bend your knees and leave your heels on the bed. Lower your left knee to your right foot, touch the bed, and then vice versa (right to left).
- Sit on a chair, legs together. Next, bend over and touch your toes to your feet, return to the starting position and repeat.
You can do gymnastics at home in the morning, before bed, or at any free minute.
Nutrition for osteochondrosis of the hip joint
Therapy necessarily includes changes in diet. It is very important to enrich the menu with protein, sulfur for collagen production, fatty acids, vitamins and other microelements. For example, salmon, sardines or mackerel can be a source of Omega 3, and eggs, legumes, cabbage, radishes and other vegetables can be sources of sulfur.
How do you recommend eating?
- Eat in small portions, but 5-6 times a day.
- Add cereals and legumes, as well as fermented milk products to your diet. For example, cottage cheese or kefir.
- Include vegetable salads in the menu.
- Minimize the amount of salt.
- Prepare dishes from lean meat. For example, you can use chicken breast or beef.
- Exclude fried, fatty, salty, canned food, sausages, semi-finished products, baked goods, alcoholic and carbonated drinks.
Doctors recommend adhering to the basic principles of proper nutrition, since the body needs a supply of high-quality nutrients to restore the joint capsule and, in particular, cartilage.
Physiotherapy for osteochondrosis of the hip joint
Physiotherapy in itself does not cure the disease; it is only an auxiliary method that speeds up the treatment of osteochondrosis of the hip joint and generally alleviates the condition. Electrophoresis improves cell regeneration and increases the conductivity of nerve impulses, magnetic therapy is used to relieve tension and start metabolic processes, and laser therapy is used to reduce inflammation.
Types of pathology
Chondropathy code according to ICD-10 is assigned M91-M94. The classification of the disease includes several forms, and each has its own characteristics of the course and causes of development.
Legg-Calvé-Perthes disease
Legg-Calvé-Perthes disease affects the head of the femur. It is most often diagnosed among boys aged 4 to 12 years. An injury can trigger the development of the disease.
At first there are no symptoms. Pain gradually appears and slowly descends to the knee joint. At rest, symptoms are practically absent, but after prolonged exercise they increase again.
On a note!
The child may not pay attention to the pain, but parents notice that the movements of the hip joint have become more limited.
Symptoms of this form of chondropathy also include muscle wasting in the hip joint. She becomes very thin and decreases in volume.
Keller's disease
There are two types of Keller's disease. The first type affects the navicular part of the foot. Either one or both limbs are involved in the process. Symptoms:
- Lameness,
- Trying to step on the outside of the foot
- Pain, especially at night,
- Swelling.
The second type of this form of pathology is diagnosed among girls aged 10 to 20 years. The symptom is pain in the area of the second and third toes. It gets worse when walking. To reduce the load, sick people try to step on their heels, which leads to the development of deforming arthrosis.
Osgood Schlatter disease
Osgood-Schlatter disease is a pathology that affects the tuberosity of the tibia. This leads to a necrotic process. The disease most often occurs in children under 18 years of age who engage in professional sports.
One of the symptoms is the formation of a lump that hurts when palpated. It is localized in the popliteal space.
Haglund's disease
Haglund Schintz disease is a type of chondropathy that causes a lump to form on the back of the heel. The disease is accompanied by the appearance of swelling and inflammation in the tendons.
The main symptom is pain, regardless of the level of activity. It occurs more often among teenage girls.
Symptoms of osteochondrosis of the hip joint
The disease develops slowly and gradually. In the first stages it does not cause discomfort, there is not even mild or severe pain. And only after a few months a person notices the first spasms and stiffness of movements. The pain cannot be called local - it can spread to the back, hips or groin area. Then you may experience swelling, numbness, aching, crunching and weakness in the legs. Of course, the set of symptoms of osteochondrosis of the hip joint depends on the severity and neglect of the disease:
- Stage 1.
Pain after exercise. For example, running or long walks. Goes away after rest. Using X-rays, it is difficult to identify signs of destruction of cartilage tissue. - Stage 2.
The pain becomes stronger and occurs even at rest. Lameness appears after strength training or heavy lifting. All destructive changes, including osteophytes, are clearly visible on x-rays. - Stage 3.
The patient regularly experiences pain and often uses a cane to walk. The muscles atrophy, the limb with the affected joint shortens. Surgery may be needed.
The disease is diagnosed by collecting complaints, external examination, neurological examination of reflexes and/or x-rays. In some cases, methods such as ultrasound, MRI and CT are used for diagnosis.