Shoulder pain can occur for various reasons - injury, joint pathology, bone damage, pinched nerve, etc. Some pathologies develop covertly, and the person experiences virtually no discomfort. Some diseases are accompanied by acute pain and limited movement. If, upon examination by a specialist, standard diagnostic techniques do not provide the necessary diagnostic information, the patient is prescribed magnetic resonance imaging of the shoulder joint.
This diagnostic method is based on the use of radio waves and magnetic fields. An MRI machine allows you to visualize the damaged area of the body, which makes it possible to establish an accurate diagnosis and proceed to effective treatment.
Operating principle
The basis of the method is an electromagnetic field in which a person is placed, given that every cell of the body contains hydrogen ions that have the ability to create a response impulse in response to the influence of electromagnetic fields. It is these impulses that are captured by the MRI machine, and based on these data it is possible to obtain a three-dimensional image of the object under study. Compared to other diagnostic methods that use X-rays, magnetic resonance imaging is safe for the human body.
Content:
- Operating principle
- What will an MRI of the shoulder joint show?
- Indications for MRI
- Preparing for the study
- Features of the procedure
- Application of a contrast enhancer
- Contraindications and restrictions
Scanning of a certain area of the body is carried out layer by layer. The thickness of the layer is determined by a specialist depending on the individual case and is only a few millimeters. Next, based on all the images received, a general information picture is formed and a conclusion is made.
Decoding
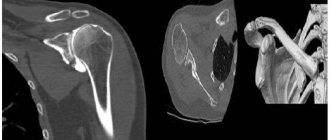
The radiation diagnostics doctor interprets the results obtained. Deciphering usually does not take more than 2 hours, but when the radiologist is busy, patients have to wait for results within 24 hours. What does an MRI of the shoulder joint show:
- inflammatory foci, destructive and degenerative changes in bones and hyaline cartilage are visualized as intensely colored areas;
- inflammation is indicated by cavities formed around the tissues;
- benign and malignant neoplasms look like areas with a denser structure. They are intensely colored and localized at the border between bones and muscles;
- when the ligaments rupture, there is a noticeable displacement of the torn parts into the articular cavity;
- overgrown edges of bone plates and calcified areas signal the irreversible destruction of cartilage tissue and the development of osteoarthritis;
- complete or partial fusion of the joint space indicates ankylosis (immobility of the joint) and the need for surgical intervention;
- the formation of sequestra (dead tissue) is a characteristic sign of infectious arthritis;
- the accumulation of fluid in the synovial bursa indicates bursitis, and the presence of effusion in the joint cavity indicates synovitis;
- changes in heat exchange, also determined during examination, accompany many diseases of the shoulder joint.
During interpretation of the results, the condition of the bone surfaces lined with cartilage tissue is assessed. Normally, there should be no obvious defects on them. Ligaments, tendons, nerve bundles, and muscle fibers located near the joint are also examined. Changes in soft tissue structures often indicate a low-grade inflammatory process.
What will an MRI of the shoulder joint show?
When a patient consults a doctor with complaints of pain in the shoulder joint or limited mobility, magnetic resonance imaging may be prescribed to clarify the diagnosis and find the true cause of the discomfort. A significant advantage of this method is that the image shows not only cartilage and bone tissue, but also blood vessels, tendons, ligaments and surrounding soft tissue. And a defect in any of these elements will be visible in the resulting layer-by-layer images.
Thus, traumatic injuries can be seen on MRI of the shoulder joint; pathologies and lesions of the periarticular bursa; presence of tumor and metastases; pathologies of muscles, ligaments or tendons; abnormalities of blood vessels, nerves and other defects.
At the same time, MRI can be used to monitor recovery dynamics – when the patient is recovering from a complex injury or surgery.
Benefits of diagnostics
According to statistics, magnetic resonance imaging of joints is prescribed much more often than ultrasound or radiography. This is due to the much higher information content of MRI.
The procedure has other advantages:
- The manipulation is non-invasive; it does not require anesthesia, incisions or punctures;
- The diagnostic process is not felt by the patient: it does not hurt or cause discomfort;
- The tomograph does not create radiation exposure, so the procedure is completely safe for your health. Magnetic resonance imaging of the shoulder joint can be done even several times a day, if necessary;
- Small list of contraindications;
- The study can even be carried out on pregnant women;
- The ability to detect destructive changes in bone and cartilage tissue, damage to the synovial capsule, ligaments, muscles, and nerve fibers.
Indications for MRI
Most often, elderly patients, athletes and people whose work activities involve constant physical activity complain of pain in the shoulder joint. But, according to statistics, at this time there is an increase in the number of complaints from young people and even children. The reason for this negative phenomenon lies in an unhealthy lifestyle, low activity, and unbalanced diet. Regardless of the cause of the discomfort - injury or the development of pathology - the patient may be prescribed magnetic resonance imaging. A referral for testing can be issued by a traumatologist, rheumatologist or attending physician.
Indications for issuing a referral for MRI:
- injuries, suspected damage or ligament rupture;
- acute or chronic shoulder pain;
- complete or partial loss of mobility;
- fracture or dislocation;
- suspicion of a tumor;
- chronic inflammatory diseases of the joints;
- degenerative diseases;
- rehabilitation period after injury or surgery.
Based on the MRI results, the attending physician can confirm a preliminary diagnosis or determine the cause of the patient’s complaints.
How is an MRI of the shoulder done?
- MRI
- Ultrasound
MRI tomograph:
Siemens Magnetom C
Type:
Open (expert class)
What's included in the price:
Diagnostics, interpretation of images, written report from a radiologist, recording of tomograms on CD + free consultation with a neurologist or orthopedist after an MRI of the spine or joint
Ultrasound machine
HITACHI HI VISION Avius
Class:
Expert (installation year 2019)
What's included in the price:
Diagnostics, interpretation of images, written diagnostic report
Preparation
During a tomography of the shoulder joint, the patient can wear his own clothes, as long as they do not have brooches, rivets, metal buttons, zippers or other fasteners. In some clinics in St. Petersburg, examinees are given special disposable underwear to minimize the possibility of metal elements getting into the magnetic resonance imaging scanner. The MRI procedure of the shoulder does not particularly regulate food intake, but in the case of MRI diagnostics with contrast, doctors recommend not eating food for several hours before this study. This will help avoid nausea and other unpleasant sensations when a contrast agent is administered. Contrast testing in people with kidney failure will require consultation with a primary care physician or nephrologist and possibly a blood test for creatinine. For young children, MRI examinations are sometimes performed under anesthesia or sedation. The tomography procedure requires the patient to remain completely still, and this is very difficult to achieve in children. If your child is scheduled for an MRI under anesthesia, preparation will include a series of tests, a consultation with a pediatrician or neurologist, and dietary restrictions before the test. As a preventive measure, women are not recommended to undergo tomographic diagnostics during pregnancy in the first trimester. People who are overweight or have large body dimensions should, when scheduling an MRI of the shoulder, clarify the weight and size restrictions that this tomograph model can handle. A closed-type tomograph in a person with phobias can cause a panic attack, so if you suffer from claustrophobia, you can take sedatives an hour before the diagnosis or choose an MRI of the shoulder joint on an open tomograph[/anchor].
Preparing for the study
Preparation for the scan includes dressing the patient in suitable clothing and removing all metal objects from the body, including removable dentures. If there are permanent metal implants in the body, you should definitely notify the specialist performing the diagnosis. The magnetic field can negatively affect dentures, displacing them from their intended place. This may also affect the outcome of the study.
The patient is certainly informed that he will be placed in a special tube of the device and will be in rather cramped conditions throughout the study. People suffering from claustrophobia or increased nervous excitability are prescribed sedatives. Sometimes claustrophobia makes it impossible to perform the procedure.
If magnetic resonance imaging is necessary for children under 5 years of age, general anesthesia may be used.
What does MRI of muscles and superficial structures show?
MRI makes it possible to detect changes in muscles and superficial structures caused by diseases, injuries and other causes, including developmental abnormalities, in the early stages, and to take adequate therapeutic measures in a timely manner.
At the same time, MRI allows you to detail the smallest structures such as individual muscle bundles, tendon fibers, etc.
Soft tissue MRI helps:
- identify the presence and location of the source of inflammation or infection;
- determine the presence of post-traumatic changes;
- identify neoplasms in soft tissues, etc.
Features of the procedure
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
The duration of the procedure is 20-30 minutes. The patient lies down on a special retractable couch. The head, legs and arms are fixed with special rollers or soft straps, and a special coil is attached to the area of study, with which images are obtained - to obtain an accurate result, it is necessary to remain motionless throughout the entire scanning process. The couch slides into the tube of the device and scanning begins.
The device produces a fairly loud sound during operation, which can cause panic attacks or neurasthenia. If there is a sharp deterioration in the patient’s condition, the patient can contact the x-ray technician via two-way communication.
Deciphering the results takes from 30 minutes to several hours, depending on the specific case. The description is made by a radiologist and issued in the form of a preliminary report. The final diagnosis is determined by the attending physician.
Who is prescribed MRI of soft tissues?
MRI of superficial structures and muscles may be recommended for diseases and conditions such as:
- severe pain;
- edema, swelling of tissues;
- vascular disorders;
- traumatic damage to muscles, tendons, subcutaneous fat, etc.;
- pinched nerve fibers;
- suspicion of the presence of neoplasms;
- suspicion of inflammatory or infectious processes;
- preoperative or postoperative examination;
- atrophic, dystrophic and other degenerative changes, etc.
1 MRI of muscles
2 MRI muscles
3 Muscle MRI
Types of MRI of muscles and superficial structures
MRI of neck muscles
It is one of the most complex types of MRI scanning, since in a relatively small area of this part of the body organs belonging to different systems are closely adjacent: nervous, lymphatic, endocrine, circulatory, digestive.
Using the phenomenon of magnetic nuclear resonance, it is possible to track pathological changes in the thyroid gland, lymph nodes, larynx and salivary glands.
An MRI of the neck is usually recommended if pain and inflammation occur, if there is injury or if a tumor is suspected. A scan may be ordered in the following cases:
- tracking changes in lymph nodes;
- detection of tumors in the neck area;
- diagnosis of thyroid pathologies;
- identification of pathologies of the vocal cords;
- diagnosis of cerebral circulatory disorders;
- detection of formation of parathyroid glands, etc.
MRI of soft tissues of the lower extremities
This study (patients often call it MRI of the leg muscles, MRI of the thigh muscles) helps to identify inflammatory, tumor processes, connective tissue diseases, and also establish the presence of fluid in the joints.
With the advent of MRI scanning, invasive diagnostic techniques such as biopsy and intraosseous pressure measurement have a painless alternative. At the same time, the reliability of the MRI result, which allows one to distinguish healthy tissue from inflamed tissue, is 95%.
If the patient wishes and as prescribed by the doctor, additional studies can be done - MRI of the gastrocnemius muscle and MRI of the piriformis muscle.
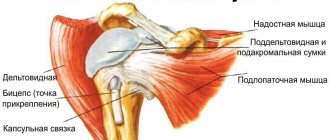
MRI of soft tissues of the shoulder
This type of MRI allows you to determine the cause of limited movement and pain in the joints of the upper extremities.
Based on the diagnostic results, the MRI doctor will determine the presence of vascular pathology, inflammation or damage to muscles and tendons, and other problems in the soft tissues of the shoulder.
MRI of soft tissues of the upper and lower extremities may be recommended in cases such as:
- developmental anomalies;
- post-traumatic injuries;
- limited motor activity of the limbs;
- pain and swelling of tissues;
- hemorrhages, hematomas;
- ruptures and damage to muscles and tendons;
- abscesses, phlegmons, infiltrates in soft tissues;
- inflammatory processes;
- myositis, etc.
1 MRI of soft tissues
2 MRI of soft tissues of the lower extremities
3 MRI of soft tissues